The economic case for renewing Ireland`s healthcare infrastructure
advertisement

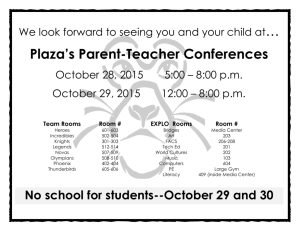
The Economic Case for Renewing Ireland’s Healthcare Infrastructure Professor Roger S. Ulrich Dept of Architecture, Texas A & M University Director Centre for Health Systems & Design November 2008 2 Introduction This briefing document has been prepared by Professor Roger Ulrich for the Hospice Friendly Hospitals (HfH) Programme which is an initiative of the Irish Hospice Foundation in partnership with the Health Service Executive. The HfH Programme, which is supported by The Atlantic Philanthropies, The Health Services National Partnership Forum and the Dormant Accounts Fund, has three key objectives: To develop standards for end-of-life care in hospitals To develop the capacity of hospitals to introduce and implement these standards To change the culture of hospitals regarding end-of-life issues The work of the programme is focused around four key themes: Integrated Care; Communication; Design & Dignity; Patient Autonomy. In May 2007, shortly after the launch of the HfH Programme, Tribal Consulting was commissioned to undertake a review of the physical environment of hospitals participating in the programme. The results of the review provided cause for concern, most particularly with regard to: the lack of facilities for private consultations and conversations in situations where confidentiality is paramount; the extent to which already very limited single-room accommodation is denied to the dying and their families because of the priority given to infection control and isolation; the lack of facilities for families; the poor quality of mortuary facilities. The issues raised in the report have been referred to in the Joint Statement on Endof-Life Care for Older People in Acute and Long-Stay Care Settings in Ireland from the National Council on Ageing and Older People and the Irish Hospice Foundation (June 2008). This statement indicated that ‘One of the significant barriers to good quality end-of-life care is the physical and sensory environment in acute hospitals, psychiatric hospitals and voluntary hospitals/homes’. It asserted that ‘hard questions must be asked about how we plan the physical environment in facilities where significant numbers of people are known to die’ and specifically asked: Why do some facilities not provide the physical environment needed to allow their residents to live and to die in dignity, for example with only thin curtains separating the living from the dying, those eating from those using a commode? Why are so many older people allowed to die in busy wards against a background of noise from other patients, televisions, etc? (Keegan et al., 1999) Why are appropriate facilities not provided for the dying and amenities for those who accompany the dying in their last hours? The review undertaken by Tribal Consulting for the HfH Programme, and the associated literature review, was referred to in the Report of the Commission on Patient Safety and Quality Assurance ‘Building a Culture of Patient Safety’ (July 2008). The Commission indicated that it was ‘..persuaded by such evidence as has been made available to it and by submissions made on this issue that the implementation of evidence-based design will result in safer and higher quality care for patients, with resultant economic benefits for the health system’. 3 Conscious that Ireland has been described as having ‘one of the worst physical health infrastructures of any country in the developed world’ and that, even in good economic times, the problem of the physical environment of our hospitals has not been seen as a priority by either government or opposition parties or indeed by many health related advocacy groups, the HfH Programme has sought to develop a positive agenda based on building an awareness of the importance of high quality healthcare environments and the related clinical, social and economic benefits. The HfH agenda includes: building the capacity of hospital and network-based work groups to appreciate and engage with issues relating to the design, layout and organisation of the physical environment; providing resources to assist hospital staff engage in practical projects in specific areas as part of the process of implementing improvements linked to standards development; supporting the development of exemplar projects so that health care staff and planners can visit and learn from examples of good practice; promoting a clear focus on design related issues in the context of all new service plans and policy developments; proposing a grants scheme to encourage small scale improvements in existing hospitals. Most importantly the HfH Programme has, with the active involvement of HSE Estates, health care professionals and hospital user representatives, developed Design & Dignity Guidelines for Physical Environments of Hospitals Supporting Endof-Life Care (June 2008) The HfH Programme believes that the unit of accommodation in hospitals should be a room, rather than a bed, and that sharing a room with others at the end of life should, in so far as is possible, be a matter of choice for all concerned. Our concerns are shared, from differing perspectives, by many others. Consequently, there is now an opportunity to link the agenda of the hospice movement with the agendas of health care providers, quality and risk managers, infection control experts, health economists, specific illness organisations, patient advocacy groups, political parties and the social partners. This briefing document, prepared by Professor Ulrich, makes the economic case for renewing Ireland’s healthcare infrastructure and, in doing so, addresses one of the commonest concerns which has been expressed in the course of discussions to date, namely, that good healthcare infrastructure is not possible on the grounds of financial cost. 4 HEALTHCARE OUTCOMES IMPROVED BY EVIDENCE-BASED DESIGN AND BETTER BUILDINGS Evidence-based design yields substantial annual savings How can investment in new healthcare buildings be justified during a time of economic uncertainty and limited funds? A peer-reviewed business analysis concluded that building a new 300-bed U.S. hospital with comprehensive evidencebased design upgrades would add 5.3% to the initial construction costs (Berry et al., 2004). However, conservative estimates of costs savings and gains in revenue suggested that the one-time additional construction costs would be recaptured in only one year. Furthermore, the savings stemming from the design improvements would recur annually over many years of operation of the hospital. In several countries, a rising tide of litigation and compensation linked to infection outbreaks, falls, and medical errors has created another compelling fiscal justification for building safer and better hospitals. A recent analysis suggests that the economic case for building better hospitals has been further strengthened by the adoption of pay-for-performance policies in countries such as the U.S. and Britain (Sadler et al., 2008). If government payers or insurance entities withhold payment to hospitals when preventable events occur such as falls and certain infections, the business case for design measures that reduce such events (single rooms, for example) is powerfully enhanced. Given this business case, health authorities would be shortsighted and irrational to forego rebuilding of healthcare infrastructure for fiscal reasons. Rather, authorities should seize the opportunity to invest in evidence-based design and better buildings as a means for improving the financial condition of the health system, and most importantly the health and safety of patients and staff (Ulrich, 2006). The sections below list several health and safety outcomes, and discuss specific evidence-based building design measures that can improve each outcome and thereby generate cost savings. Reduce hospital-acquired infections Hospital acquired infections are a major contributor to escalating care costs and one of the leading causes of death. Aging or obsolete healthcare buildings facilities hinder the prevention and control of infections. A large amount of scientific research strongly supports the following design measures for reducing hospital acquired infection: Provide single-bed rooms with private toilets to enable separation or isolation of patients on admission, so that those with unrecognized infections will not be mixed in with uninfected patients in multibed rooms; to reduce airborne infection transmission by increasing isolation capacity and facilitating good air quality through measures such as ventilation, air flow direction and pressure, and filtration; and to facilitate thorough cleaning after a patient leaves (Ulrich, 2004; Ulrich and Wilson, 2006; Ulrich et al., 2008). 5 Design and maintain the water system at the proper temperature and adequate pressure; and stagnation and back flow should be minimized. To increase handwashing compliance install alcohol-based hand-rub dispensers at the bedside and locate handwash basins close to staff movement paths in visually prominent locations near work points (Ulrich and Wilson, 2006; Ulrich et al., 2008). Strong evidence indicates that air filtration in combination with single rooms reduces the incidence of infection and mortality among immunocompromised and other vulnerable patient groups, thereby lowering care costs. Reduce falls Falls are an increasing problem that produce physical injuries, longer stays in hospitals, and substantially increase care costs. A study of 34,972 patients found that 7.2 % experienced at least one fall during hospitalization, which increased their length of stay by an average of 13.1 days (Schwendimann, 2006). There is considerable evidence that bedrails are ineffective for reducing falls and often increase the severity of injuries caused by falls from hospital beds. Design to provide good visual access to patients. Most falls occur when patients are not observed and/or unassisted. Visual access to patients in multibed rooms is often blocked by drawn privacy curtains. Research indicates that designing wards to provide very good visual access from nursing stations and corridors to patients’ bed and rooms can effectively reduce falls, because nurses can quickly identify needs of the patients and provide immediate assistance. One study suggests that design to provide excellent visual access from hallway nurse stations via windows may reduce falls by 25% (Vassallo et al., 2000). Design to support family presence. Limited evidence has linked family presence in patient rooms to fewer falls, because the presence of family appears to reduce the risk that patients will get out of bed unassisted or unobserved. Providing single rooms to support family presence, in combination with localized nurse charting stations with direct visual access to beds (via hallway windows) can cut falls by two-thirds (Hendrich et al., 2002, 2004) thereby markedly reducing injuries and costs. Reduce medical errors A limited but growing amount of research shows that appropriate environmental design can play an important role in reducing frequent, harmful, and costly medical errors. Increase lighting and reduce distractions. Medication dispensing and other errors can be reduced significantly by providing relatively high levels of worksurface lighting, and designing work spaces to reduce distractions and interruptions. 6 Shorter distances to medication storage reduce errors.. A risk assessment of several medication dispensing scenarios concluded that shorter distances from patient rooms to medication storage reduces the risk that clinicians will bypass procedures and access medications for multiple patients, thereby reducing errors such as giving a patient a medication intended for another patient (Institute for Healthcare Improvement, 2004). By comparison, centralized location of medications increases nurse walking and can worsen patient safety by increasing medication dispensing errors. Provide single-bed rooms to improve several outcomes and lower longterm costs The evidence-based design intervention that positively affects the largest number of outcomes in hospitals, including care costs, is the provision of single-bed rooms (Ulrich, 2006; Ulrich et al., 2008). Because of the many well-documented advantages of single-bed rooms, the American Institute of Architects 2006 Guidelines for Design and Construction of Health Care Facilities recommends that in new general hospitals “the number of beds per room shall be one” (American Institute of Architects and Facilities Guidelines Institute, 2006, p. 40). Also, a recent evidence-based report issued by the National Association of Children’s Hospitals and Related Institutions (NACHRI, 2008) recommends that single rooms should be provided for nearly all patients in pediatric facilities. It was earlier emphasized that single rooms are important for reducing transmission of hospital-acquired infection. Also, much research has shown that single-bed rooms, compared to multibed accommodation, more positively impact other outcomes as described below. Single rooms substantially lessen noise, thereby reducing patient stress and improving sleep (studies reviewed in Ulrich et al., 2008). Sleep deprivation hinders the healing process and contributes to increased morbidity and costs by impaired immune function, delirium, disrupted thermoregulation, and ventilatory compromise (Wallace et al., 1999). Single rooms reduce harmful and costly patient transfers. Multibed rooms generate more transfers of patients between rooms because incompatibility among patients is a frequent problem. Detrimental aspects of patients transports identified by much research include adverse effects on patient stability and outcomes, worsened rates of cross-infection, increased medication errors, manual lifting injuries to staff, demand for staff time, high costs, and increased length of stay (Ulrich and Zhu, 2007; Ulrich et al., 2008; Hendrich et al., 2004; Institute of Medicine, 2004). Single rooms, by eliminating transfers related to roommate incompatibility (such as when one patient becomes infected), improve safety and several other outcomes and produce substantial cost savings (Berry et al., 2004; Sadler et al., 2008). Single rooms are far superior to multibed rooms for enhancing dignity and privacy. The absence of roommates helps prevent privacy breaches during discussions between patients and care staff (Ulrich et al., 2008). Patients in single rooms are more willing to provide personal information to care providers, which facilitates diagnosis, effective treatment, and improved outcomes (Barlas et al., 7 2001; Mlinek and Pierce, 1997). Other research has found that nurses perceive single rooms to be more appropriate than multibed rooms for patient examinations, collection of medical histories, and protecting patient dignity (Chaudhury et al., 2006). A high percentage of single rooms prevents the stressful and demeaning problem of mixed-gender accommodation. Single rooms are superior for supporting family presence. Compared with multibed rooms, single rooms are more likely to provide space and furniture to accommodate visiting relatives (Chaudhury et al., 2006) and to permit flexible visiting hours. Single rooms also greatly increase privacy for patient-family communication and social support. Nursing staff who have experience with both single and multibed rooms judge singles to be better for accommodating family (Chaudhury et al., 2006). Single rooms enhance communication between clinical staff and patients. Patients in single rooms report consistently higher satisfaction with communication from physicians and nurses compared with patients in multibed rooms cared for by the same staff (Press Ganey, 2003). Kaldenburg (1999) found that clinicians in multibed rooms are reluctant to discuss patient issues or give information when they are within earshot of a roommate, out of respect for patient privacy. Single rooms increase patient satisfaction. A vast amount of sound data provides unequivocal evidence that patients in single-bed rooms in American hospitals, compared to patients with one or more roommates, are consistently and substantially more satisfied with the overall quality of their care (e.g., Press Ganey, 2003). A study sponsored by NHS Estates at a large English hospital (Lawson and Phiri, 2003) found that 93% of patients who had experience with both single and multibed rooms preferred having a single room. Single rooms compared to multibed rooms increase flexibility in managing bed availability (Lawson and Phiri, 2003), and promote better patient flow and efficiency per bed (Hendrich et al., 2004). Reduce pain Pain is a pervasive, serious, and costly problem that can be reduced by designing healthcare buildings to provide: Exposure to daylight. Rigorous research suggests that patients experience less pain and take significantly fewer costly analgesic medications, when the building orientation and patient room design provide exceptional exposure to daylight. A study by Walch et al. (2005) suggests that designing hospitals to increase daylight exposure can reduce pain medication costs by 20% for patients undergoing surgery, compared to the costs for comparable patients assigned to shaded rooms. Views of nature. Exposing patients to views of nature can produce substantial and clinically important alleviation of pain (Malenbaum, Keefe, Williams, Ulrich, & Somers, 2008). Design that provides patients with window views of nature, access to gardens, and exposure to nature art and pictures, can alleviate pain and emotional duress, and reduce care costs. 8 Alleviate depression and shorten stays by designing for daylight exposure Higher room daylight exposure shortens stays of depressed patients. A large body of rigorous evidence indicates that exposure to light -- daylight or bright, full-spectrum artificial light -- is effective in reducing depression and improving mood, even for persons hospitalized with severe depression (Golden et al., 2005). Medical studies have reported that hospitalized patients with depression can have more favorable recovery outcomes, including shorter and less costly stays, if they are assigned to sunnier rooms rather than rooms that receive less daylight or are always in shade. A study found that patients hospitalized for depression stayed an average of 3.7 days less if they were assigned east-facing rooms exposed to morning light, compared to patients in west-facing rooms with less sunlight (Benedetti et al., 2001). Beauchemin and Hays (1996) found that adult patients hospitalized for severe depression in a Canadian facility had shorter stays by an average of 2.6 days if they were assigned to sunny rooms rather than rooms that were always in shade. Higher room daylight may shorten stays of female MI patients. Depression is a serious problem not only for mental health patients, but also for several other categories of patients, such as those with cardiovascular disease and cancer. An investigation of myocardial infarction patients in an intensive care unit in a Canadian hospital suggested that female patients had shorter stays (1.1 days shorter) if their rooms were sited to provide higher versus lower daylight exposure (Beauchemin and Hays, 1998). In the same study, mortality in both sexes was lower in sunnier rooms than in north-facing rooms. Reduce noise to improve several outcomes and lower care costs Sound-absorbing ceilings reduce incidence of rehospitalization of cardiac patients. Along with other proven acoustic performance enhancements (providing single rooms and reducing noise sources) installation of high performance soundabsorbing ceiling tiles contributes to reduced noise and improved outcomes. Published research suggests that the installation of high performance soundabsorbing ceiling tiles alone can produce substantial savings in caring for cardiac patients by reducing the incidence of rehospitalization of myocardial infarction patients by approximately 30% to 45% within three months after initial discharge (Hagerman et al., 2005). Reduce noise to improve outcomes in neonatal intensive care. Several studies of infants in neonatal intensive care units (NICUs) have reported that higher noise levels elevate blood pressure, heart and respiration rates, and decrease oxygen saturation, thereby increasing need for oxygen support therapy (Slevin, Farrington, Duffy, Daly, & Murphy, 2000). These negative effects on outcomes foster longer, more costly hospital stays in newborn intensive care. Along with eliminating and reducing noise sources such as medical equipment, installation of high performance sound-absorbing ceiling tiles contributes to reduced noise and promotes improved outcomes in NICUs (White et al., 2006). 9 Reduce noise to lessen intake of pain medication. There is limited evidence that sound-absorbing ceilings may also contribute to lower costs by reducing intake of pain medication by surgery patients. Sound absorbing ceiling tiles and other noise reduction measures increase patient satisfaction. When high performance ceiling tiles were installed in a coronary critical care unit (CCU), noise levels declined and patients reported they were significantly more satisfied with care quality -- compared to when low performance ceiling tiles were in place (Hagerman et al., 2005) Design that reduces noise diminishes staff work stress and perceived demands. Nursing staff perceive higher sound levels on wards as stressful and interfering with their work (Bayo et al., 1995; Norbeck, 1985). Topf and Dillon (1988) reported that noise-induced stress was linked to emotional exhaustion or burnout among critical care nurses. A rigorous, prospective study by Blomkvist et al. (2005) in a Swedish hospital demonstrated that installing high performance soundabsorbing ceiling tiles (versus lower performance tiles) substantially reduced perceived work demands, and lowered work pressure and stress. Ceiling mounted patient hoists cut costly staff injuries Several studies have shown that the pervasive and very costly problem of staff lifting injuries can be substantially reduced by providing ceiling mounted patient hoists. Research also has found that ceiling lifts, compared to portable hoists, are more effective in reducing injuries and require less time and space to use (Hignett and Evans, 2006; Keir and MacDonell, 2003). Two studies of ceiling lifts installed in single patient rooms have reported that the initial cost was paid back within 2.5 years or less by savings stemming from fewer staff manual lifting injuries (Chhokar et al., 2005; Joseph and Fritz, 2006). Design ward layouts to improve patient safety and outcomes, and reduce costly attrition of nurses Ward floor layouts in older hospitals generally provide long corridors organized around a central nursing station, where medication and charts are located, and central locations for supplies and medications. Considerable research has shown that nurses therefore spend much of their time (more than 40% in older UK NHS hospitals) walking up and down halls engaged in wasteful activity such as fetching supplies, thereby increasing fatigue and stress, eroding job satisfaction, and sharply cutting the time available for observing patients and delivering direct care (Hendrich, 2003; Institute of Medicine, 2004; Ulrich, 2006). Studies in the U.S. and Britain indicate that hospitals with obsolete floor layouts severely hamper nurse work efficiency, and limit staff to providing only about 16-24 minutes of care time per patient during an eight-hour work shift. Wards designed according to modern evidence-based principles greatly increase nurse time for observation and care of patients. Evidence-based ward floor layouts provide single-bed rooms and decentralized nurse charting stations with viewing windows to improve safety, outcomes, and reduce costs by fostering direct 10 observation of vulnerable patients. Research suggests that closer location of supplies to patient rooms also is important because centralized supply location can double staff walking and seriously reduce patient care time (Hendrich, 2003; Institute of Medicine, 2004). Such properly designed wards substantially reduce staff walking and fetching time, increase time for observation and care of patients, and heighten nurse work satisfaction (Institute of Medicine, 2004; Hendrich et al., 2004; Ulrich, 2006). Importantly, there is good evidence that well-designed wards with single rooms and decentralized nurse charting and observation do not require higher nurse staffing levels than traditional multi-bed units, and can reduce costly nurse attrition by up to 50% (Hendrich et al., 2004; Institute of Medicine, 2004). Research References American Institute of Architects and Facilities Guidelines Institute (2006). Guidelines for Design and Construction of Health Care Facilities. Washington, DC: American Institute of Architects. Barlas, D., Sama, A. E., Ward, M. F., & Lesser, M. L. (2001). Comparison of the auditory and visual privacy of emergency department treatment areas with curtains versus those with solid walls. Annals of Emergency Medicine, 38(2), 135-139. Bayo, M. V., Garcia, A. M., and Garcia, A. 1995. Noise levels in an urban hospital and workers' subjective responses. Archives of Environmental Health 50(3):247251. Beauchemin, K. M., and Hays, P. (1996). Sunny hospital rooms expedite recovery from severe and refractory depressions. Journal of Affective Disorders, 40(1–2), 49–51. Beauchemin, K. M., and Hays, P. (1998). Dying in the dark: Sunshine, gender and outcomes in myocardial infarction. Journal of the Royal Society of Medicine, 91, 352–354. Benedetti, F., Colombo, C., Barbini, B., Campori, E., and Smeraldi, E. (2001). Morning sunlight reduces length of hospitalization in bipolar depression. Journal of Affective Disorders, 62(3), 221-223. Berry, L. L., Parker, D., Coile, R. C., Hamilton, D. K., O’Neill, D. D., and Sadler, B. L. (2004). The business case for better buildings. Frontiers of Health Services Management, 21, 3-24. Blomkvist, V., Eriksen, C. A., Theorell, T. Ulrich, R. S. and Rasmanis, G. (2005). Acoustics and psychosocial environment in intensive coronary care. Occupational and Environmental Medicine, 62, 132-139. Buchanan, T. L., Barker, K. N., Gibson, J. T., Jiang, B. C., and Pearson, R. E. (1991). Illumination and errors in dispensing. American Journal of Hospital Pharmacy, 48(10), 2137–2145. Chaudhury, H., Mahmood, A. and Valente, M. (2006). Advantages and disadvantages of single versus multiple-occupancy rooms in acute care environments. Environment and Behavior, 37(6), 995-999. Chhokar, R., Engst, C., Miller, A., Robinson, D., Tate, R. S., and Yassi, A. (2005). The three-year economic benefits of a ceiling lift intervention aimed to reduce healthcare worker injuries. Applied Ergonomics, 36(2), 223-229. Diette, G. B., Lechtzin, N., Haponik, E., Devrotes, A. and Rubin, H.R. (2003). Distraction therapy with nature sights and sounds reduces pain during flexible 11 bronchoscopy: A complementary approach to routine analgesia. Chest 123(3), 941948. Golden, R. N., Gaynes, B. N., Ekstrom, R. D., Hamer, R. M., Jacobsen, F. M., Suppes, et al. (2005). The efficacy of light therapy in the treatment of mood disorders: A review and meta-analysis of the evidence. American Journal of Psychiatry, 162(4), 656–662. Hagerman, I., Rasmanis, G., Blomkvist, V., Ulrich, R., Eriksen, C. A., and Theorell, T. (2005). Influence of intensive coronary care acoustics on the quality of care and physiological state of patients. International Journal of Cardiology, 98(2), 267-270. Hendrich, A., Fay, J., and Sorrells, A. (2002). Courage to heal: Comprehensive cardiac critical care. Healthcare Design, 11–13. Hendrich. A. (2003). Optimizing physical space for improved outcomes: Satisfaction and the bottom line. Paper presented at the Impact Conference, Institute for Healthcare Improvement and The Center for Health Design, Atlanta, GA. Hendrich, A. L., Fay, J., and Sorrells, A. K. (2004). Effects of acuity-adaptable rooms on flow of patients and delivery of care. American J. of Critical Care, 13(1), 35–45. Hignett, S., and Evans, D. (2006). Spatial requirements in hospital shower and toilet rooms. Nursing Standard (Royal College of Nursing, Great Britain), 21(3), 43– 48. Institute for Health Improvement (2004). FMEA: Comparison of Five Medication Dispensing Scenarios. Boston, Massachusetts: Institute for Healthcare Improvement. Institute of Medicine (2004). Keeping patients safe: Transforming the work environment of nurses. Washington, DC: National Academies Press. Joseph, A. and Fritz, L. (2006). Ceiling lifts reduce patient-handling injuries. Healthcare Design, 6(1), 10-13. Kaldenburg, D. O. (1999). The influence of having a roommate on patient satisfaction. Press Ganey Satisfaction Monitor, January/February (www.pressganey.org). Keir, P., and MacDonell, C. (2003). Muscle activity during patient transfers: A study on the influence of lift assists and experience. Ergonomics, 47(3), 296–306. Kozarek, R. A., Raltz, S. L., Neal, L., Wilber, P., Stewart, S., and Ragsdale, J. (1997). Prospective trial using Virtual Vision® as distraction technique in patients undergoing gastric laboratory procedures. Gastroenterology Nursing, 20 (1), 12-18. Lawson, B. and Phiri, M. (with J. Wells-Thorpe) (2003). The Architectural Healthcare Environment and its Effects on Patient Health Outcomes. Report sponsored by NHS Estates. London: TSO. Lewy, A. J., Bauer, V. K., Cutler, N. L., Sack, R. L., Ahmed, S., Thomas, K. H., et al. (1998). Morning vs evening light treatment of patients with winter depression. Archives of General Psychiatry, 55(10), 890–896. Malenbaum, S., Keefe, F. J., Williams, A. C., Ulrich, R. S., and Somers, T. J. (2008). Pain in its environmental context: Implications for designing environments to enhance pain control. Pain, 134, 241-244. Miller, A. C., Hickman, L. C., and Lemasters, G. K. (1992). A distraction technique for control of burn pain. Journal of Burn Care and Rehabilitation, 13(5), 576-580. Minckley, B. (1968). A study of noise and its relationship to patient discomfort in the recovery room. Nursing Research, 17, 247-250. Mlinek, E. J., & Pierce, J. (1997). Confidentiality and privacy breaches in a university hospital emergency department. Academy of Emergency Medicine, 4(12), 1142-1146. 12 NACHRI (National Association of Children’s Hospitals and Related Institutions) (2008). Evidence through innovation: Transforming children’s health through the physical environment. Alexandria, VA: NACHRI. Norbeck, J. S. (1985). Perceived job stress, job satisfaction, and psychological symptoms in critical care nursing. Research in Nursing & Health, 8 (3), 253-259. Press Ganey, Inc. (2003). U.S. national satisfaction data for 2003 comparing patients with versus without a roommate. Press Ganey, Inc., South Bend, Indiana. Sadler, B. L., DuBose, J., and Zimring, C. (2008). The business case for building better hospitals through evidence-based design. Health Environments Research & Design, 1(3), 22-39. Schwendimann, R. (2006). Patient falls: a key issue in patient safety in hospitals. Unpublished Doctoral Dissertation, University of Basel, Zurich, Switzerland. Slevin, M., Farrington, N., Duffy, G., Daly, L., and Murphy, J. F. (2000). Altering the NICU and measuring infants' responses. Acta Paediatrica, 89(5), 577-581. Topf, M., and Dillon, E. (1988). Noise-induced stress as a predictor of burnout in critical care nurses. Heart Lung 17(5):567-574. Tse, M. M. Y., Ng, J. K. F., Chung, J. W. Y., and Wong, T. K. S. (2002). The effect of visual stimuli on pain threshold and tolerance. Journal of Clinical Nursing 11(4), 462-469. Ulrich, R. S. (2004). Evidenced-based design for patient safety. In: The Environment for Care – Delivering the Best Environment for Care. NHS Estates Report. London: TSO, pp. 14-18, 35-36. Ulrich, R. S. (2006). Evidence-based healthcare architecture. Lancet, 368: S38-S39. Ulrich, R. S. and Wilson, P. (2006). Evidence-based design for reducing infection. Public Service Review: Health (UK), 8: 24-25. Ulrich, R. S. and Gilpin, L. (2003). Healing arts. In S. B. Frampton, L. Gilpin and P. Charmel (Eds.), Putting Patients First: Designing and Practicing Patient-Centered Care. San Francisco: Jossey-Bass, 117-146. Ulrich, R. S., Lundén, O. and Eltinge. J. L. (1993). Effects of exposure to nature and abstract pictures on patients recovering from heart surgery. Psychophysiology, 30 (Supplement 1), 7. Ulrich, R. S. and Zhu, X. (2007). Intra-hospital transport of patients and medical complications: Implications for architectural design and research. Health Environments Research & Design, 1(1), 31-43. Ulrich, R. S., Zimring, C., Quan, X. and Joseph, A. (2006). The environment’s impact on stress. In S. Marberry (Ed.), Improving Healthcare with Better Building Design. Chicago: Health Administration Press, 37-61. Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H-B., Choi, Y-S., Quan, X., and Joseph, A. (2008,). A review of the research literature on evidence-based healthcare design. Heath Environments Research and Design, 1(3), 101-165. Vassallo, M., Amersey, R. A., Sharma, J. C., and Allen, S. C. (2000). Falls on integrated medical wards. Gerontology, 46(3), 158-162. Walch, J. M., Rabin, B. S., Day, R., Williams, J. N., Choi, K., and Kang, J. D. (2005). The effect of sunlight on post-operative analgesic medication usage: A prospective study of patients undergoing spinal surgery. Psychosomatic Medicine, 67, 156–163. Wallace, C. J., Robins, J., Alvord, L. S., and Walker, J. M. (1999). The effects of earplugs on sleep during exposure to simulated intensive care unit noise. American Journal of Critical Care, 8(4), 210-219. White, R. D. (2006). Recommended standards for newborn intensive care unit (NICU) design. Journal of Perinatology, 26, (3), S2-S18.