AACN Beacon Award for - American Association of Critical
advertisement

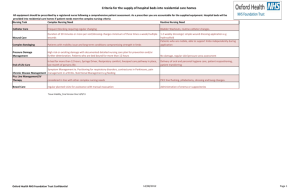
1 AACN Beacon Award for Excellence Application Example 2 Introduction This mock application provides you and your unit examples of criteria question responses. This information is provided solely as a reference to assist you as you develop your application. The responses included in this illustration do represent typical responses from a unit that has received a Beacon Award, but do not necessarily represent responses from a Gold-level unit. If you have additional questions please feel free to email beacon@aacn.org. Unit Profile The Unit Profile describes the framework within which your unit functions. The Unit Profile should identify the key characteristics of your unit including the environment of care and relationships with other units, patients, families and stakeholders. Information from the Unit Profile helps reviewers better understand the composition and structure of your unit and facility. You do not need to include detailed information about your processes or outcomes in the Unit Profile. You will have an opportunity to provide that information when answering the criteria questions in Categories 1-5. The Unit Profile is not scored. Criteria Questions Describe the type of facility the unit works within. How many beds are in the hospital and unit? 1 Response The University Hospital is a fully accredited, acute-care, 506-bed, not-for-profit community hospital that serves more than 440,000 people in Jones County and adjoining communities. There are 4 separate critical care units totaling 46 critical care beds with 10 designated Intensive Care Unit (ICU) beds. University Hospital has received the Gold Seal of Approval from the Joint Commission along with the following notable designations: • Magnet designation for Nursing Excellence since 2006 • J.D. Power and Associates Distinguished Hospital Program Award for Outstanding Inpatient and Emergency Department Care • 10 Joint Commission Gold Seals for Cardiac, Cancer, Joint Replacement and Stroke Care • Named by HealthGrades as one of America’s 100 Best Hospitals for Cardiac Care, Cardiac Surgery, Coronary Intervention, Orthopedic Surgery, Joint Replacement, and Gastrointestinal Care • Designation as a Top Hospital by the Leapfrog Group. University Hospital was one of only 65 hospitals in the country to make the list. 8 Describe the structure for unit governance and decision making including how decisions affecting operations are made. Notes: Examples may include top-down leadership or unit-based councils. Response Two councils (Resource & Innovation and Practice & Professional Development) comprise our unit’s 3 Shared Nursing Leadership. These councils provide an opportunity for staff nurses to participate in decision making that will impact the unit, create innovative programs, provide evidence-based practice recommendations and facilitate the professional development of direct care staff. Each council is cochaired by a staff RN and a member of nursing leadership. Leadership relies upon the direct care nurses input regarding practice changes, addressing workplace satisfaction and streamlining workflow. Suggestions or recommendations from the Councils are presented to the Care Delivery and Nursing Leadership teams for discussion and review. The councils meet monthly and are open to new membership. Many of the unit leaders are involved in the unit wide multi-disciplinary Care Delivery Team and the Critical Care Committee. This committee includes Pediatric ICU and Cardiac ICU leadership who work together to standardize care across the critical care areas. The most recent project includes a Daily Goals Sheet completed by the team during rounds and utilized for hand-off and communication between providers and shifts. This is now a standard part of daily rounds utilized in each of the intensive care units. Information from the Critical Care Committee is shared amongst the unit-based Care Delivery Teams and Shared Nursing Leadership Councils and then communicated to staff via email, education newsletters and staff meetings. Category 1: Leadership Structures and Systems – 150 Points Unit leaders are integral to ensuring a healthy work environment that focuses on the delivery of the best care for patients and families. On the unit, the best care may be reflected in a commitment to systematically develop and train nurse leaders; ensure accountability; advocate and participate in decision making; and provide meaningful recognition to staff. Creating a sustainable healthy work environment can improve the care delivery environment, thereby improving clinical outcomes, patient and family satisfaction, and staff satisfaction and retention. The criteria questions in this category are aimed at soliciting information about how your unit leaders support and maintain a healthy work environment. For each question reviewers will evaluate the comprehensiveness of your approach; application and integration across staff and key stakeholders; and evidence of continued evaluation, shared learning and process improvement. Criteria Questions 1 For unit leaders identified in the Unit Profile: a. Describe how they are trained to meet and maintain the responsibilities of their role. For example, how are unit leaders held accountable by managers, staff or interdisciplinary stakeholders? b. Describe how unit leaders guarantee joint accountability between medical, nursing and other leaders. c. Describe how this group works together to ensure integration of patient care within and outside of the unit. Notes: Unit leaders are defined as anyone who has daily responsibility for unit function and may include managers, supervisors, charge nurses or directors. This may also include physicians and other nonnursing personnel. Some examples of accountability may include formal processes such as peer review, performance evaluation and/or performance against measurements and goals; it may also include informal feedback mechanisms or surveys. Integration of patient care includes the processes and systems used to ensure sustained quality of care between your unit and supporting units (such as dialysis or 4 radiology) and/or outpatient care settings (such as clinics, offices and rehabilitation facilities). Response Formal orientation and continuing education programs for leadership positions vary based on the role. New managers are partnered with and mentored by more experienced leaders. A Management Development Series of workshops provides new leaders with skill building and management training on subjects such as personnel management, dealing with difficult employees, providing positive customer service, managing priorities, and creating a respectful workplace. The Nursing Leadership Luncheon Series is also available where a variety of monthly topics are presented by hospital subject matter experts. Critical care nursing leadership attends a weekly mentoring and collaboration meeting that is facilitated by the Vice President of Cardiovascular and Critical Care Services. All nurse directors, nurse managers and clinical coordinators from the cardiovascular and critical care areas assemble to discuss leadership challenges, present case studies or share successes with their peers. This long-standing meeting is very well received by critical care nursing leadership. One nurse manager stated, “As a manager, whether novice or experienced, you face different and often difficult challenges in your role. This group has helped me problem solve and develop strategies to deal with specific situations related to practice and/or staffing issues.” In addition, this past year a Nursing Administration Journal Club was implemented. This journal club provides a forum for vigorous discussion on topics pertinent to current clinical issues. Participation includes nursing administrators, nurses with advanced degrees and nurse scientists. Each month a designated nursing leader selects a pertinent article to review. The meeting follows a set format for research article critique. Our unit administration functions with joint accountability. The frontline leaders meet with the Nursing Director and Critical Care Director on a bi-weekly basis to discuss what is working well in the unit and to identify areas of improvement. Together, they align their goals with the goals of the institution and are responsible for the “cascading” of goals from CEO to associate level. Information sharing is done at these meetings and recognition of unit “wins” is done. These directors are easily accessible, maintain an open door policy and promote autonomy within the nursing profession. The Unit Medical Director, who is also the director of trauma services, takes an active role by meeting with frontline leaders on a monthly basis. He will also meet informally as needed. He is instrumental in assisting staff nurses with the implementation of evidence-based practices to the bedside. He makes it a point to include each bedside nurse (who he knows by name) in rounds and values their input. He works collaboratively with the APN, unit director and frontline leaders on unit incentives and projects. With his guidance, we have instituted ICU specific glycemic standing orders, electrolyte standing orders and venous thromboembolism assessment and guidelines have been restructured and order sets have been developed. He works collaboratively with the APN to track duration of indwelling urinary catheters, as well as, centrally accessed lines. He shares findings with nursing, as well as, the medical staff including residents and students. Category 3: Effective Communication, Knowledge Management, Learning and Development – 100 Points Skilled communication is an important component of a healthy work environment and supports true collaboration to provide quality patient-centered care. Continued growth and development through education and training in the ever-changing field of healthcare can improve outcomes and satisfaction. The criteria questions in this category are aimed at soliciting information about how your unit ensures effective communication among all staff that provide care; staff competency among those who provide care; and manages and encourages knowledge sharing. For each question reviewers will evaluate the 5 comprehensiveness of your approach; application and integration across staff and key stakeholders; and evidence of continued evaluation, shared learning and process improvement. Criteria Questions: Effective Communication 2 Describe how all staff and key stakeholders effectively communicate and collaborate for optimal patient care. Notes: Examples of stakeholder communication processes may include interdisciplinary care teams, plans of care or daily goal sheets. Response Unit leaders ensure effective communication between team members and all key stakeholders through formal and informal methods. The nurses, respiratory therapists and physicians round on the patients three times in a 24-hour period using the situation, background, assessment and recommendation (SBAR) format. Patients and families are encouraged to participate in daily rounds. The nurse presentation during rounds plays a primary role. This allows the team to get a quick overview on sedation/pain medication requirements in the previous 24 hours, existing lines, insertion dates and necessity for vascular access and tubes such as foley catheters. This information is imperative to reduce the number of blood stream and urinary tract infections in the unit. By rounding three times daily, plans are re-evaluated and changes to care are initiated without delay. Goals identified for the day are posted on patient communication boards for patients, families and health care team members. Cardiac and trauma surgery rounds are conducted daily on their respective patients; once again nurses present at these patient care rounds. The ICU team conducts multi-disciplinary rounds weekly on all patients. The multi-disciplinary team consists of the patient, families, patient’s nurse, intensivists, residents, social work, respiratory therapist, pharmacist, child life specialist, nutritionist and unit leaders. The bedside nurse is asked for their input on the patient as in daily rounding. This allows for open communication amongst all stakeholders and thus an optimal plan of care can be developed for each patient. This is yet another opportunity for the bedside nurse to have input on patient care. Effective communication and collaboration also include safety huddles conducted prior to each shift. This information is a combination of hospital and unit updates, concerns and upcoming events. The safety huddle information is also posted and available for staff review throughout the shift. A member of management attends shift briefing in order to answer any questions or concerns raised by staff. Additional learning is shared via storyboards, emails and ICU newsletters. Monthly staff meetings are conducted with all staff members in attendance. If unable to attend, conference calling is available to staff at home, and minutes are posted in a designated notebook for review and initialing. Monthly internal quality improvement meetings with trauma and cardiac services as well as general medicine services, help the ICU identify areas of concern and improvement in efforts to optimize patient outcome. Category 5: Outcome Measurement – 450 Points This category focuses on the results achieved from your objective evaluation and patients/ family evaluations of the unit’s performance. Through measuring your progress, you can assess and improve processes related to clinical, staff, patient and family outcomes. For each question, reviewers will evaluate the data presented. Specifically, they are evaluating your current performance levels1, trends over time2, and results against comparable benchmarks3. Although there are no requirements for the reporting time frame or amount of data you present, keep in mind that your results are used for performance management of your unit. Therefore, the measures you 6 select to include should support decision making in a rapidly changing environment, and the measurement intervals should be appropriate for effective, timely, data-based decision making. Notes: 1. Levels reflect numerical information that places or positions a unit’s results and performance on a meaningful measurement scale. 2. Trends are numerical information that shows the direction and rate of change. A statistically valid trend generally requires a minimum of three historical data points. 3. Comparisons are data points to evaluate a unit’s outcomes against similar external outcomes. Comparisons might include other units, overall facility, regulatory requirements, external benchmarks or relevant nationally recognized standards. Some examples of recognized standards may include National Database for Nursing Quality Indicators (NDNQI), National Quality Forum (NQF) or National Association of Children’s Hospitals and Related Institutions (NACHRI). Criteria Questions 3 Summarize your unit’s key patient safety and clinical outcomes results. What are your current levels and trends in key measures of: a. Medication safety? b. Hospital-acquired conditions? c. Serious reportable events? How do these results compare with the performance of similar units? Notes: Outcomes included in this section should reflect your specific unit patient population and scope of service; at a minimum those measures required in regulatory reporting requirements should be included. See additional notes in the Beacon Program Handbook under Category 5: Outcome Measurement. Response Catheter-Associated Urinary Tract Infection (CAUTI) Our ICU’s rate of CAUTIs for the last 12 months is 0.66 per 1000 device days, and our last CAUTI occurred in December 2010. We benchmark our rates with the National Healthcare Safety Network (NHSN) within the CDC. Their current benchmark rate is 3.4 per 1000 device days for a “Medical/Surgical Major Teaching Hospital,” so we are well below the national average (Figure 28). In an effort to maintain/decrease this low rate, our ICU follows CDC guidelines. Indwelling urinary catheters are placed using aseptic technique only by RNs and only when deemed medically necessary. We understand that avoiding an unnecessary indwelling catheter is the best way to decrease nosocomial CAUTIs. Catheters are removed as soon as they are no longer medically indicated. After placement, a closed system is maintained with few exceptions. If catheter irrigation or specimen collection is required, strict aseptic technique is used. Urine collection bags are kept below the level of the 7 bladder at all times. While the indwelling catheter is in place, the RN performs an assessment every 12 hours including a visual inspection of the meatus and urine color and clarity. Abnormalities are noted. Documentation includes catheter placement date and size. Routine catheter care using soap and water is performed at least every 12 hours. Our ICU team avoids potentially harmful practices such as routine irrigation or regularly scheduled catheter changes. The RN staff utilizes a bladder scanner to avoid unnecessary catheterizations. In 2009, one ICU staff RN became our champion for CAUTI prevention and review and implementation of evidence-based practices. She has co-authored and updated the hospital-wide procedure for indwelling catheter insertion and CAUTI prevention and presented didactic information for all ICU RNs. Currently, she is working on acquiring new catheter securement devices and publishing a patient education brochure on CAUTI prevention. As a member of the CAUTI team she works to implement the bundle, simplifying prevention. The bundle will roll out later this year and will include: Provider order Indications for indwelling catheter Alternatives to consider Aseptic Insertion Securing device Daily assessment for removal of catheter when no longer indicated Another performance improvement activity for CAUTI prevention was launched in 2010. The creation of order sets was targeted to help providers consider indications for indwelling catheters and monitor for continued need. The order sets encourage critical thinking by providers for all patients with indwelling catheters. If the catheter is still indicated two days after the order is placed for a post-operative patient, the provider must renew the order daily.