Antibiotics - California Science Teacher
advertisement

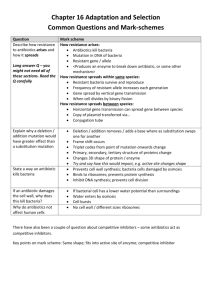
Bio-Ethics of Antibiotic Use and Research Hazel Chun AP Biology Per. 1 06/11/10 Ever since antibiotics were first used in the 1940’s, new resistant strains of bacteria were constantly forming. This process eventually lead to the question, “Are the effects of antibiotic use and research more helpful or harmful to public health?” Bacteria are unicellular organisms (prokaryotes) that are the most abundant organisms found on the planet Earth. These organisms inhabit every corner of the world and even within the human body. Certain types of bacteria live even within the digestive tract of animals and help them digest food and increase the amount of nutrients the body absorbs. Another type of bacteria which are called nitrogen fixing bacteria, live within the soil and supply nitrogen to plants. In addition to the plethora of helpful bacteria, there are bacteria that cause harmful effects to animals, and in this particular case, humans. These disease causing agents are called pathogens. Some examples of sickness in humans caused by bacterial pathogens are pneumonia, tetanus, and tuberculosis. Antibiotics help in killing harmful bacteria or inhibit the growth of bacteria within the body. As the use of antibiotics increased through time, the emergence of many bacterial diseases and illnesses were lowered greatly but this has lead another dilemma. Bacteria reproduce quickly, and what doesn’t kill them only makes them stronger. Meaning, bacteria that are not killed by an antibiotic can quickly reproduce passing off its ability of resistance to offspring and continually make people sick. When harmful bacteria enter the body, they usually secrete toxins into the body killing the cells of its host. Some secrete endotoxins which are defined as components of the outer membrane of a certain gram negative bacteria which is released only when the bacteria dies (Campbell & Reece 546). Another type of toxin secreted by bacteria are exotoxins. Exotoxins are proteins that destroy the cells of its host by disrupting the natural way the cells function and goes through its life cycle. Once toxins are released, they spread fairly quickly via the bloodstream and become difficult to get rid of. Other times, bacteria may invade a host cell where it would be undetected by the immune system. This is what causes the symptoms of illnesses. Usually, the body’s own immune system releases antibodies to combat the bacteria and prevent further spread of the toxins and other pathogens, but when the body’s defenses are not effective, people put antibiotic drugs to use. These drugs alter the way bacteria function. Different bacteria react differently to different antibacterials. Antibiotics are classified based on they types of bacteria it is effective on, whether it is bactericidal or bacteriostatic, and if it can defeat either gram-positive, gram-negative or both. Bactericidal antibiotics kill bacteria; while bacteriostatic reverse the growth of bacterial colonies (Mayer). When an antibiotic is put to work, it deals with two types of bacteria classified as either gram-positive or gram-negative. Gram-negative bacteria have simple cell walls made up of peptidoglycan. These types of bacterial pathogens are more susceptible to antibacterials because their cell walls can be easily altered or destroyed. Gram-negative bacteria have an additional layer of membrane on top of the peptidoglycan layer which contains lipopolysaccharides. Lipopolysaccharides are toxic so both the body’s natural immune system and antibiotics are less effective. Antibiotics often kill gram-positive bacteria by altering the cell walls of pathogens. They prevent or alter the “cross linking of the molecules within the cell wall” (Gilroy). The cell walls of the bacteria are very crucial to a bacteria’s survival so if it is not functioning correctly due to a mishap of its form the function changes, and the bacteria cannot survive. In gram-positive bacteria, cross links are composed of peptidoglycan which is a network of modified sugar polymers cross linked by peptides. When antibiotics prevent these cross links from forming properly, the bacteria lyses. For gram negative bacteria, antibiotics use other methods to destroy the bacteria. A good example of a gram-negative killing antibacterial would be streptomycin. Streptomycin binds to a subunit of a ribosome within a bacterium and inhibits the process of protein synthesis (Todar). Some are also known to inhibit the synthesis of RNA and or DNA. When a bacterium is not affected by an antibacterial drug, it is deemed resistant to the antibiotic. When an antibacterial is used, it may not kill all the pathogens. The few that survive are the ones that have a gene to withstand the effects of an antibacterial. If the remaining bacteria are not dealt with, they will pass on their genes with the use of various mechanisms and reproduce creating a new colony that cause the same illness as the original population, but now the same treatment from before is rendered maladjusted to the new strain. In other words, the bacterium has become resistant to the antibiotic. Bacteria have a number of ways becoming resistant and passing on its gene for resistance other than directly producing offspring. Bacteria can gain resistance on its own by mutating randomly in hopes of gaining a gene that codes for resistance. Other mechanisms used to get resistance involve the role of another bacterium that already has the gene for resistance. One such mechanism is called conjugation. During conjugation, a bacterium with resistance (F+) extends a special of type pilus called a sex pilus and attaches to another bacterium lacking resistance (F-). After the pilus is attached, one bacterium transfers DNA to the other in the form of plasmids. The DNA that has been transferred is a special type of DNA is called a plasmid. Plasmids are small, circular, self replicating DNA molecules that carry only a few genes (most which are essential only for the production of sex pili, and resistance) (Campbell & Reece 349). The plasmid is transferred to the bacteria (F-) as a single strand, and upon entering, the plasmid reverts back to its original circular form and turns the bacterium into F+. Although it is through the use of antibacterials that resistant strains form, research has still continued and antibiotics are still vastly used. They are a necessity in current society and cannot easily be eradicated. Research is desperately needed to constantly form new drugs to combat the ever evolving bacteria, and antibiotics are used for numerous reasons. But with this constant cat and mouse chase between new drugs and new mutations, scientists are trapped in a never ending cycle. This cycle has the science community on edge about practicing the use and research of antibiotics. Michael R. Mulvey, PhD and Andrew E. Simor, MD say “the emergence of antibiotic-resistant organisms is a major public health concern, particularly in hospitals and other health care settings. Antibiotic-resistant organisms appear to be biologically fit and are capable of causing serious, life-threatening infections that are difficult to manage because treatment options are limited.” Doctors are carelessly prescribing antibiotics to colds that are caused by viruses and are not affected by the drugs. Another problem arises in hospitals by patient to patient transfer of resistant bacteria. Hospitals are also one of the few places in society in which antibiotics of all types are heavily relied upon used and ironically as a result, they are a “focal point for the emergence and spread of antibiotic-resistant pathogens” (Kolef and Fraser 298-314). Every time a new resistance is formed a new antibiotic is needed. Many scientists support research of antibacterials and further use of them because they are essential to healthy lives. They fight off infections and the more that is known about bacteria and the antibacterials used to fight them, the safer people are from infections. Thomas Gootz explains that, “vigilance in understanding the mechanisms by which bacteria become resistant to existing antibiotics will lay the groundwork for finding new agents that escape resistance.” His opinion is that to beat the bacteria one must know all about how it interacts with antibacterials to put a stop to resistant strains. The organizations SHEA and HICPAC feel that, “monitoring multidrug-resistant organisms (MDROs) and the infections they cause in a healthcare setting is important to detect newly emerging antimicrobial resistance profiles, to identify vulnerable patient populations, and to assess the need for and effectiveness of interventions” (Vol. 29 No. 10 ,2008). In a research experiment that observed the role of antibiotics in pancreatitis, Ramsay and Breedveld feel that the use antibiotics should be used to help control the infection. Although the antibiotic is not crucial to treating the condition, Ramsay and Breeveld believe that the patients “should receive antibiotic prophylaxis” because it attributed to preventing multi-organ system failure and ultimately death (351-353). Without the continuation of research, new antibiotics would not be engineered to fight the resistant strains currently alive. Other researchers and doctors in the field feel that experiments must be conducted to find treatments to current bacterial infections and diseases. They are aware of the consequences that may come about as a result of constant experimenting, but they feel the benefits outweigh costs. The general public also supports the use of antibacterials to the extent which is becoming a problem. A couple examples are ingesting antibiotic drugs for any symptom of sickness and constant use of disinfectant products on almost all surfaces, objects and food. In contrast to those in support of antibacterial usage and research, there is quite a handful against the idea. These scientists and medical experts do not feel that experimenting around with different antibacterials is worth the risk of potentially forming yet another resistant bacteria. The top risk of experimenting with antibiotics is that it “carries a risk of increasing selection pressure for resistance” (Ramsey and Breedveld). If a research project to create a new antibiotic goes well, everyone benefits. If not, the bacteria targeted is still creating illness in people and the experimental drug may have had an effect on another pathogen that was not meant to be altered. Aside from research, the uses of antibiotics themselves are not openly welcome. In the pro/con paper of the use of antibiotics to help treat pancreatitis Blackbourne and Cohn explain that the trials “found no significant differences in organ dysfunction or mortality” (351-353). Their message is that the continual use of an antibiotic that may or may not be helping the chances of patient’s wellness is not worth using until a definite answer is known about its role. There are many solutions and measures that can be taken to control this quickly growing issue. The best way is prevention, but when that fails, it is important to take quick action. Places like hospitals can establish specific protocol when dealing with the use of antibiotics and monitor known strains of resistance in bacteria. The Centers for Disease and Control (CDC) has published guidelines in reference to the way antibiotics should be handled. This should be strictly followed. When a resistant strain of bacteria is found within a patient, they should be isolated to keep the bacteria from spreading to others. Doctors should also be more aware and careful about prescribing antibiotics so freely. They should only prescribe antibiotic drugs if there is a definite diagnosis to the illness instead of using antibiotics as the first and last options. Doctors should promote the use of antibiotics only when the infections are bacterial, as opposed to viral. Even if these precautionary rules are instated, some bacteria will undoubtedly slip through the cracks and form resistance. This calls for a fast and accurate development of a new antibacterial by pharmaceutical companies. But this is not easy to do because the development of a new drug costs much time and money, which is why many companies have taken a back seat to antibacterial research. Many funds are invested into the formation of one drug, and if it turns out to be ineffective, all the investments are considered to have been wasted. Much resistance may occur through clinical means like in labs and such, but much of it is caused the by public and their constant use of antibiotics without knowing what antibiotics actually do or the possible consequences. The public at large can freely purchase antibiotics on their own accord. This makes controlling the usage of antibiotic difficult to regulate. A vitally effective way of attacking resistant bacteria is to use more that one drug at once to ensure that all of the pathogens are destroyed. But this has a drawback in that it may result in MDROs. A solution to help lessen the problem that is going at in the moment (as opposed to preventing it), would be to put out incentives for antibiotic research. Due to the cost of engineering antibacterials and considering there is guarantee the product will work, many companies have stopped funding antibacterial research. With incentives like funding and easier access to conduct research, scientists will be more drawn to help study resistant bacteria and engineering new antibiotics. Another way to keep bacteria at bay is, once a new drug has been formed to defeat a previously resistant bacteria, it should be closely monitored incase of future mutations. Although all these measures can help reduce the issue at hand, nothing can completely stop it because of two main reasons. The first one is that antibiotics are crucial to the well being of the majority of humans and animals alike. The second reason is that mutations occur spontaneously and randomly. There is no way to control mutations so the only thing to do is to be prepared at all times. Antibiotic research is a risky business but it is essential. The constantly mutating bacteria need a form of antibiotic to keep the numbers at bay. Without antibiotic research, there would be no way to combat future bacterial illnesses because all of then would have become to the current drugs being used now. While it is important to reward new advances in antibiotic research with incentives, it is equally important to set strict policies and procedures for when research is being conducted. The CDC’s guidelines should be adopted and followed by all hospitals. Researchers should keep a sharp eye out in case a bacterial colony is somehow spread out of the lab and into society and also for mutated strains that pop up during the course of their research. Bacterial mutations will occur whether antibiotics are used or not, but the use of antibiotics slightly speed up the process. This is why research must be very carefully planned out and drug testing should be put off until the last division of an antibacterial research project. Society is in need of antibiotics and the research of antibiotic research, but can do well with better organization. The way research is conducted, how and when antibiotics are used and the proper protocol to follow when dealing with resistant strains of bacteria (in hospital and labs) need to be properly addressed and put in order. Works Cited Campbell, Neil A., and Jane B. Reece. "Chapter 27: Prokaryotes ." AP Edition Biology. San Francisco: Pearson, Benjamin Cummings, 2005. Print. Gilroy, William G. "Discovery Sheds Light on the Nature of the Bacterial Cell Wall and How Antibiotics Work." Lumen. Notre Dame University, 8 Apr. 2006. Web. 10 June 2010. <http://www.nd.edu/~lumen/2006_04/HowAntibioticsWork.shtml>. Kollef, Marin H., and Victoria J. Fraser. "Antibiotic Resistance in the Intensive Care Unit." Annals of Internal Medicine 134.4 (2001): 298-314. Annals of Internal Medicine. American College of Physicians. Web. 10 June 2010. <http://www.annals.org/content/134/4/298.abstract>. Mayer, Dr. Gene. "Antibiotics- PROTEIN SYNTHESIS, NUCLEIC ACID SYNTHESIS AND METABOLISM." Biomedical Sciences Graduate Program. University of South Carolina, 17 Feb. 2010. Web. 11 June 2010. <http://pathmicro.med.sc.edu/mayer/antibiot.htm>. Mulvey, Michael R., and Andrew E. Simor. "Antimicrobial Resistance in Hospitals: How Concerned Should We Be?" Canadian Medical Association Journal (2009): 408-15. National Center for Biotechnology Information. 17 Feb. 2009. Web. 10 June 2010. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2638041/?tool=pubmed>. Ramsay, Graham, Lorne H. Blackbourne, Stephen M. Cohn, and Paul Breedveld. "Pro/con Clinical Debate: Antibiotics Are Important in the Management of Patients with Pancreatitis with Evidence of Pancreatic Necrosis." The Critical Care Forum 7.5 (2003). National Center for Biotechnology Information. 17 Mar. 2003. Web. 10 June 2010. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC270709/>. Campbell, Neil A., and Jane B. Reece. “Chapter 18: The Genetics of Viruses and Bacteria." AP Edition Biology. San Francisco: Pearson, Benjamin Cummings, 2005. Print Shlaes, David M. et al. "Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: Guidelines for the Prevention of Antimicrobial Resistance in Hospitals." Infection Control and Hospital Epidemology 18.4 (1997): 275-91. www.shea-online.org. Web. 10 June 2010. <http://www.sheaonline.org/Assets/files/position_papers/AntimicroResist97.PDF>. Todar, Kenneth. "Antimicrobial Agents in the Treatment of Infectious Disease." Online Textbook of Bacteriology. Web. 11 June 2010. <http://www.textbookofbacteriology.net/antimicrobial_4.html>.