Symptom Control Guidelines for patients with End Stage Renal
advertisement

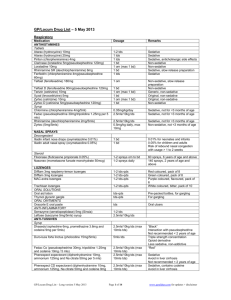
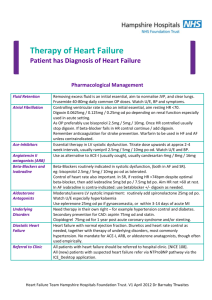
Symptom Control Guidelines for patients with End Stage Renal Failure in the community (eGFR<15) Symptom Dyspnoea Common Causes / Comments Fluid overload (Pulmonary oedema)………………………………………………………………. Metabolic Acidosis………………………………………………………………………………… Pain Nausea/ Vomiting Agitation Itch Restless legs Constipation Anaemia – Hb level can sometimes decrease rapidly causing dyspnoea Avoid NSAIDs* (only give if necessary for pain control AND patient close to dying) Consider underlying cause of pain (eg peripheral vascular disease etc) If prescribing opioids advise: Start a low dose of opioid Avoid slow release preparations of opioid Increase usual dose interval as half life maybe prolonged (eg give prn) Inform patient and relatives of signs of opioid toxicity (drowsiness, confusion, myoclonus) & to call doctor should these occur. Will need early clinical review. Oral opioids: Risk of accumulation and toxicity as all undergo renal excretion. Topical opioids: Fentanyl patches – inactive metabolites, minimal renal excretion but potent so avoid in opiate naïve patients. Buprenorphine patches may also be safe but evidence is limited. Injectable opioids: Alfentanil and Fentanyl are s/c drugs of choice. Short half life when given prn (<1hr). Diamorphine/morphine have risk of accumulation. Uraemia (Nausea is prevalent, constant queasiness) Gastric Stasis (Post prandial intermittent nausea, early satiety, vomiting relieves nausea) Maybe sign is beginning to enter terminal phase. Exclude other causes: eg sepsis, urinary retention, drug side effect, consider hypercalcaemia (CorrCa>2.8mmol/L) or opioid toxicity. Common in ESRF. Exacerbating factors: (1) Dry skin (2) High serum phosphate (>1.5mmol/L) (3) Iron deficiency (Ferritin<100 / MCV<80 / Transferrin sats<20%) - consider IV iron* Common in ESRF. Anaemia exacerbates – consider checking Hb. Management If pt distressed administer midazolam 2.5mg s/c stat. Electric Fan (or breeze) on patient’s face can help alleviate dyspnoea. Furosemide -dose required may be high: max 250mg orally/24hrs*. Consider adding metolozone 2.5mg po alt days*. To monitor response can check daily weights. If poor response after 1 week furosemide can be given s/c by syringe driver over 24hrs to aid absorption*. If appropriate, weekly U&Es, LFTs, Cl & serum bicarbonate check. Check bloods to confirm – if serum bicarbonate <20 mmol/L prescribe Na bicarbonate 500mg po tds* Recheck bloods to assess response 1 week later. If Hb<6gm/dl admission for transfusion may be appropriate* 1st step: Paracetamol 1g po tds 2nd Step: Paracetamol 1g po tds PLUS - for intermittent pain: Either Tramadol IR 50mg po prn max bd OR oxycodone IR (oxynorm) 2.5mg po prn max 8-12 hourly. Cautiously titrate oxynorm dose every few days according to response*. -for constant pain: Buprenorphine 7 day patch 5mcg /hr. NB this is equivalent to approx 5mg of oral oxycodone total dose in 24hrs. 3rd Step: Paracetamol 1g po qds plus Fentanyl 72 hour patch 12mcg/hr. NB this is equivalent to 20mg of oral oxycodone total dose in 24hrs, so is potent. If pain sounds neuropathic or due to muscle spasm consider clonazepam 0.5mg po od as an alternative to opiates. Haloperidol 0.5-1mg po/sc od max tds Metoclopramide 5mg po/sc tds (max 15mg/24hrs) If no treatable cause found Haloperidol 0.5-1mg po max bd +/- Lorazepam 0.5mg po/sl max bd Regular emollient (eg Diprobase topically bd) Adjust phosphate binders*. Itch can be resistant to anti-histamine: (1) Chlorphenamine 4mg nocte-sedative effect may help sleep (max tds) & Ranitidine 150mg po bd (2)Or Ondansetron 4-8mg po max bd often effective-but NB s/e is constipation (3) Or Pregabalin 25mg po nocte Clonazepam 0.5mg po nocte Senna 15mg od & Lactulose 10-20mls max tds If needed, switch lactulose to Na Docusate 200mg max tds. * Please contact renal team for advice: BLT Renal supportive care nurses Mon-Fri 9-5pm (tel 07920595266) Out of hours – contact on call renal registrar via BLT switch (02073777000) Or for symptom control/ terminal care: Contact the local hospice team (see Co-ordinate my Care website for contact numbers) If patient is dying please follow Renal Liverpool care pathway guidelines (see Co-ordinate My Care Renal website) References: ‘Symptom management for the adult patient dying with advanced kidney disease’ Douglas et al Pall Med 2009 23:103, ‘Systematic review of the use of opioids for those with moderate to severe cancer pain & renal impairment’ King et al Pall Med 2011 25: 525







![Antibiotics [pre:Dfreq, post: D dose by 50%]](http://s3.studylib.net/store/data/007446576_1-5f5b3cd9462e3ff75ef61a5b7a0b32d2-300x300.png)