What is an Angioplasty? - St Vincent`s University Hospital

S
T
.
V
INCENT
’
S
U
NIVERSITY
H
OSPITAL
CARDIAC REHABILITATION
DEPARTMENT
Discharge Information
After Your Angioplasty
SVUH PD 12/10 035
Introduction
You have had an angioplasty, which is a serious event, but you will recover and return to enjoy a normal life. The information in this booklet will help you on the road to recovery. It is divided into two sections:
1) Discharge Advice. The discharge advice will guide you through the first few weeks of recovery. It is important to remember that everyone recovers at different rates.
2) Lifestyle Advice. The build up of fatty material or plaque, known as heart disease, is progressive. You can slow down this progression and reduce your risk of further heart problems by changing your lifestyle. It is your responsibility to make and maintain these changes for the rest of your life.
Do not feel you are alone during your recovery. Phone us if you need support or advice.
Marie Minogue/Kathryn O’Sullivan
Cardiac Rehabilitation Nurse Specialists
St Vincent’s University Hospital,
Elm Park, Dublin 4.
Tel: 01-2214957
Fax 01-2094968 www.st-vincents.ie
Discharge Advice after Your Angioplasty
If you had a heart attack prior to your angioplasty, it is essential that you follow the discharge advice for a heart attack. Your cardiac rehabilitation nurse or coronary care nurse will discuss this with you.
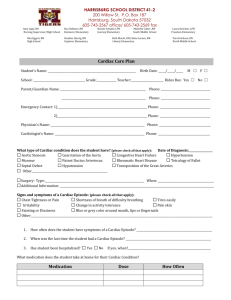
What is an Angioplasty?
An Angioplasty is a procedure used to widen narrowed coronary arteries and to improve the blood supply to the heart muscle. A stent may or may not be inserted during your angioplasty.
What is a Stent?
It is a tiny metal stainless steel tube, which is expandable. The stent is placed in a narrowed coronary artery and expanded to keep this artery open (see diagram below).
Following insertion of the stent there is sometimes a risk of blood cells (platelets) forming a clot around the stent. This risk is reduced by taking the medications Clopidogrel (Plavix) or Prasugrel
(Efient). You should not stop either medication unless directed by a
Cardiologist.
3
Groin/Wrist Puncture Site Care (after an Angiogram or
Angioplasty)
You may experience some tenderness and/or bruising at the puncture site. You should contact your G.P if
The site or limb becomes swollen, pale, cool or numb.
If you develop signs of infection i.e. redness, drainage, heat at the site or a temperature.
If you develop increasing pain, discomfort, tingling or bruising. Some bruising is normal.
If the site starts to bleed you need to apply direct pressure and attend your local Accident and Emergency department immediately.
If you had an Angio-seal closure in the groin you may feels a pea size lump in the area.
Avoid heavy lifting, straining and household chores for a week.
The dressing can be removed the following day or follow the advice of your nurse/doctor.
You may shower. Avoid bathing, swimming pools etc until the skin has healed.
Mood
Initially, on hearing your diagnosis you may go through a range of emotions. You may feel shock, numbness, denial, anger, anxiety, or depression.
About 20% of people report adjustment difficulties following a new cardiac diagnosis; this is normal in patients recovering from a life-changing event. It may manifest as loss of confidence, feeling more irritable or down in yourself or a feeling of panic. Your confidence will return.
Adjustment can take up to a hundred days, so be easy on yourself and keep in touch with the cardiac rehab team. We have specialist psychological support should you require it. Contact the cardiac rehabilitation nurses and they will arrange this for you.
4
Activities
You can usually resume normal light activities within four to five days, once the groin area has healed.
Avoid heavy physical exertion and lifting such as carrying shopping or hoovering for ten days.
Sexual activity can be resumed after a few days, once you are feeling well enough.
Rest and Relaxation
It is normal to feel tired when you go home but this should improve over a week to ten days.
Aim to get at least eight hours sleep each night.
Work
You can resume work after a week or follow the advice of your cardiologist. If you have a strenuous job you may need to extend your leave. If your cardiologist agrees, you may do non-physical work. This should not be stressful.
Chest Pain
After an angioplasty it is normal to have niggles in your chest that last seconds
If you develop chest pain that is not relieved with GTN spray (two puffs, at three minute intervals, to a maximum of three times) do not hesitate to call an ambulance on 999 or 112 from your mobile.
Even if the pain is relieved by GTN spray you need to consult your
GP that day .
Do not drive with chest pain and pull over before taking GTN spray.
Possible side effects of GTN spray include dizziness and/or headache. If you get dizzy staying sitting and stop taking the GTN spray. Phone an ambulance if the pain persists.
Remember if you are getting any chest pain tell your doctor immediately.
5
Driving
You can drive after one week unless your cardiologist says otherwise. This advice is different if you drive a commercial vehicle, taxi, bus or truck and you will need specific advice from your cardiologist.
You must inform your vehicle insurance company that you had an angioplasty to ensure your insurance will be valid.
You should also inform the Driving Licence Authority
It may take longer than a week before you feel confident to drive.
Attending the Dentist
Inform your dentist about your medications especially Aspirin,
Clopidogrel (Plavix), Prasugrel (Efient) or Warfarin.
It is not necessary to take preventative antibiotics after an angioplasty.
Travel
Flying is not recommended for a week, however if essential, follow the advice of your cardiologist.
Make sure you obtain adequate travel insurance. You are obliged to inform the travel insurance company of your heart condition and any pre-existing illness.
Bring a list of your medication with the generic names i.e.
Atorvastatin (generic name), Lipitor (brand name) and doses or photocopy your prescription.
Carry an extra week’s supply of medication.
Put medication in hand luggage in case your luggage gets lost.
General Advice
Drink water/juice for twenty-four hours to help your body get rid of the angiogram dye.
You may find that you bleed more easily as a result of the blood thinning medication. If you cut yourself, apply direct pressure to the wound until it stops bleeding.
You may feel more sensitive to the cold. Dress appropriately for the weather.
6
Lifestyle Advice after an Angioplasty
When recovering from a heart event your lifestyle changes are important.
The Cardiac Rehabilitation Nurses/team and Coronary Care Nurses will discuss this with you, either in hospital or when they meet you after a few weeks.
Smoking
If you are a smoker, giving up is the most important thing you can do to avoid further heart problems.
If you need assistance, there is a smoking cessation service available in the hospital. Talk to the doctors/nurses if you are interested in information or advice and they will organise this for you.
Alternatively, you can ring the Smoking Cessation Service on 01-
2214958.
Exercise
It is essential that you exercise following your angioplasty. Exercise will reduce your risk of developing further heart problems.
Below is the exercise regime to follow (from the day you leave hospital):
This is a walking programme, as walking is the easiest exercise to take up. You can go out two to three times in the day if you wish.
Week 1: 5-10 minutes at a time.
Week 2: 10-15 minutes at a time.
Week 3: 15-20 minutes at a time.
Week 4: 20-30 minutes at a time.
Week 5: Aim for 30-45 minutes walk most days of the week.
If you are limited by joint pain or a medical/surgical condition please speak to your doctor, nurse or physiotherapist. Remember to listen to your body. You should always be able to talk while you are exercising. This is the ‘walk talk test’, a simple test to ensure that you are exercising within you limitations.
If you plan to attend the Cardiac Rehabilitation programme in St
Vincent’s University Hospital, you will be invited to education sessions facilitated by a nurse and a physiotherapist, who will advise you on how best to exercise at this stage.
7
Cholesterol
Find out what your cholesterol level is. These are the current recommendations although they may vary according to your consultant. o Total Cholesterol less than 4.5 mmol/L o LDL ‘Bad’ Cholesterol less than 1.8 mmol/L o HDL ‘Good’ Cholesterol greater than 1.0 mmol/L for a man
greater than 1.2 mmol/L for a woman. o Triglycerides less than 1.7 mmol/L
A healthy lifestyle will help improve your cholesterol level.
Take your medication as prescribed.
Healthy Eating
Enjoy a low-fat diet, choosing from a wide variety of foods.
If you received specific dietary advice, try to follow it.
Include plenty of fruit and vegetables, aim for five servings a day.
Chicken and fish are healthy choices.
Lean red meat three or four times a week is okay.
Eat oily fish (such as salmon, mackerel, sardines, trout, and herrings) twice a week (fresh or tinned).
An egg a day is okay, if you have raised cholesterol limit eggs to 4-6 per week.
Use low-fat spreads and low-fat/light milk.
Use less salt. Choose other flavourings instead; pepper, herbs, spices, vinegar, mustard and garlic.
Intake of caffeine containing drinks should be in moderation.
Keep chocolate, sweets, cakes, crisps and biscuits for treats/special occasions and have a small amount.
Avoid frying. Grill, bake, poach, microwave, dry roast, steam or stir-fry in very little oil. Vegetable oil such as sunflower, corn, soya, rapeseed, or olive is a healthy option when used in small amounts.
8
Weight
Being overweight or obese is a risk factor for heart disease.
Start by following the advice regarding healthy eating and exercise.
Use the information in this booklet as a guide to change your eating habits and start a regular exercise programme.
Small consistent changes can make a big difference.
Use this Chart to check if you are a Healthy Weight or if you need to lose some weight.
9
Waist Size
The higher your waist measurement, the greater your risk of developing diabetes and heart disease.
Ideal waist size Increased risk Greater risk
Female Less than 32” (80cm) 32-35” (80-88cm) More than 35” (88cm)
Male
Less than 37”(94cm)
37-40” (94-102cm)
More than 40”(102cm)
Alcohol
Avoid drinking to excess on any one occasion.
Drink in moderation and preferably with meals.
Taking cardiac medication and alcohol is generally safe, but avoid taking both at the same time.
The recommended guidelines for adults is
Up to 11 standard drinks per week for women
Up to 17 standard drinks per week for men.
Examples of a standard drink include
1 pub measure of spirits (35.5mls)
1 small glass of wine (12.5%)
Half pint of normal beer
Blood Pressure
If you have high blood pressure it is important to take your medication as prescribed.
Eat a healthy low-fat diet, with 5 portions of fruit and vegetables daily.
Avoid salt or reduce your salt intake as much as possible.
Include 3 portions of calcium rich foods per day (1 portion = 1 glass of milk or 1 pot of yoghurt or 1oz (28g) of cheese). Use low-fat options.
Maintain a healthy weight.
Exercise daily.
Learn to relax and to manage your stress.
10
Medication
Get your discharge prescription filled the day you leave hospital and be careful not to miss a dose.
It is important to take your medication as prescribed.
Don’t stop taking any medication without first consulting your doctor.
Take your medications with cold water only.
Grapefruit can interfere with medications therefore avoid grapefruit or grapefruit juice.
A prescription is valid for six months at the most. Your GP will renew your prescription after that .
Please refer to “Step by Step through Heart Medicines” for any queries regarding medication (available in CCU/ Cardiology and The
Irish Heart Foundation) or consult your pharmacist.
On Discharge
Outpatient Appointment
You will receive an outpatient’s appointment by post. If you do not receive a date for this appointment, please contact the ward secretary on 01-2214295. If you have concerns in the interim contact your GP.
Cardiac Rehabilitation Follow-up
If you choose to attend this hospital for cardiac rehabilitation the cardiac rehabilitation nurse will contact you a few weeks after going home and invite you to meetings with a nurse and a physiotherapist. The six-week exercise and education programme will follow where you will also meet a dietitian, pharmacist and psychotherapist.
Please note this information is intended as a guide only. If necessary, follow individual advice given by your doctor or nurse.
11
Marie Minogue/Kathryn O’Sullivan
Cardiac Rehabilitation Nurse Specialists
St Vincent’s University Hospital,
Elm Park, Dublin 4.
Tel: 01-2214957
Fax 01-2094968 www.st-vincents.ie
Date:
Revision Date:
August 2012
August 2014
V5 SVUH COMPHYS21
12