Colorimetric End-Point Determination
advertisement

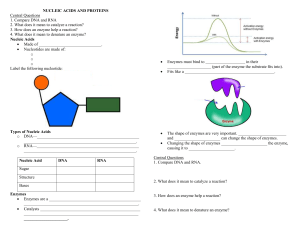
UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) 17enz1.wpd Task Colorimetric, end-point determination of Amylase, Lipase, and Transaminase enzymes. Objectives Upon completion of this exercise, the student will be able to: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Define enzyme and isoenzyme. List three general conditions under which cytoplasmic enzymes diffuse into the plasma. Compare/contrast fixed time and kinetic methods of enzyme assay. Identify the substrates acted upon and products produced by enzymes. Correlate disease states with enzyme levels. Identify and state the purpose of the reagents used in the procedures. Correlate the new and old names of the transaminase enzymes. State normal values of the enzymes. Write the reactions catalyzed by SGOT and SGPT respectively. Perform amylase, lipase, and transaminase enzyme procedures as instructed. Supplies and Equipment 1. 2. 3. 4. 5. 6. 7. 37 C water bath Timer Pipetts Alanine KG substrate Calibration solution NaOH, 0.4N Color reagent References Kaplan, Alex, Clinical Chemistry, & Sigma produce inserts Enzyme activity At normal body temperature, cellular chemical reactions, particularly those for the oxidation or transformation of organic compounds would occur very slowly. While raising the temperature would increase the speed of the reaction, living cells cannot be subjected to high temperatures because of the delicate nature of protoplasm. Biological systems, however, developed a number of catalysts that enable the necessary metabolic reactions to occur at body temperature. Enzymes are the functional proteins that catalyze biological reactions. Enzyme catalysts are not used up in the process and do not change the equilibrium point of the reaction; they merely accelerate the rate for reaching equilibrium. The velocity of enzyme reactions is affected by a variety of factors including: concentration of reactants, pH, temperature, ionic strength, and presence of inhibitors. Essentially, any substance that alters the configuration of an enzyme affects its activity. Refer to lecture notes and textbook reading assignment for description of enzyme inhibition/inhibitors. Enzymes are present in all body cells. Enzymes catalyze all essential reactions: oxidation, reduction, hydrolysis, esterification, synthesis, and molecular interconversions necessary for vital activities. MLAB 2401 - Cllinical Chemistry Lab Manual ! 145 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Enzymes are also found in low concentration in body fluids. They may be plasma specific enzymes or non-plasma specific enzymes which have no known physiological function in the plasma. While some of these enzymes are secreted, others come from the disintegration of cells during the normal process of breakdown and replacement. Certain enzymes appear in body fluids in much higher concentration following injury or death of tissue cells. In addition, altered membrane permeability that may occur with inflammation may be sufficient to permit the diffusion of cytoplasmic enzymes from cells into body fluids. Serum is the usual fluid taken for enzyme measurement for diagnostic purposes, but other body fluids may be chosen under appropriate circumstances. The concentration of an enzyme in plasma or serum cannot be measured readily in terms of ug per liter because it is difficult to determine in a direct manner the mass of a specific enzyme per unit volume of fluid. Instead, the rate at which the enzyme catalyzes a reaction with a substrate is measured under specific conditions. The activity of an enzyme may be measured by two different approaches: fixed time (two-point assay) and continuous monitoring (Kinetic assay). Two-point Assays The first enzyme tests commonly employed in the clinical laboratory (amylase, lipase, alkaline and acid phosphatase) utilized a fixed time for the reaction and expressed the enzyme activity as the amount of substrate transformed by a specified volume of serum under the particular conditions of the test. Often incubation times were long (24 hours in the lipase method of Cherry and Crandall, and 1 hour in the alkaline phosphatase method of Bodansky). As a consequence, there was some enzyme inactivation (partial denaturation), product inhibition, and suboptimal concentration of substrate after a time. The rate of enzyme activity decreased with time after an early period of linearity. Enzyme results from fixed time/two-point assay procedures are reported in units devised by the person who developed or was given credit for the procedure. The units often bear the early researcher's name (Cherry Crandall units, Bodansky units, etc.). The greater stability and sensitivity of modern spectrophotometers have improved the performance of two-point assays by making shorter incubation times possible. In such systems, however, it is necessary to establish the limits of enzyme activity in which zero order kinetics are followed. Preliminary experiments with different time intervals and with various aliquots of serum sample are essential for the selection of the conditions that produce linearity. Kinetic Assays In the kinetic assay, approach to enzyme measurement, enzyme concentration is determined through the observation of the enzyme's rate of activity over a short period of time. Three ways have been utilized to measure enzyme rate (decrease in substrate, increase in product, or a change in cofactor). Because the reaction time is usually short, there is little danger of enzyme inactivation. Furthermore, continuous monitoring permits multiple readings for the determination of the rate. If during the multiple readings a decrease in enzyme reaction rate is noted, the technician should suspect high enzyme activity causing substrate depletion. Continuous monitoring is used most commonly with those enzymes in which changes in NADH or NADPH are measured but can also be used for the determination of other enzyme activities (e.g., alkaline phosphatase) if a colored product is generated from a non-colored substrate. 146 ! MLAB 2401 - Clinical Chemistry Lab Manual UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Although a few enzyme tests have been employed in the clinical laboratories for more than 50 years, the past 25 years have seen a tremendous increase in their use and scope. The discovery by LaDue, Wroblewski, and Karmen in 1954 that the serum glutamic-oxaloacetic transaminase, or SGOT (now called aspartate aminotransferase, AST), activity in serum was increased within 24 hours after a myocardial infarct, initiated the modern era of clinical enzymology. Many different enzymes were investigated in an attempt to find early indicators of specific tissue injury. The serum patterns of several different enzymes that are obtained after a suspected organ injury are usually more revealing than the activity of a single enzyme; this finding has led to the multiplicity of enzyme tests. A further refinement in clinical enzymology has been the measurement of the different isoenzymes of a particular enzyme. Some enzymes exist in multimolecular forms (isoenzymes) that have similar catalytic activity but different biochemical and immunologic properties; they can be separated and identified by electrophoresis, by difference in absorption properties, or by reaction with specific antibodies. Refer to lecture notes and textbook reading assignment for further description of isoenzymes. Enzyme results are expressed in International Units (IU). The International Unit is defined as the amount of enzyme which converts 1 micromole substrate per minute under conditions. Temperature and method must be stated. Procedure I Amylase Determination Purpose Amylases are secreted by the salivary and pancreatic glands into their respective juices, which enter the gastrointestinal tract. These enzymes are important for the digestion of ingested starches. The amylase that is normally present in serum is derived from both pancreas and salivary glands. The activity of serum amylase rises following an obstruction to the flow of fluid from either the salivary or pancreatic glands. Acute pancreatitis is caused by blockage of the pancreatic ducts or by direct injury to the pancreatic tissue by toxins, inflammation, trauma, or by impaired blood flow. Serum amylase activity is raised considerably in acute pancreatitis, obstruction of the pancreatic ducts, and mildly in obstruction of the parotid (salivary) gland. The rise in serum amylase activity after obstruction of the pancreatic ducts is rapid and temporary. It usually reaches a maximum value from 6 to 10 times upper limits of normal (ULN) in about 24 hours and returns to normal in two or three days. Amylase is excreted through the kidneys. Unlike other enzymes, amylase is frequently detected and measured in urine specimens. A decreased concentration of serum amylase may be found in acute or chronic hepatocellular damage, but this is not a sensitive liver function test. Methods of Measurement Approaches used to measure the amylase enzyme: Amyloclastic measures the disappearance of the starch substrate. Saccharogenic measures the appearance of the carbohydrate products MLAB 2401 - Cllinical Chemistry Lab Manual ! 147 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Chromogenic - the enzyme=s activity on the starch-dye coupled substrate results in increasing color formation proportional to enzyme=s concentration. Kinetic / enzymatic continuous-monitoring - coupled enzyme reactions Principle Amylase is an enzyme that hydrolyses starch to oligosaccharides and eventually to maltose and glucose. Measurement of the time required for serum to hydrolyze starch in a carefully standardized substrate solution is a quantitative expression of the amylase activity. Starch (blue with iodine) Amylase > Oligosaccharides Amylase > (red with iodine) Maltose Glucose The endpoint is determined by removing portions of serum-starch mixture at timed intervals and adding them to iodine solution. As long as starch is present, a purplish color will develop. As the incubation proceeds, the color will change from blue to blue-purple, to red-purple, and finally to reddish-brown. This is the endpoint. Steps: Although this test is sound, new products using kinetic reactions are more popular. At this time, this product is not available. The steps have been condensed to give you an overview of how the test is performed. 1. Pre-incubate an aliquot of iodine solution to 37C. 2. Into tubes labeled control, patient 1, etc., place 2 mL of starch substrate. (The starch substrate must be aseptically drawn from the stock bottle.) 3. Warm test tubes at 37C for 5 minutes. 4. Testing one specimen at a time, add 0.5 mL serum or control to its appropriately labeled starch tube. Mix, return to water bath, and start time. 5. After 3 minutes, remove 0.1 mL of the serum-starch mixture and add it to the bottom of a small (10 x 75 mm) tube containing 0.1 mL of the iodine solution. Mix and observe color. The objective is to determine the number of minutes required to convert all of the starch to sugars. 6. If the color is purple, the endpoint has not been reached. Wait another 2 minutes and withdraw another 0.1 mL from the serum-starch mixture. Record the elapsed time. Add this 0.1 mL to a second tube of iodine solution and note the color. Continue incubation for more intervals until addition of serum-starch results in reddish-brown endpoint. Record total elapsed time in minutes to reach endpoint. Calculations: Serum amylase 1800 (Somogyi Units/dl) Endpoint time (minutes) Expected Values: Serum: 38-200 Somogyi Units/dL Procedure II Lipase Determination 148 ! MLAB 2401 - Clinical Chemistry Lab Manual UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Purpose Lipase measurements are used in the diagnosis and monitoring of various diseases of the pancreas such as acute pancreatitis and obstruction of the pancreatic duct. While the amylase test is more sensitive to pancreatic damage/disruption, lipase is considered to be more specific. Principle Pancreatic lipase catalyzes the two-step hydrolyses of triglycerides to diglycerides followed by the somewhat slower formation of monoglycerides Triolein H2O lipase Diglyceride H2O > diglyceride fatty acid lipase > monoglyceride fatty acid The decrease turbidity of a triolein suspension can be measured in the ultraviolet range. The rate of turbidity decrease is a measure of lipase activity. Specimen Non-hemolyzed serum or heparinized plasma Procedure III Transaminases Purpose The transaminases function to retain amino groups during amino-acid breakdown by transferring the amino group from the amino acid to a keto acid. They are found in many tissues including heart, liver, kidney, and muscle. When there is tissue destruction, as seen following a MI or during hepatic necrosis, increased amounts of the aminotransferase enzymes can be detected in the plasma or serum. Human serum contains many different transaminases. The two most commonly measured are glutamic oxaloacetic transaminase (GOT, aspartate aminotransferase, or AST) and glutamic pyruvic transaminase (GPT, alanine aminotransferase, or ALT). Serum Aspartate Aminotransferase, AST (Transaminase, GOT) Aspartate aminotransferase (AST) is found in practically every tissue of the body, including red blood cells. It is in particularly high concentration in cardiac muscle and liver, intermediate in skeletal muscle and kidney, and in much lower concentrations in the other tissues. The discovery by LaDue, Wroblewski, and Karmen that the serum AST (GOT) concentration increased shortly after the occurrence of a myocardial infarction greatly accelerated the search for enzymes in serum as indicators of specific tissue damage. The measurement of the serum AST level is helpful for the diagnosis and following of cases of myocardial infarction, hepatocellular disease, and skeletal muscle disorders. MLAB 2401 - Cllinical Chemistry Lab Manual ! 149 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) The serum activity of AST is increased after myocardial infarction, in liver disorders, in trauma to or in diseases affecting the skeletal muscle, after a renal infarct, and in various hemolytic conditions. Myocardial infarction. The serum activity of AST begins to rise about 6 to 12 hours after myocardial infarction and usually reaches its maximum value in about 24 to 48 hours. It usually returns to normal by the fourth to sixth day after the infarct. The increase in activity is not as great as for CK, nor does it rise as early after the infarct. It is a much less specific indication of myocardial infarction than the rise in CK, since so many other conditions, e.g., liver, muscle, or hemolytic disease, can cause a rise in serum AST. Prolonged myocardial ischemia may be accompanied by a rise in serum AST. Congestive heart failure also is associated with an increased serum activity of AST because of the hepatic ischemia and anoxia that is produced. Serum Alanine Aminotransferase, ALT (Transaminase, GPT) The concentration of ALT in tissues is not nearly as great as for AST. It is present in moderately high concentration in liver, but is low in cardiac and skeletal muscles and other tissues. Its uses for clinical purposes is primarily for the diagnosis of liver disease and to resolve some ambiguous increases in serum AST in cases of suspected myocardial infarction, when the CK test or isoenzyme tests for LD and CK-MB are not available. When both AST and ALT are elevated in serum, the liver is the primary source of the enzymes (liver ischemia because of congestive heart failure or other sources of liver cell injury). If the serum AST is elevated while the ALT remains within normal limits in a case of suspected myocardial infarction, the results are compatible with myocardial infarction. The serum activity of ALT is increased in a variety of hepatic disorders. Principle AST (GOT) and ALT (GPT) catalyze the transfer of amino groups from specific amino acids to ketoglutaric acid yielding glutamic acid and oxaloacetic or pyruvic acid respectively. These ketoacids are then determined colorimetrically after their reaction with 2,4dinitrophenylhydrazine (DNP). SGOT (AST) Reitman-Frankel reaction. SGOT catalyzes the reaction of aspartic acid and alphaketoglutaric acid to oxaloacetic acid and glutamic acid. The oxaloacetic acid is treated with 2, 4-dinitrophenylhydrazine in an alkaline medium to produce a highly colored hydrazine which can be measured colorimetrically. SGPT (ALT) SGPT catalyzes the substrate alanine and alpha-ketoglutaric acid to pyruvic acid and glutamic acid. The pyruvic acid is treated with 2,4-dinitrophenylhydrazine in an alkaline medium to form a highly colored hydrazine which is measured photometrically. 150 ! MLAB 2401 - Clinical Chemistry Lab Manual UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) A. Preparation of a Calibration Curve for SGOT and SGPT Values 1. Into large (16 x 150 mm) test tubes pipet the solutions indicated in column 2, 3, and 4. 1 Tube # 1 2 3 4 5 6 B. 2 Calibration Standard Solution (uL)/ mL 0 50 100 150 200 250 0 .050 .100 .150 .200 .250 3 Substrate (mL) 4 Water (mL) 5 Serum GOT Activity (SF units/mL) 6 Serum GPT Activity (SF units/mL) 0.5 0.450 0.400 0.350 0.300 0.250 0.1 0.1 0.1 0.1 0.1 0.1 0 20 55 95 148 216 0 23 50 83 125 B Absorbance 2. Add 0.5 mL color reagent to each tube. Shake gently and leave at room temperature for 20 minutes. 3. Add 5 mL of 0.4N NaOH to each tube. Mix by inversion. 4. Wait 5 minutes, then read and record absorbance of all tubes at 500 nm using water as a reference. 5. Plot a calibration curve of absorbance values (ordinate) vs. the corresponding units of GOT and GPT (abscissa). GOT (AST) PROCEDURE 1. Into appropriately labeled (control, patient, etc.) 13 x 100 mm tubes, pipet 0.5 mL Sigma prepared substrate into each patient test tube. Place in a 37 water bath to warm. 2. Add 0.1 mL sample and shake gently to mix. Leave in water bath. 3. Exactly one hour after adding serum, add 0.5 mL Color Reagent. Shake gently and leave at room temperature for 20 minutes. 4. Add 5.0 mL of 0.4N NaOH and mix by inversion. 5. Wait at least 5 minutes, then read and record the absorbance at 500 nm on the same instrument used to prepare calibration curve, using water as a reference. MLAB 2401 - Cllinical Chemistry Lab Manual ! 151 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) 6. C. Determine GOT activity using calibration curve. GPT (ALT) PROCEDURE 1. Into each appropriately labeled test tube, pipet 0.5 mL of alanine - KG substrate. Place in a 37 water bath to warm. 2. Add 0.1 mL sample and shake gently to mix. Leave in water bath. 3. Exactly 30 minutes after adding serum, add 0.5 mL Color Reagent. Shake gently and leave at room temperature for 20 minutes. 4. Add 5.0 mL 0.4N NaOH and mix by inversion. 5. Wait 5 minutes, then read and record absorbance at 500 nm in the same instrument used in preparing your calibration curve, using water as a reference. 6. Determine GPT activity using your calibration curve. Results normal borderline GOT Up to 28* 28-40* GPT Up to 21* 21-35* *Sigma-Frankel Units per milliliter 152 ! MLAB 2401 - Clinical Chemistry Lab Manual UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Name Date TRANSAMINASES Wavelength Calibration Curve Tube # 1 2 3 4 5 6 2 Calibration Standard Solution uL or mL 0 50 100 150 200 250 Spectrophotometer Used 3 Substrate (mL) 4 Water (mL) Serum GOT Activity SF units/mL Serum GPT Activity SF units/mL 0.500 0.450 0.400 0.350 0.300 0.250 0.1 0.1 0.1 0.1 0.1 0.1 0 20 55 95 148 216 0 23 50 83 125 B 0 0.050 0.100 0.150 0.200 0.250 Transaminase Test Results AST Absorbance AST Concentration ALT Absorbance Absorbance ALT Concentration Control 1 _______________ Control 2 Patient 1 Patient 2 AST Quality Control Your Results Controls= range of expected results. In control? Yes / No Level 1 ID______________ Level 2ID_______________ Accepting Patient Results? Reason ALT Quality Control Your Results Controls= range of expected results. In control? Yes / No Level 1 ID______________ MLAB 2401 - Cllinical Chemistry Lab Manual ! 153 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) ALT Quality Control Level 2ID_______________ Accepting Patient Results? 154 ! MLAB 2401 - Clinical Chemistry Lab Manual Reason UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) MLAB 2401 - Cllinical Chemistry Lab Manual ! 155 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) Name Date Study Questions Instructions: Based on information presented in lecture and lab notes, answer the following questions. Legibly write your answers in the space provided. Unless otherwise indicated, each question is worth one point. I. What is an enzyme? II. What is an isoenzyme? (2 pts) III. State at least one (1) of the three general conditions that would cause cytoplasmic enzymes to diffuse into the plasma resulting in increased concentration. IV. According to the information presented in the lab, compare/contrast fixed time and kinetic methods of enzyme assay as to time, danger of inactivation, and units reported. (3 pts) incubation time inactivation units reported Fixed time Kinetic Assay V. Amylase is an enzyme that catalyzes the degradation of ___________________. VI. List at least three (3) body fluids that contain measurable amounts of amylase. (3 pts) VII. Serum amylase and lipase are elevated in diseases of the _________________. VIII. After considering the three ways used to determine enzyme concentration, how is the amylase concentration determined in this laboratory procedure? IX. What is the indicator for this amylase method? 156 ! MLAB 2401 - Clinical Chemistry Lab Manual UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) X. The lab states that amylase is more sensitive and the lipase test is more specific. In your own words, explain what this means. XI. What purpose/function is performed by the transaminases? XII. Write the new preferred names for SGOT and SGPT indicating which is which. XIII. Write the reaction catalyzed by SGOT. Label the substrate and products. (2 pts) XIV. Write the reaction catalyzed by SGPT. Label the substrate and products. (2 pts) XV. What component in the Sigma Color Reagent reacts with oxaloacetic or pyruvic acids to give a measurable colored product? XVI. What are the normal values for SGOT and SGPT by this method? Use correct units. (2 pts) XVII. Compare the expected values for SGOT and SGPT following myocardial infarction? (2 pts) MLAB 2401 - Cllinical Chemistry Lab Manual ! 157 UNIT: Enzymes I (Colorimetric/Turbidimetric/End-point) (continued) XVIII. Compare the expected values for SGOT and SGPT for the following liver conditions. SGOT hepatitis B obstruction B cirrhosis B cancer B 158 ! MLAB 2401 - Clinical Chemistry Lab Manual SGPT