Amiodarone - NHS Grampian
advertisement

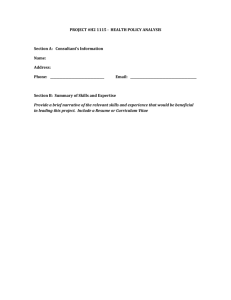
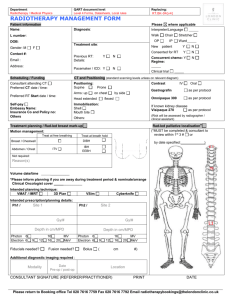
Shared Care Policy and Prescribing Information for General Practitioners for oral Amiodarone (Adults only, non-renal patients) Publish public Applies to: NHS Grampian Coordinator Clinical Pharmacist Cardiology Signature: K McKessack Authorised for issue by Medicine Guidelines and Policies Group Signature: C Hind PATIENT NAME Version 4 Document no: NHSG/SCPa/Amio/MGPG730 Effective date: April 2015 Review Date: April 2017 Supersedes: Version 3 HOSPITAL WARD CHI NUMBER TELEPHONE NO ADDRESS CONSULTANT (print name) DATE OF BIRTH THERAPEUTIC INDICATION FOR THIS PATIENT: DATE SIGNATURE (to be completed by consultant) DOSAGE/PREPARATION/ROUTE/FREQUENCY OF ADMINISTRATION: (to be completed by consultant) SAFE PRACTICE IS THAT THE CLINICIAN WHO ORDERS THE TEST MUST ACT ON THE RESULT CARE WHICH IS THE RESPONSIBILITY OF THE HOSPITAL CONSULTANT CARE WHICH IS THE RESPONSIBILITY OF THE GENERAL PRACTITIONER 1. Baseline: 1. Thyroid function tests; liver function tests (LFTs) and U&Es. All patients should have a baseline chest Xray and ECG. 2. 3. 2. Before starting amiodarone: If respiratory symptoms, e.g. cough, breathlessness, wheeze, haemoptysis, then clinical assessment including spirometry/gas transfer. If asymptomatic, not essential to perform spirometry/gas transfer, unless clinician considers patient "high risk", e.g. daily dose 400mg/day or greater or if concern about underlying respiratory disease. 3. Copy of results to be sent to GP. 4. Initiation of therapy and recommendations for dose increments ensuring the patient is aware of required monitoring and side effects to report. 5. Decision on final dose required for patient. 6. Monitoring clinical response to treatment. 7. If pulmonary toxicity suspected arrange urgent chest X-ray and lung function tests including where possible gas transfer factor. 8. If optic neuropathy suspected arrange ophthalmological examination. 4. 5. 6. GP may be asked to undertake baseline blood tests if the hospital consultant is physically unable to obtain blood samples. Prescribing of medication under guidance of consultant. Check before prescribing medication that the monitoring is up to date and that results are within the normal range. GP should be aware that the drug can cause hypo or hyperthyroidism, hepatotoxicity, pulmonary toxicity, peripheral neuropathy, phototoxicity, optic neuropathy. Patients should be asked about the development of new or progressive shortness of breath, non-productive cough, or deterioration in general health at each visit. Persistent (>2 weeks) respiratory symptoms should prompt clinical assessment, discussion with the hospital consultant and a repeat chest X-ray/detailed pulmonary function tests. Any abnormal results including those noted above should be reported to the consultant. The General Practitioner has primary responsibility for monitoring therapy according to the schedule below. Clinical assessment of thyroid status combined with thyroid function tests and LFTs every 6 months and for up to 8 months after discontinuing therapy. If pulmonary toxicity suspected contact consultant to arrange urgent chest X-ray and lung function tests including where possible transfer factor. If optic neuropathy suspected contact the clinical decision unit at the eye clinic, Aberdeen Royal Infirmary to arrange ophthalmological examination. When writing laboratory request forms always include details of the patient’s medication NOTE: in addition to absolute values for haematological indices a rapid fall or a consistent downward trend in any value should prompt caution and extra vigilance. If something unexpected occurs Contact Consultant. Notify the consultant if the drug is stopped. UNCONTROLLED WHEN PRINTED Review Date April 2017 (sooner if recommendations change) SCP and Prescribing Information for GPs for oral AMIODARONE - Version 4, April 2015 NHSG/SCPa/Amio/MGPG730 -1- Shared Care Policy and Prescribing Information for General Practitioners for oral Amiodarone (Adults only, non-renal patients) ABNORMAL MONITORING RESULTS ACTION TO BE TAKEN discuss with consultant urgently Hypo or hyperthyroidism identified † Severe liver function abnormalities Clinical signs of liver disease discuss with consultant urgently Pulmonary toxicity suspected discuss with consultant urgently to arrange chest X-ray and lung function tests including where possible transfer factor Blurred or decreased vision discuss with consultant urgently discuss with the clinical decision unit at the eye clinic, Aberdeen Royal Infirmary urgently † Amiodarone may be associated with a variety of hepatic effects, including cirrhosis, hepatitis and jaundice. At the beginning of therapy, elevation of serum transaminases (1.5 to 3 times normal) may occur. These may return to normal with dose reduction, or sometimes spontaneously. For specific product information please consult the current summary of product characteristics (http://emc.medicines.org.uk/) and the BNF (http://www.bnf.org/bnf/) Other information Amiodarone is highly protein bound and has a very long half-life (on average 50 days), monitoring should be continued for up to 8 months after discontinuing therapy. There are a number of drug interactions that must be considered. When a new drug is prescribed please refer to Summary of Product Characteristics (SPC), BNF or contact Medicines Information. Some of the important drugs that interact with amiodarone include warfarin, digoxin, phenytoin, and drugs which prolong the QT interval. Amiodarone can significantly increase the International Normalised Ratio (INR) suddenly; therefore the INR should be monitored very closely for two weeks following the addition of amiodarone to existing warfarin therapy. If amiodarone and warfarin are started concurrently a warfarin dose reduction of approx. one third should be considered along with close monitoring of the INR. On discontinuation of amiodarone the INR may be significantly reduced, and therefore INR should be monitored closely. Phenytoin plasma levels should be monitored and dosage should be reduced if toxicity occurs Drugs that prolong the QT interval are contra-indicated (check SPC for full list and refer to https://www.crediblemeds.org/index.php/login/dlcheck website). The dose of simvastatin should not exceed 20mg daily in patients receiving concomitant medication with amiodarone, due to the increased risk of myopathy and rhabdomyolysis. Amiodarone sensitises the skin to sunlight, patients can burn very easily. Exposure to direct sunlight also produces pigmentation of the skin, which can be permanent. To minimise the photosensitivity reactions exposure to sunlight and ultraviolet light should be limited by wearing protective clothing and using sunscreen with a high protection factor. Ophthalmological Reactions. Patients on continuing therapy always develop micro-deposits in the cornea. This is usually of no clinical consequence and may rarely cause subjective symptoms such as visual haloes in dazzling light (especially at night) and blurring vision. Optic neuropathy is rare and usually presents as decreased or blurred vision. Pregnancy Discuss with consultant. Contra-indicated in pregnancy. Advise to contact their doctor immediately should pregnancy occur. Breast-feeding Discuss with Aberdeen Maternity Hospital. Contra-indicated in breast-feeding. Responsibilities of GPs undertaking monitoring A GP agreeing to monitor amiodarone should: Ensure that the relevant monitoring requirements are undertaken at the correct frequency, Ensure that the test results are checked for any abnormality as soon as the results are available, Ensure abnormal results are acted upon, Only continue to prescribe amiodarone if it is being satisfactorily monitored, Contact the consultant in the event of a drug reaction or monitoring abnormality or anything you are unhappy about, Be alert for any of the known adverse reactions. The patient should be encouraged to ensure blood tests are taken at the correct intervals. UNCONTROLLED WHEN PRINTED Review Date April 2017 (sooner if recommendations change) SCP and Prescribing Information for GPs for oral AMIODARONE - Version 4, April 2015 NHSG/SCPa/Amio/MGPG730 -2-