Chesapeake Regional Medical Center Therapeutic Hypothermia
advertisement

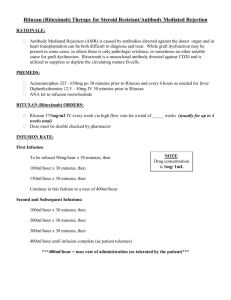
736 Battlefield Blvd N, Chesapeake, VA 23320 THERAPEUTIC HYPOTHERMIA PROTOCOL *****EMERGENCY DEPARTMENT/INTENSIVE CARE UNIT***** Allergies: __________________ Ht: __________ Wt: __________Kg 1. Admit to Intensive Care Unit: Date Time a. Time of Arrest: ____________________________________ Ordered Ordered b. Time of Return of Spontaneous Circulation_______________ c. Time Cooling Initiated: ______________________________ 2. INCLUSION CRITERIA: Cardiac Arrest with initial rhythm of ventricular fibrillation or pulseless ventricular tachycardia with return of spontaneous circulation (ROSC). Initiate hypothermia therapy as soon as possible. 3. EXCLUSION CRITERIA: a. b. c. d. e. f. g. h. i. DNR/DNI or severely impaired cognitive status prior to cardiac arrest Glascow Motor Scale GREATER than 5 or patient is following commands Pulseless GREATER than 60 minutes GREATER than 12 hrs since return of Spontaneous Circulation (ROSC) Initiate hypothermia therapy as soon as possible. Metastatic Cancer or other terminal illness Comatose baseline due to CNS depressing drugs, ICH or SAH, or other possible causes (i.e. drug intoxication, pre-existing coma) Sepsis as etiology for arrest Uncontrollable bleeding Significant trauma, especially intra-abdominal such as splenic or liver laceration (due to increased risk of bleeding) 4. CONSULTS: a. Pulmonary / Critical Care Medicine MD___________________________________________ b. Cardiology __________________________________________________________________ c. Neurologist _________________________________________________________________ d. OB/GYN consult if pregnant:__________________________________________________ e. Vascular Access Team for Central Line or PICC and Arterial line insertion f. Rapid Response Team (CODE SILVER - ICE) g. Notify Nursing Supervisor immediately for admission to ICU h. Other: ____________________________________ 5. EQUIPMENT LIST: a. Arterial Line Kit (radial, ulnar, or femoral site) b. Central Line Insertion Kit c. Two 1 liter bags of 0.9% NaCL at 39.2˚F or 4˚C d. Hypothermia Cooling System e. Cooling Pads – Use sizing chart to determine size ( for torso and upper and lower limbs) f. Foley Catheter Temperature probe (preferred monitoring route) g. Esophageal Temperature probe (secondary route if patient anuric or unable to insert Foley catheter) h. Rectal Temperature probe (use only if Foley catheter or Esophageal temperature inaccessible) i. Neuromuscular Blockade Equipment (BARD Pump and Peripheral Nerve Stimulator) j. Fluid Warmer (if needed) k. CVP Monitoring Kit l. NGT insert orally if not contraindicated m. Forehead sensing / Ear sensing probes for oxygen saturation. 1of 12 736 Battlefield Blvd N, Chesapeake, VA 23320 Date Ordered Time Ordered *****EMERGENCY DEPARTMENT/INTENSIVE CARE UNIT***** 6. INITIAL LABORATORY ORDERS: STAT a. Urine HCG on all women of child bearing age (less than 55) Obtain serum if urine not available. b. CBC/Platelets/ PT / PTT /INR / Fibrinogen c. CMP / Magnesium / Ionized Calcium / Phosphorous d. Amylase / Lipase / Lactic Acid e. CPK MB / CK / Troponin f. Pan Culture – Blood Culture ( 2 Sets), Urine Culture, Sputum Culture (if appropriate) g. Urinalysis h. ABG / ScvO2 □ Toxicology screen if appropriate MD must check √ box to order 7. DIAGNOSTIC TESTS: a. 12 Lead EKG STAT, then Q 8 hrs X 2 Reason for test: post cardiac arrest or MI b. Chest X Ray Portable STAT: Repeat in am and in 72 hrs. c. Echocardiogram Routine unless specified below: to determine ejection fraction. MD must check √ box to order □ ASAP per Cardiology request □ Within 24 hours of initiation of protocol □ Repeat in am d. CT Scan of Head without contrast to r/o intracranial hemorrhage, or other causes of coma STAT e. EEG (routine) 8. VENTILATOR MANAGEMENT: Mode: A/C Rate: 15 VTE: 6- 8 ml/kg of IBW FiO2 to maintain O2 saturation > 94% PEEP: 5 ABG in 30 minutes (Temperature correct) If unable to temp correct subtract 10mm PCO2 and 20mm PO2. Inline nebulizer with Albuterol 2.5 mg /Atrovent 0.5 mg Q 4 H PRN for wheezing Ventilator Temperature – Respiratory Therapy to turn heater to non invasive setting (89.6˚F or 32˚C) during cooling and maintenance phase. 9. LINE / TUBE PLACEMENT: a. Place 2 large bore peripheral lines b. Place arterial line (radial, ulnar, or femoral) for blood pressure monitoring prior to cooling. c. Place central line or PICC line prior to initiation of hypothermia d. If patient requires catherization, arterial sheath and central line can be placed in cath lab by Cardiologist. e. Insert temperature sensing Foley Catheter prior to cooling f. Insert oral gastric tube and connect to low intermittent suction. Clamp for meds. 2of 12 736 Battlefield Blvd N, Chesapeake, VA 23320 Date Ordered Time Ordered *****EMERGENCY DEPARTMENT/INTENSIVE CARE UNIT***** 10. MONITORING: INDUCTION/COOLING AND REWARMING PHASES: a. Vital Signs, Core Body Temperature, and Water Temperature of Cooling Unit - every 15 minutes during induction, until less than 93.2 ˚ Fahrenheit (34 ˚ Celsius), - then every 30 minutes times 2 - and then every 1 hour b. MAP Overall Goal 70-100 (MAP 70-80 if ON Pressors; MAP 80-100 if NOT on Pressors) c. ScVO2 Goal 65 % or greater d. Notify MD if urine < 2ml/kg IBW q4H e. Modified Ramsay Scale GOAL 2-3 (Achieve baseline then use during rewarming phase) - Every 30 minutes till Ramsey Goal is achieved - then every 1 hour Light / Awake 1 Anxious, agitated or restless or both 4 2 Cooperative, oriented and tranquil 5 Deep / Asleep Brisk response to light glabellar tap or loud auditory stimulus Sluggish response to a light glabellar tap or loud auditory stimulus 3 Responds to commands only 6 No response to a light glabellar tap or loud auditory stimulus START PROPOFOL UNLESS OTHERWISE NOTED PROPOFOL (DIPRIVAN) INFUSION (Concentration: 10 mg / ml) (Agent of Choice unless specified by MD) ▪ Start Propofol IV Infusion at 50 mcg/kg/min ▪ Titrate by 5 – 10 mcg/kg/min every 5 minutes until sedation goal is achieved. ▪ Maximum infusion rate 100 mcg/kg/min MD must check √ □ ▪ ▪ □ box to order MIDAZOLAM (VERSED) INFUSION (Conc: 1 mg/ml) Start if Propofol is contraindicated Bolus 1-2 mg IV Start Midazolam Infusion at 1 – 3 mg/hr Titrate by 1 – 2 mg/hr until sedation goal is achieved Maximum infusion rate: 15 mg/hr □ FENTANYL (SUBLIMAZE) INFUSION (1 mg/100 ml NS = 1000 mcg / 100 ml = 10mcg/ml ) ▪ Start Fentanyl Infusion at 25 – 100 mcg/hr. ▪ Maximum infusion rate: 300 mcg/hr 3of 12 f. Train of Four (TOF) per Neuromuscular Blockade Protocol GOAL 2 – 3 (See attached) - Every 1 hour till TOF is at Goal g. Central Venous Pressure Monitoring - Every 1 hr GOAL CVP 8 mmHg- 20 mmHg during cooling /induction phase - then q4 hours during maintenance phase h. Assess skin - Every 4 hours (pull pads back to fully assess skin) i. Do not treat for Bradycardia if BP and urinary output acceptable. j. Hypothermia therapy increases risk for bleeding. Notify MD for significant bleeding - may consider terminating hypothermia therapy 736 Battlefield Blvd N, Chesapeake, VA 23320 Date Ordered Time Ordered *****EMERGENCY DEPARTMENT / INTENSIVE CARE UNIT***** 11. COOLING: INDUCTION PHASE - GOAL Temperature 89.6 – 93.2 ˚ F (32 – 34˚C) Target temperature 91.4˚F or 33˚C within 4 hours of ROSC. ***DO NOT COOL TO <32˚C (89.6˚F)*** a. b. c. d. e. f. g. h. Infuse 2 liters 0.9 % NaCL (1L per site concurrently) at 39.2˚F (4˚C) over 30 minutes or ASAP (PER PERIPHERAL LINE ONLY) if no evidence of Pulmonary Edema or if not already done. Obtain access (arterial line and central line) Assess patient for baseline Ramsay Scale Score and Train of Four (TOF) Initiate sedation and paralytic. All patients are to be paralyzed prior to hypothermia therapy Attach Hypothermia Cooling Unit. Cooling pads to cover 40 % of total body surface area (TBSA). Set Target Temperature at 91.4˚F (33˚C) DO NOT CUT PADS for any reason. (Reference Hypothermia Cooling Unit Competency) If UNABLE to achieve target core temperature WITHIN 4 HOURS, notify MD for further orders. Consider ice packs to neck, groin, and axilla. Room Temperature – Turn room thermostat to lowest setting during cooling and maintenance phase If patient requires Cardiac catherization procedure continue hypothermia therapy while in cath lab. GUIDELINES FOR INFUSION OF VECURONIUM STANDING ORDERS NO WAKE UP ASSESSMENT DURING COOLING PHASE A. Patient MUST be on ventilator before this drug is administered. B. Patient requires paralysis. If patient is not already paralyzed, administer a bolus of 100 mcg/kg Vecuronium IV. Patient weight ______________kg. C. Vecuronium infusion (20mg/20ml NS syringe via Bard Infusion Pump) to run at 1 mcg/kg/min D. Perform and document initial current (mA’s) and Train of Four (TOF) prior to drug therapy. Evaluate and chart “train of four” (TOF) q 1hr x 4hr, then q 4h x continuously. GOAL = Maintain TOF between 2 and 3 E. If TOF < 2, decrease infusion by next increment using Bard infusion pump and check TOF q 15min until desired range. F. If TOF > 3, increase infusion by next increment using BARD infusion pump and check TOF q 15 min until in desired range. G. Eye care is to be provided q 24 hr with Lacrilube. H. Patient positioning: Reposition patient q2hr to include passive ROM and other appropriate decubitus prevention measures as otherwise ordered. I. If patient exhibits signs or symptoms of any adverse reaction to Vecuronium, notify MD immediately. Order required to discontinue infusion and for reversal agents. Reversal Agents: Choose A or B to reverse Vecuronium MD must check √ box to order □ □ A. 1. Neostigmine (Prostigmine) 0.5-2 mg IV. TOTAL not to exceed 5 mg. 2. Glycopyrrolate (Robinul) 0.2 mg IV for each 1mg of Neostigmine. May be mixed in same syringe as Neostigmine. 3. Atropine 0.6 – 1.2 mg for each 0.5 – 2.5 mg of Neostigmine. Give 30 seconds before Neostigmine. B. 1. Endrophonium Chloride (Tensilon) 10 mg IV every 5 -10 minutes up to 40 mg. To be given in conjunction with Atropine 2. Atropine 0.01 – 0.02 mg/kg (give before Tensilon) Physician Signature: _____________________________ 4of 12 Date:_________________________ 736 Battlefield Blvd N, Chesapeake, VA 23320 Date Ordered Time Ordered ***** INTENSIVE CARE UNIT***** 12. SERIAL LABORATORY ORDERS: NOTE: For ABG and Central Venous Blood – Use temperature correction when analyzing ABGs and Central Venous Blood. The temperature should be written on a bright sticker and attached to the syringe and it should be indicated when ordering the lab. Follow Serial Laboratory checks per Hypothermia Electrolyte Replacement Protocol if used a. ABG q 6 hrs and PRN b. ScvO2 q6h until rewarming process complete. Call MD for Scvo2 <65 c. Lactic Acid q 6 hours until warming process complete d. Repeat CPK – MB, CK, Troponin q 6 hours times 2 e. Ionized Calcium, CBC / PT / INR/PTT/ Fibrinogen/ BMP/ Mg / Phosphorous every 6 hrs 13. NUTRITION: a. NPO b. Nutrition Consult Day #3 (Do not start Tube feedings until rewarming process completed) 14. IV FLUIDS: Infuse 2 liters (ROOM TEMPERATURE) of 0.9 % NaCL over 30 minutes if MAP < 80 and CVP < 8. Give in addition to the 2 liters given at induction of therapy X 1 only. CALL MD IF GOAL IS NOT MET Maintenance IVF: D5NS at 75ml/hr unless specified by MD : ____________________________ 15. GI PROPHYLAXIS: Pantoprazole 40 mg IV daily 16. VENOUS THROMBOSIS: Sequential Compression Device MD must check √ box below to order □ Heparin 5000 units subcutaneously every 8 hours if less than 70 years old □ Heparin 5000 units subcutaneously every 12 hours if greater than or equal to 70 years old 17. ANTIEPILEPTIC PROPHYLAXIS: Keppra 1gm q12 IVPB 18. PRE-MEDICATION FOR PRBC & PLATELETS (unless hypothermic): MD must check √ box below to order □ Acetaminophen Liquid 160 mg/5ml – Give 650 mg per oral gastric tube X 1 dose Diphenhydramine Liquid 25 mg/10ml – Give 25mg per oral gastric tube X 1 dose OR □ Acetaminophen Supp 650 mg X 1 per rectum Diphenhydramine 25 mg IV X 1 dose only 19. BLOOD GLUCOSE CONTROL: ALL BLOOD MUST BE DRAWN FROM ALINE/VASCULAR ACCESS DEVICE. DO NOT DO FINGERSTICKS - Give 1 unit Regular insulin SQ for 10mg/dl for BG >140. Initiate Intensive Insulin Therapy Infusion Protocol for BG >170 X 2 consecutively. (Scan protocol to pharmacy) 20. VASOACTIVE AGENTS: Hypotension MAP < 80 Levophed (Norepinephrine) Infusion: (4mg / 250ml ) Begin at 2 – 4mcg/min, titrate to maintain MAP ≈ 70-80 mmHg. Maximum Dose: 30 mcg/min Notify MD if unable to maintain GOAL. May consider Neosynephrine (Phenylephrine) Drip 5of 12 736 Battlefield Blvd N, Chesapeake, VA 23320 21. ANTIHYPERTENSIVES: Hypertension for MAP > 100 consistently Nitroglycerin Infusion: ( 100 mg/ 250 ml) Begin at 10 mcg/min for MAP > 100 mmHg (titrate to MAP 80-100) Maximum Dose: 200 mcg/min Consider Esmolol for hypertension with tachycardia or with acute ischemia/MI w/o LV dysfunction. Call MD for further orders. □ Esmolol (Brevibloc) 2.5gm/250ml NS. Start at 50mcg/kg/min and titrate by 50mcg/kg/min every 5-10 min. Call MD if more than 200mcg/kg/ min required. Maximum rate of 300 mcg/kg/min. 22. HEPARIN INFUSION THERAPY: If patient is currently on or requires Heparin therapy post AMI/PCI: a. Initiate Integrilin/Heparin protocol if ordered b. Integrilin dosing does not change. Continue dosing based on original protocol. c. Administer full dose Heparin bolus then reduce heparin protocol titration rate by 50% while patient is in the Cooling Phase. d. Once patient begins warming phase, draw PTT stat and adjust heparin infusion based on ORIGINAL protocol rate. 23. RE-WARMING PHASE: DO NOT PERMIT HYPERTHERMIA > 98.6° F (37°C) in the first 24 hours after cooling phase a. Initiate 24 hours after target temperature reached. b. Rewarm to 98.6 ˚ F (37 ˚C) over 12 hours. c. Initiate “Warming Algorithm” d. Hold all potassium containing fluids if serum K is > 3.5 immediately before and during re-warming phase. DO NOT INITIATE rewarming until last drawn K level is known. DO NOT INITIATE rewarming and notify MD if K >5.0. e. Stop NEUROMUSCULAR BLOCKADE infusion after temperature reaches 96.8 ˚ F (36 ˚ C) f . MANAGEMENT OF SHIVERING: BEDSIDE SHIVERING ASSESSMENT SCALE (BSAS) No Shivering Mild: Localized shivering to neck and or chest Moderate: Shivering involving neck and/or chest and upper extremities Severe: Generalized (total body) shivering involving all 4 extremities If Bedside Shivering Assessment Scale (BSAS) greater than or equal to 1: 0 1 2 3 Meperidine 12.5-25 mg IV q4-6 hours PRN shivering (not to exceed 100 mg) – AVOID in renal failure , history of seizures, MAO inhibitors, Buspar, SSRI Antidepressants, or late term pregnancy Or (alternative use only if Meperidine cannot be used) □ Dexmetatomidine 1mcg/kg IV over 10 minutes q4 hours PRN shivering (Not to exceed 24 hours) g. Acetaminophen 650 mg via NGT or rectally every 4 hours if temperature spikes greater than 98.6˚F (37˚C). Do not exceed 3 gm/day. h. Maintain normothermia for 48 hours using acetaminophen. Use standard cooling blanket to target temperature of 98.6˚F (37˚C) as needed to help maintain normothermia 24. ELECTROLYTE REPLACEMENT If serum creatinine 2 or less initiate the Intensive Care Electrolyte Replacement for Hypothermia Therapy. (See attached order set) If serum creatinine greater than 2 initiate the Renal Electrolyte Replacement for Hypothermia Therapy. (See attached order set) Physician Signature: _____________________________ 6of 12 Date:_________________________ 736 Battlefield Blvd N, Chesapeake, VA 23320 Intensive Care Electrolyte Replacement Orders for Hypothermia Therapy 1. The Ordering of replacement protocols automatically discontinues previous (prn, one-time) replacement orders for each electrolyte ordered. 2. The physician indicates which orders to initiate. These orders will remain in effect until the patient is discharged from the ICU or contraindications are present. 3. Contraindications to using these replacement protocols include: -Serum creatinine greater than (>) 2 (M.D. may write an order to give at a higher level) -Urine output less than 200cc over previous eight hours 4. Based on physiological interactions, if several electrolytes are known to be low, they should be replaced in the following order: (This is not an order for additional labs.) a. Calcium (if IONIZED level <4), should be replaced before Magnesium or Phosphate b. Magnesium should be replaced before Potassium 5. Discontinue replacement orders upon transfer out of Intensive Care. 6. The physician has ordered the following: Potassium Replacement: IF NO PICC, CVP OR MEDIPORT USE 10 MEQ KCL/100ML STERILE H2O ENTERAL ROUTE is preferred for patients without rhythm disturbances. Tube feeding must be at goal or patient tolerating a full liquid diet Serum Level (mEq/L) If patient receiving potassium in IV infusion 3.9 - 4 None 10 mEq KCL po / NG or If patient NOT receiving other potassium infusion 10 mEq KCL po /NG or 10 mEq KCL / 100 ml Sterile Water over 1 hour 20 mEq KCL po / NG or 3.7 – 3.8 Infusion Rate 10 mEq/Hour 10 mEq/hour 10 mEq KCL/100 ml Sterile Water IV over 1 hour 20 mEq KCL in 100 ml Sterile Water IV over 2 hours Recheck serum level In am 2 hours post IV repletion or 4 hours post enteral repletion *DO NOT REPLACE POTASSIUM DURING REWARMING PHASE UNLESS LESS THAN 3.5mEq/L* 3.5 – 3.6 10 mEq/100 ml Sterile Water IV over 1 hours and 20 mEq/100 ml Sterile Water IV over 2 hours 20 mEq KCL IV in 100 ml Sterile Water over 2 hours X 2 doses 10 mEq/hour 2 hours post IV repletion 3.3 – 3.4 20 mEq KCL IV in 100 ml Sterile Water over 2 hours X 2 doses 20 mEq/100 ml Sterile Water IV over 2 hours X 2 doses and 10 mEq/100 ml Sterile Water IV over 1hour 10 mEq/hour 2 hours post IV repletion 3.2 or less 20 mEq/100 ml Sterile Water IV over 2 hours X 2 doses and 10 mEq/100 ml Sterile Water IV over 1 hour 20 mEq KCL/100 ml Sterile Water IV over 2 hours X 3 doses 10 mEq/hour 2 hours post IV repletion 7of 12 736 Battlefield Blvd N, Chesapeake, VA 23320 Magnesium Replacement: Serum Level (mg/dl) Dose Infusion Rate 1 gm/hr Recheck serum level Magnesium 3 grams IV in 100 ml 0.45% NaCl over 2 hours Over 2 hours 50 ml/hr = 1.5 gm/hour In AM 1.3 – 1.4 Magnesium 4 grams IV in 100 ml sterile water over 3 hours Over 3 hours 33 ml/hr = 1.3 gm/hour In 4 hours post repletion Less than or equal to 1.2 Magnesium 5 grams IV in 100 ml 0.45% NaCl over 4 hours Over 4 hours 25 ml/hr = 1.25 gm/hour In 4 hours post repletion 1.5 – 1.8 Phosphate Replacement: ENTERAL route is preferred for patients without rhythm disturbances. Tube feeding must be at goal or patient tolerating a full liquid diet Serum Level Dose of Sodium Phosphate Infusion Rate Recheck serum level (mg/dl) (1 ml = 3 mmol) With AM labs If 2.5 – 1.6 and patient able Neutra-Phos 1 tablet by mouth Every 8 hours times 3 doses to tolerate ENTERAL dose or NG 9 mmol NaPO4 in 100 ml Over 4 hours With AM labs 2.3 – 2.5 a. 1.7 – 2.2 1.1 – 1.6 Less than or equal to 1 0.45% NS over 4 hours 12 mmol NaPO4 in 100 ml 0.45% NS over 4 hours 18 mmol NaPO4 in 100 ml 0.45% NS over 6 hours 24 mmol Na PO4 in 100 ml 0.45% NS over 6 hours (25 ml/hr) Over 4 hours (25 ml/hr) Over 6 hours (17 ml/hr) Over 6 hours (17 ml/hr) With AM labs 4 hours post repletion 4 hours post repletion Calcium Replacement: a. b. c. Do not administer calcium and magnesium or calcium and phosphate through the same IV at the same time. Calcium gluconate is the preferred agent and may be administered through either a central or peripheral access. Call MD if the serum bicarbonate (HCO3) or serum CO2 greater than or equal to 25. Calcium chloride should be used for severe symptomatic hypocalcemia (e.g. hypotension, refractory shock, neuromuscular irritability, psychiatric abnormalities or laryngeal spasm). Call MD for dosing. Calcium chloride, if used, must be given through a central access. Serum IONIZED Calcium Level (mmol/L) 4.3 – 4.4 4.0 – 4.2 3.8 – 3.9 3.6 – 3.7 3.4 – 3.5 3.3 – or below Initiate replacement and call M.D. 8of 12 Dose of Calcium Gluconate 1 gram Calcium gluconate in 50 ml NS over 30 min 2 grams Calcium gluconate in 50 ml NS over 45 min 3 grams Calcium gluconate in 100 ml NS over 1 hour 4 grams Calcium gluconate in 100 ml NS over 90 min 5 grams Calcium gluconate in 150 ml NS over 90 min 6 grams Calcium gluconate in 150 ml NS over 90 min Infusion Rate Over 30 minutes (100 ml/hr) Over 45 minutes (38 ml/hr) Over 1 hour (100 ml/hr) Over 90 minutes (66 ml/hr) Over 90 minutes (100 ml/hr) Over 90 minutes (100 ml/hr) Recheck serum level 4 hours post infusion 4 hours post infusion 4 hours post infusion 4 hours post infusion 4 hours post infusion 4 hours post infusion 736 Battlefield Blvd N, Chesapeake, VA 23320 RENAL POTASSIUM REPLACEMENT ORDERS HYPOTHERMIA THERAPY CRITICAL CARE ONLY Date Ordered Time Ordered 1. Discontinue all previous Potassium replacement orders 2. May give IV or enteral route of administration but not both 3. Enteral route is preferred route for patients without severe hypokalemia or rhythm disturbances. a. Tube feeding must be at goal or patient tolerating full liquid diet b. If dose is greater than 40meq give in divided doses 4 hours apart 4. IV repletion is recommended for potassium levels less than 3.2 mmol/dl 5. Standard Dilution and rate of administration for IV repletion: • Peripheral access: 10 meq/100ml diluents/hour • Central access: 20 meq/100ml diluents/hour or 10 meq/50ml diluents/hour •Central access (fluid restricted 20 meq/50ml diluent 6. Repeat serum potassium level post infusion: 2 hours post IV repletion OR 4 hours post enteral repletion 7. Discontinue Potassium replacement orders upon transfer out of critical care Criteria: •Serum Creatinine greater than 2 mg/dl •OR Serum Creatinine has increased 0.5 mg/dl or more in last 24 hours •OR urine output less than 0.5ml/kg/hr IBW for two consecutive hours RENAL POTASSIUM REPLACEMENT Potassium Level Potassium Replacement Route Peripheral Normal Saline or D5 W Diluent/Volume Central Central Fluid Restricted Length of Infusion 3.7 – 3.8 mmol/L 10meq KCl Enteral/IV 100 ml 50 ml 50 ml 1 hour *DO NOT REPLACE POTASSIUM DURING REWARMING PHASE UNLESS IT IS LESS THAN 3.5 mEq/L* 3.5 – 3.6 mmol/L 3.3 – 3.4 mmol/L 3.2 mmol/L or less 9of 12 20meq KCl 30meq KCl 40meq KCl Enteral/IV Enteral/IV IV 200 ml 300 ml 400 ml 100 ml 150 ml 200 ml 50 ml 100 ml 100 ml 2 hours 3 hours 4 hours 736 Battlefield Blvd N, Chesapeake, VA 23320 RENAL MAGNESIUM REPLACEMENT PROTOCOL HYPOTHERMIA THERAPY CRITICAL CARE ONLY Date Ordered Time Ordered 1. Discontinue all previous magnesium PRN replacement orders 2. Repeat Magnesium level post IV infusion a. 4 hours, if initial level less than or equal to 1.4mg/dl b. In AM, if initial level greater than 1.4mg/dl 3 .Give IV route ONLY 4. Enteral route is preferred route for patients without rhythm disturbances Tube feeding must be at goal or patient tolerating a full liquid diet 5.Discontinue all replacement protocols upon transfer out of critical care Criteria: • Serum Creatinine greater than 2mg/dl • OR Serum Creatinine has increased 0.5mg/dl or more in last 24 hours • OR Urine output less than 0.5ml/kg/hr IBW for last two hours RENAL MAGNESIUM IV REPLACEMENT Level 1.7 or greater 1.5 – 1.6 mg/dl 1.3 – 1.4 mg/dl 1.1 – 1.2 mg/dl 1mg/dl or less 10of 12 Dose (IV) None 1 gram Magnesium Sulfate 2 grams Magnesium Sulfate 3 grams Magnesium Sulfate 4 grams Magnesium Sulfate Diluent/Volume None NS 100 ml Sterile H2O 50 ml NS 100 ml Sterile H2O 100 ml (use 2 doses of 2 grams dosing) Length of Infusion None 30 minutes 60 minutes 90 minutes 2 hours 736 Battlefield Blvd N, Chesapeake, VA 23320 RENAL PHOSPHATE REPLACEMENT ORDERS HYPOTHERMIA THERAPY CRITICAL CARE ONLY Date Ordered Time Ordered 1. If Ionized Calcium less than or equal to 4mg/dl, replace calcium prior to replacing phosphorus 2. Repeat Phosphate Level post infusion: a. 4hours post IV infusion /last enteral dose, if phosphate level less than or equal to 2.2 mg/dl b. In Am post IV infusion/last enteral dose, If phosphate level greater than 2.2 mg/dl 3. Discontinue replacement protocol upon transfer from critical care Criteria: -Serum creatinine greater than 2mg/dl - OR Serum creatinine has increased 0.5mg/dl or more in last 24 hours - OR Urine output less than 0.5ml/kg/hr IBW for last 2 hours RENAL PHOSPHOROUS IV REPLACEMENT Level 2.3 – 2.4 mg/dl 2.1 – 2.2 mg/dl 1.9 – 2.0 mg/dl 1.7 – 1.8 mg/dl 1.5 – 1.6 mg/dl 1.4 mg/dl or less Information Only Sodium Phosphate 1 ml provides 3 mmol phosphate 3 mmol 6 mmol 9 mmol 12 mmol 15 mmol 18 mmol Volume of infusion Length of Infusion Central or Peripheral 50 ml D5W 2 hours 100 ml D5W 4 Hours PHOSPHOROUS ENTERAL REPLACEMENT PROTOCOL- NEUTRA-PHOS Level PO or NG Dose 2.5 – 2.6 mg/dl 1 packet 2.3 – 2.4 mg/dl 2 packets 2.1 – 2.2 mg/dl 2 packets 1.9 – 2.0 mg/dl 2 packets 1.8 mg/dl or less use IV protocol 11of 12 Frequency Times one dose Times one dose Every 2 hours for 2 doses Every 2 hours for 3 doses 736 Battlefield Blvd N, Chesapeake, VA 23320 RENAL CALCIUM REPLACEMENT ORDER HYPOTHERMIA THERAPY Date Ordered Time Ordered 1.Discontinue all previous calcium PRN replacement orders 2.Calcium replacement should be administered if the patient has: a. Ionized calcium 4 or less b. Ionized Calcium greater than 4 but less than 4.5 and exhibiting: 1. Refractory Shock in the setting of sepsis, post-op, massive blood transfusions, status post parathyroid surgery, renal disease, pancreatitis, rhabdomyolysis, unexplained poor cardiac performance 2. Neuromuscular Irritability (tetany, muscle spasms, Chvostek’s or Trousseau’s sign, weakness, hyperactive reflexes, seizures) 3. Psychiatric abnormalities in a previously asymptomatic patient 4. Laryngeal spasm 3. Repeat Ionized Calcium level a. 4 hours post infusion if less than 4 mg/dl and symptomatic b. In AM if greater than or equal to 4 mg/dL 4. Use Calcium Chloride for severe symptomatic hypocalcemia (HYPOTENSION) 5. DO NOT administer calcium and magnesium through the same IV at the same time. 6. Discontinue Calcium replacement orders upon transfer out of critical care. CALCIUM IV REPLACEMENT Serum Bicarbonate (HCO3) OR Serum CO2 less than or equal to 30mmol/L OR Chloride greater than 112mmol/L Level Volume Length of Infusion CALCIUM GLUCONATE (Preferred) 4.3 – 4.4mg/dl 3 grams in 100 ml 60 minutes 4.1 – 4.2mg/dl 4 grams in 100 ml 90 minutes 3.9 – 4.0mg/dl 5 grams in 150 ml 90 minutes 3.8 or less 6 grams in 150 ml 90 minutes Serum Bicarbonate (HCO3) OR Serum CO2 greater than 30 mmol/L. USE CENTRAL LINE ONLY Level Volume Length of Infusion CALCIUM CHLORIDE USE CENTRAL LINE ONLY 4.3 – 4.4 mg/dl 1 gram in 50 ml 30 minutes 3.9 – 4.2 mg/dl 1.5 grams in 50 ml 60 minutes 3.8 mg/dl or less 2 grams in 50 ml 60 minutes 12of 12