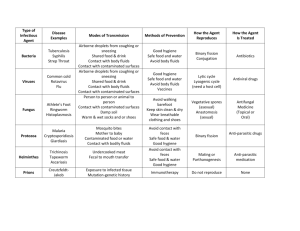
Identification
advertisement

SALMONELLA TYPHI / SHIGELLA / E. COLI / HEPATITIS A VIRUS SALMONELLOSIS Identification A bacterial disease commonly manifested by an acute enterocolitis, with sudden onset of headache, abdominal pain, diarrhea, nausea and sometimes vomiting. Dehydration, especially among infants or in the elderly, may be severe. Fever is almost always present. Anorexia and diarrhea often persist for several days. Deaths are uncommon, except in the very young, the very old, the debilitated and the immunosuppressed. Occurrence Salmonellosis is classified as a foodborne disease because contaminated food, mainly of animal origin, is the predominant mode of transmission. The incidence rate of infection is highest in infants and young children. Epidemiologically, Salmonella gastroenteritis may occur in small outbreaks in the general population. About 60-80% of all cases occur sporadically; however, large outbreaks in hospital, institutions for children, restaurants and nursing homes are not uncommon and usually arise from food contaminated at its source, or less often, during handling by an ill person or a carrier, but person to person spread can occur. Mode of transmission By ingestion of the organisms in food derived from infected animals or contaminated by feces of an infected animal or person. This includes raw and undercooked eggs and egg products, raw milk and raw milk products, contaminated water, meat and meat products, poultry and poultry products. In addition, turtles, iguanas and chick, and unsterilized pharmaceuticals of animal origin are potential sources of these bacteria. Recently, several outbreaks of salmonellosis have been traced to consumption o f raw fruits and vegetables that were contaminated during slicing. Fecal-oral transmission from person to person is important, especially when diarrhea is present; infants and stool incontinent adults pose a greater risk of transmission than do asymptomatic carriers. Epidemics are usually traced to foods such as processed meat products, inadequately cooked poultry and poultry products; uncooked or lightly cooked foods containing eggs and egg products, raw milk and dairy products, including dried milk; and foods contaminated with feces by an infected food handler. Epidemics may also be traced to foods such as meat and poultry products that have been processed or prepared with contaminated utensils or on work surfaces or tables contaminated in previous use. Methods of Control Educated food handlers and preparers about the importance of a) handwashing before, during and after food preparation; b) refrigerating prepared foods in small containers; c) thoroughly cooking all foodstuffs derived from animal sources, particularly poultry, pork, egg products and meat dishes; d) avoiding recontamination within the kitchen after cooking is completed; and e) maintaining a sanitary kitchen and protecting prepared foods against rodent and insect contamination. Page 1 of 4 Educate the public to avoid consuming raw or incompletely cooked eggs, as in eggs cooked “over easy” or “sunny side up,” in eggnogs or homemade ice cream, and using dirty of cracked eggs. Pasteurized or irradiated egg products should be used to prepare dishes in which eggs would otherwise be pooled before cooking or when the dish containing eggs is not subsequently cooked. Exclude individuals with diarrhea from food handling and from care of hospitalized patients, the elderly and children. Indoctrinate known carriers on the need for very careful handwashing after defecating (and before handling food) and discourage them from handling food for others as long as they shed organisms. Recognize the risk of salmonella infections in pets. Chicks, duckling and turtles are particularly dangerous pets for small children. SHIGELLA Identification An acute bacterial disease involving the large and distal small intestine and characterized by diarrhea accompanied by fever, nausea and sometimes toxemia, vomiting, cramps and tenesmus. In typical cases, the stools contain blood and mucus (dysentery) resulting from mucosal ulcerations and confluent colonic crypt microabscesses caused by diarrhea. Convulsions may be an important complication in young children. Bacteremia is uncommon. Mild and asymptomatic infections occur. Illness is usually self-limited, lasting an average of 4-7 days. Occurrence Worldwide; it is estimated that shigellosis causes about 600,000 deaths per year in the world. Two thirds of the cases, and most of the deaths, are in children under 10 years of age. Illness in infants under 6 months is unusual. Outbreaks commonly occur under conditions of crowding and where personal hygiene is poor, such as in jails, institutions for children, day care centers, mental hospitals and crowded refugee camps. Shigellosis is endemic in both tropical and temperate climates; reported cases represent only a small proportion of cases, even in developed areas. Mode of transmission Mainly by direct or indirect fecal oral transmission from a symptomatic patient or a short term asymptomatic carrier. Infection may occur after the ingestion of very few (10-100) organisms. Individuals primarily responsible for transmission are those who fail to clean hands and under fingernails thoroughly after defecation. They may then spread infection to others directly by physical contact or indirectly by contaminating food. Water and milk transmission may occur as the result of direct fecal contamination; flies can transfer organisms from latrines to uncovered food items. Methods of Control An organized effort to promote careful handwashing with soap and water is the single most important control measure to decrease transmission rates in most settings. Page 2 of 4 ENTEROHEMORRHAGIC E. COLI (EHEC) Identification This category of diarrheogenic E. coli was recognized in 1982 when an outbreak of hemorrhagic colitis occurred in the USA and was shown to be due to an unusual serotype, E. coli O157:H7, that had not previously been incriminated as an enteric pathogen. The diarrhea may range from mild and nonbloody to stools that are virtually all blood but contain no fecal leukocytes. The most feared clinical manifestations of EHEC infection are the hemolytic uremic syndrome (HUS) and thrombotic thrombocytopenic purpura (TTP). Approximately 2-7% of subjects who manifest EHEC diarrhea progress to develop HUS. EHEC elaborate potent cytotoxins called Shiga toxins 1 and 2. Shiga toxin 1 is identical to Shiga toxin elaborated by Shigella dysenteriae 1; notably, HUS is also a well recognized severe complication of S. dysenteriae 1 disease. Occurrence These infections are now recognized to be an important problem in North America, Europe, South Africa, Japan, the southern cone of South America and Australia. Serious outbreaks, including cases of hemorrhagic colitis, HUS, and some deaths, have occurred in the USA from inadequately cooked hamburgers, unpasteurized milk, apple cider (made from apple that were probably contaminated by cow manure) and alfalfa sprouts. Mode of transmission Transmission occurs mainly by ingestion of contaminated food; as with salmonella, it is most often due to inadequately cooked beef (especially ground beef) and also raw milk and fruit or vegetables contaminated with ruminant feces. As with Shigella, transmission also occurs directly from person to person, in families, child care centers and custodial institutions. Waterborne transmission has also been documented; one outbreak was associated with swimming in a crowed lake and one was caused by drinking contaminated unchlorinated municipal water. Methods of Control Heat beef adequately during cooking, especially ground beef. The 2002 Oregon Food Sanitation Rules states to cook ground beef to an internal temperature of 155 F for at least 15 seconds. Reliance on cooking until all pink color is gone is not as reliable as using a meat thermometer. Protect, purify and chlorinate public water supplies; chlorinate swimming pools. Ensure adequate hygiene in childcare centers, especially frequent handwashing with soap and water. Outbreaks Linked to Restaurants or Public Gatherings Likely sources include undercooked meat, cross-contaminated food, or possibly food contaminated by an infected food handler. Any investigation should focus on implicating specific food items and evaluating their method of preparation. Ask about recent illness among food handlers. Page 3 of 4 HEPATITIS A VIRUS (HAV) Identification Onset of illness in adults in nonendemic areas is usually abrupt with fever, malaise, anorexia, nausea and abdominal discomfort, followed within a few days by jaundice. In general, severity of illness increases with age, but complete recovery without sequelae or recurrences is the rule. Generally, hepatitis A is considered a disease with a relatively low case-fatality rate. Occurrence In developed countries, disease transmission is frequent among household and sexual contacts of acute cases, and also occurs sporadically in day care centers with diapered children, among travelers to countries where the disease is endemic, among injecting drug users and among men who have sex with men. Where environmental sanitation is poor, infection is common and occurs at an early age. In the USA, 33% of the general population has serologic evidence of prior HAV infection. Mode of transmission Person to person by the fecal-oral route. The infectious agent is found in feces, reaches peak levels the week or two before onset of symptoms and diminishes rapidly after liver dysfunction or symptoms appear, which is concurrent with the appearance of circulating antibodies to HAV. Common source outbreaks have been related to contaminated water; food contaminated by infected food handlers, including foods that are not cooked or are handled after cooking; raw or undercooked molluscs harvested from contaminated waters; and contaminated produce such as lettuce and strawberries. A number of outbreaks in the USA and Europe have been associated with injecting and noninjecting drug use. Methods of Control Educate the public about good sanitation and personal hygiene, with special emphasis on careful handwashing and sanitary disposal of feces. Provide proper water treatment and distribution systems and sewage disposal. Management of day care centers should stress measures to minimize the possibility of fecal-oral transmissions, including thorough handwashing after every diaper change and before eating. Oysters, clams and other shellfish from contaminated areas should be heated to a temperature of 185 F – 194 F for 4 minutes or steamed for 90 seconds before eating. Page 4 of 4