Allergy Care Pathways Project: Anaphylaxis Working Group
advertisement

Allergy Care Pathways Project
Anaphylaxis Pathway – final draft v16
Table of Contents
National Care Pathway ...........................................................................................................................1
Anaphylaxis ............................................................................................................................................1
Methodology ...........................................................................................................................................3
Recommendations .................................................................................................................................7
Research Priorities .................................................................................................................................8
Care Pathway for Children with Anaphylaxis .......................................................................................9
Conflict of interest ................................................................................................................................15
References ............................................................................................................................................16
Appendix 1: Glossary...........................................................................................................................20
Appendix 2: Evidence Table: systematic reviews and primary research .........................................21
Appendix 3: Evidence Table: Guidelines ............................................................................................27
National Care Pathway
Allergic conditions constitute the commonest cause of chronic disease in childhood and affect upwards
of 20% of the population. They seriously impair quality of life and health of children and occasionally
can lead to death. Children and young people who experience allergic conditions often received
different levels of care which can affect health outcomes and interfere with schooling. The 2006
Department of Health review of allergy services recommended that there was a specific need to define
care pathways for children with allergic conditions.
The terminology and format for care pathways is wide and varied. Critical pathways, care paths, clinical
pathways are all patient focussed tools that provide the sequence and timing of actions to achieve
patient outcomes with the greatest efficiency [20]. Integrated care pathways are important because they
help to reduce unnecessary variations in patient care and outcomes [21].
The RCPCH has been commissioned by the Department of Health to develop 6 national care pathways
for children with allergies. It is the intention of the Project Board to develop ideal evidence based
national care pathways that are adopted for local use. These pathways will focus on standardising the
level of care received by children with allergic conditions and defining the competences required to
provide a high quality service.
The Allergy Care Pathways Project Board recommends that all locally adopted care pathways should be
implemented by a multidisciplinary care team with a focus on improving services for children with
allergic conditions. One important factor in implementing the care pathway is the use of audit tools to
analyse unnecessary variations in care.
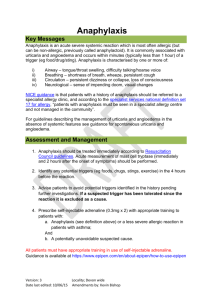
Anaphylaxis
Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction which is
characterised by rapidly developing life-threatening respiratory and/or circulation problems; it is usually
associated with skin and mucosal changes [22;23].
Understanding the epidemiology and disease burden posed by anaphylaxis is important in order to
develop insights into risk factors for its aetiology, and inform service provision and resource allocation
decisions. Accurately characterising the epidemiology of anaphylaxis is however complicated by
inconsistencies in disease definition [23] and the challenges in undertaking prospective cohort studies for
a disorder that is relatively infrequent, and in which disease episodes are typically short-lived and are in
the majority of cases self-limiting [24]. There is as a consequence concern about under-reporting,
Page 1
v15
under-recognition and under-diagnosis of anaphylaxis, this further complicating any reliable assessment
of its frequency or impact. This is important because despite the overall good prognosis, fatalities do
occur, most commonly in young people; these fatalities are believed to be largely avoidable with
appropriate emergency and preventative management [24-29].
A variety of data sources have been used in an attempt to estimate the incidence, lifetime prevalence,
morbidity and case fatality ratio associated with anaphylaxis. These have included population surveys,
case records from primary and secondary care, hospital episode statistics, adrenaline prescribing data
and mortality statistics. Whilst all these available sources have some utility, population-based studies are
likely to yield the most accurate data on the epidemiology and disease burden posed by anaphylaxis.
From the population-based data currently available, the incidence rate, where this is defined as the
number of episodes of anaphylaxis that occur in a defined population over a given period of time, is
estimated at between 80-210 episodes per million person-years [24]. Incidence varies by age, gender,
geography and socio-economic position; the usual socioeconomic gradient between adverse health
outcomes and deprivation seems to be reversed [30]. The limited data available on time trends suggests
that the incidence of anaphylaxis has increased over recent decades and this appears in particular to be
due to increases in allergies to foods in children and young people and adverse drug reactions in older
people; greater awareness, recognition, reporting and recording are other possible explanations [30-36].
Anaphylaxis may be triggered by a wide range of factors, but may also occur spontaneously (idiopathic
anaphylaxis). The most common trigger in childhood is food, followed by drug allergy. Anaphylaxis due
to other triggers such as insect venom or exercise is rare [33;37]. The most frequent food triggers in
childhood are peanut and nuts, cows milk, hen egg, fish and shellfish [38;39].
Lifetime prevalence can be defined as the proportion of a defined population known to have experienced
anaphylaxis during their lifetime. A review by a Working Group of the American College of Allergy,
Asthma and Immunology summarised the findings from a number of seminal studies and concluded that
anaphylaxis affects anywhere between 0.05-2.0% of the general population at some point in their lives,
these large variations possibly reflect regional differences in the diagnostic criteria that tend to be used
[40]. More recent work from the UK however suggests that the prevalence in the UK may be lower than
this estimate; interrogation of a large database of GP records suggests that there are an estimated
40,000 people with a clinician-recorded diagnosis of anaphylaxis diagnosis in the UK [35].
The majority of episodes of anaphylaxis are self-managed by patients/carers – often sub-optimally using
antihistamines and/or bronchodilators, but not adrenaline – and many people experiencing episodes of
anaphylaxis will therefore not receive medical attention [41]. A proportion of episodes will result in the
seeking of medical attention, of whom some (estimated at 28-100 hospital admissions per million people
per year) will be admitted to hospital [24;42].
As a potentially fatal condition, anaphylaxis can have a profound impact on quality of life, this impact
extending way beyond the acute phase of the illness. Although still often thought of mainly as an acute
disorder, anaphylaxis should really be considered as a long-term condition [26]. The impact on the
quality of life of carers should not be under-estimated.
There are at present no reliable ways of assessing of who will and will not experience severe episodes,
but in general terms factors such as the speed of onset of the reaction, the dose of allergen required to
trigger a reaction and severe previous reactions are markers of potentially severe future reactions [27].
Those with underlying asthma – especially if poorly controlled – and cardiovascular disease are
particularly at risk of fatal outcomes [24-27;43]. Delay in receiving medical attention and in particular
adrenaline treatment is another key factor that has repeatedly been implicated in fatal episodes [44;45].
The overall case fatality ratio, where this is defined as the proportion of cases of anaphylaxis that prove
Page 2
v15
fatal of anaphylaxis, is estimated at less than 1% in the majority of case series, or in population terms as
between 1-5.5 fatal episodes of anaphylaxis per million population per year [24]. Mortality statistics
obtained for the Department of Health review showed that from 1993 to 2002 there were approximately
10 deaths per year in England and Wales in which anaphylaxis was a contributing cause [46]. Reported
anaphylaxis fatality rates will inevitably underestimate the true incidence due to difficulties in diagnosis
post-mortem. A case review of death certificates for adults and children in the UK recorded up to 20
probable anaphylactic deaths in the UK annually [47].
Methodology
Objectives
The aim of the project was to develop an evidence-based national care pathway for children with
anaphylaxis. The underpinning principle was that the eventual pathway would:
describe the ideal pathway of care for children from the first presentation with suspected
anaphylaxis in any healthcare setting to the desired patient endpoint
be informed by the best available research evidence and, in areas where research evidence is
lacking, by the consensus of a multidisciplinary team of experts
define the steps in pathway on the basis of the competencies of health care professionals rather
than the setting in which the care should be provided
provide a national template to facilitate local review of services for children with anaphylaxis to
ensure consistent high quality care.
Stages of Pathway Development
The pathway was developed by a multi-disciplinary Anaphylaxis Working Group (AWG) chaired by Dr
Andrew Clark and which reported to a Project Board chaired by Professor John Warner.
The AWG included health professionals with expertise in paediatric allergy, allergy nursing, pharmacy,
primary care, secondary care, immunology, dietetics and emergency care and a parent/carer
representative (Table 3). The AWG was supported by a full-time project manager.
There were two face-to-face meetings of the AWG, in September and October 2009 and one telephone
conference in November 2009.
1. Initial mapping
At its initial meeting the AWG mapped out the ideal care pathway for the five key stages: self care,
ambulance care, emergency department (ED) care, inpatient/further care and outpatient
management, including follow up.
2. Evidence Review
A comprehensive evidence review was undertaken to identify the evidence base for a care pathway
for children with anaphylaxis. A PICOS (Patient/Population, Intervention, Comparators, Outcomes
and Studies) approach was used when formulating the search strategy.
Scoping search
An initial scoping search conducted between 3 August and 25 August 2009 focussed on clinical
questions did not provide a comprehensive list of evidence. The full list of clinical questions used in
the clinical questions used in the scoping search can be obtained from the RCPCH Science &
Page 3
v15
Research Department. This strategy was not pursued and a general systematic search for the
overall care of children with allergies was undertaken.
Literature search strategy
A systematic search was conducted between 26 and 27 August 2009; this covered searches in the
Cochrane Library, Medline, the National Guidelines Clearing House, the Scottish Intercollegiate
Network (SIGN) and the National Institute for Clinical Excellence (NICE). An updated final search
will be conducted upon completion of all of the pathways in July 2010.
Search terms were compiled by pearling expert identified papers for keywords. The terms identified
and used included: hypersensitivity, adolescen$, child$, infant and anaphylaxis. A copy of the full
search strategy can be obtained from the RCPCH Science & Research Department. The search was
not restricted by language. In order to collate the most contemporary evidence base the search was
restricted to the period 1 January 1990 – 26 August 2009. The results of the search were compiled in
a Reference Manager library to allow for easy identification of duplicates. There was no systematic
attempt to identify grey literature. Additional papers for inclusion were identified by snowballing the
references of the appraised papers. Handsearching was conducted by working group members.
Inclusion/exclusion criteria
Participants: Children and young people aged 0-18 with anaphylaxis and/or an allergic condition
related to anaphylaxis. Mixed studies were included where it was possible to extract data on children
and young people. Where there was no evidence directly relating to children adult studies were
included on the recommendation of expert opinion, otherwise adult studies were excluded.
Interventions: Studies that included preventative and therapeutic interventions in any setting by any
health professional, including self care.
Comparators: Any comparator, including no comparator.
Outcome measures: The outcomes examined in the review of evidence included symptoms
(mild/moderate/severe), quality of life and mortality.
Studies: Systematic reviews of key interventions and clinical guidelines/guidance based on reviews
of evidence were included. Primary research was considered, including RCTs, non-controlled trials,
case-control studies and cohort studies. Case reviews with more than 3 reports were also considered
where there was no other evidence.
Evidence Appraisal Methods
The evidence was appraised in 3 stages: an initial title review, an abstract and title review and finally
an appraisal.
Stage 1
The project manager initially reviewed 831 titles; this resulted in 199 systematic reviews, primary
papers and guidelines.
Abstracts and titles were then reviewed by the AWG Chair; this resulted in 37 systematic reviews
and/or primary papers and 6 guidelines for appraisal by the AWG members.
Stage 2
Stage 1 was conducted by the AWG Chair who reviewed the 199 titles and abstracts of the clinical
guidelines and papers using 3 measures: meets study criteria (e.g. anaphylaxis), concerned
with/applicable to children and young people and guideline, systematic review or primary research
with original data.
Page 4
v15
This process resulted in 37 systematic reviews and/or primary papers and 6 guidelines for appraisal
by the AWG members
Stage 3 – systematic reviews and primary research
Thirty seven systematic reviews and primary research passing stage 1 and 2 were critically
appraised by two reviewers from the AWG using modified Critical Appraisal Skills Program (CASP)
tools [48]. The CASP tools can be obtained from the RCPCH Science & Research Department.
Data extraction was performed concurrently with the critical appraisal. Conflicts were resolved using
de-identified appraisals and the consensus of the AWG members. All included papers were
synthesised into an evidence table and assigned an evidence level by the AWG according to the
SIGN methodology (Table 1) [49].
This process resulted in the inclusion of 12 papers and an additional 17 papers for review through
snowballing the reference lists. After the completion of the stage 3 appraisal of the systematic
reviews and primary research 19 papers were marked for inclusion.
Stage 3 – guidelines
All documents setting clinical standards and passing stage 1 and 2 were reviewed by the RCPCH
Clinical Standards Team to ensure College standards for endorsement were met as part of the
RCPCH appraisal and endorsement process. One component of this was to appraise the guideline
using a modified version of the AGREE tool [50]. Any methodological weaknesses were highlighted
in the evidence tables and all included guidelines were assigned an appropriate grade accordingly.
Due to time and resource constraints within the project design recommendations from the clinical
guidelines have been accepted verbatim. Methodological weaknesses of each clinical guideline
were highlighted in the evidence table (Table 5).
This process resulted in the inclusion of 4 clinical guidelines. All but one clinical guideline appraised
used the SIGN methodology (Table 2) to grade their recommendations. The Resuscitation Council
UK Guideline [51] used the RCP Concise Guidance to Good Practice [52]; this is highlighted in the
evidence table.
Table 1 Key to evidence statements [49]
Level
Criteria
1++
High quality meta-analyses, systematic reviews of RCTs, or RCTs with a very low risk of bias
1+
Well-conducted meta-analyses, systematic reviews, or RCTs with a low risk of bias
1-
Meta-analyses, systematic reviews, or RCTs with a high risk of bias
2++
High quality systematic reviews of case control or cohort or studies
High quality case control or cohort studies with a very low risk of confounding or bias and a high
probability that the relationship is causal
2+
Well-conducted case control or cohort studies with a low risk of confounding or bias and a
moderate probability that the relationship is causal
2-
Case control or cohort studies with a high risk of confounding or bias and a significant risk that
the relationship is not causal
3
Non-analytic studies, e.g. case reports, case series
4
Expert opinion
Page 5
v15
Figure 1: Methodology of Evidence Review
Literature Review and Expert Opinion
Project Manager
Stage 1: Reference Manager (de-duplication)
[831]
Project Manager
Titles reviewed
[199]
Project Manager/WG Chair
Titles and Abstracts reviewed [43]
Snowballing
reference list of
appraised papers
[17]
WG members
Include [12]
Stage 2:
Guidelines
[6]
Systematic Review/
Primary Evidence:
Stage 2 [37]
RCPCH Clinical Standards Team
WG Chair
Exclude {5}
Include [23]
Include
[4]
Exclude {14}
Exclude
{2}
Critical Appraisal / Data
extraction: Stage 2
Critical Appraisal / Data
extraction: Stage 3
Stage 3:
AGREE
Appraisal
Project Manager, background (5)
WG members, background (5)
RCPCH Clinical Standards Team
Include [7]
Exclude {0}
Include [12]
Exclude {6}
Include [4]
Exclude
{0}
Project Manager
Data extraction
Table 2 Grades of Recommendation [49]
Grade
A
Criteria
At least one meta-analysis, systematic review, or RCT rated as 1++, and directly applicable to the
target population; or
A body of evidence consisting principally of studies rated as 1+, directly applicable to the target
population, and demonstrating overall consistency of results
B
A body of evidence including studies rated as 2++, directly applicable to the target population,
and demonstrating overall consistency of results; or
Extrapolated evidence from studies rated as 1++ or 1+
C
A body of evidence including studies rated as 2+, directly applicable to the target population and
demonstrating overall consistency of results; or
Extrapolated evidence from studies rated as 2++
D
Evidence level 3 or 4; or
Extrapolated evidence from studies rated as 2+
3. Synthesis of Pathway
Defining the pathway
The pathway was developed over two meetings of the AWG. At the first meeting the pathway was
iteratively mapped using expert consensus opinion. This process was initiated by defining the
principal points of entry into the pathway of children with anaphylaxis and then breaking down the
ideal pathway of care into discrete stages from self-care to follow -up. For each of these stages a
number of key components of care were identified. This approach was further developed at the
second meeting using the results of the evidence review to guide the discussion. The pathway
stages were further developed and linked, where possible, to the strength of the evidence, using
colour coding to distinguish those stages underpinned by evidence and those informed by the expert
opinion of the group. The pathway is colour coded according to the assigned SIGN grade [49].
Page 6
v15
Defining the competences
Competences were mapped to the appropriate section of the pathway using three sources:
RCPCH: A Framework of Competences for Level 3 Training in Paediatric Immunology,
Infectious Diseases and Allergy [53]
RCPCH: A Framework of Competences for Training General Paediatricians with an interest in
allergy [54]
Skills for Health National Occupational Standards for Allergy [55]
For each stage of the pathway the group then identified the competencies in one or more of the three
main categories:
the things a health professional should know
the specific skills a health professional should be able to do
the services or facilities the health professional should have access to
The final pathway is in therefore in two sections; an algorithm of the stages of care of the ideal
pathway and the competences, with the evidence referenced, required to deliver the ideal pathway.
4. Stakeholder consultation/External peer review
An initial stakeholder list was constructed by the Project Board. All stakeholders were contacted by
email and invited to review the pathway. Stakeholders were also invited to suggest additional
stakeholders. The pathway document was also made available on a public section of the RCPCH
website between Tuesday 6 October and Thursday 22 October, 2009. All stakeholder comments
were made public on the RCPCH website upon finalisation of the pathway and a full list of the
comments are available from the RCPCH Science & Research Department.
2. Development of recommendations
The AWG recognises that care pathways are not clinical guidelines and therefore do not normally
include recommendations. However the review of the evidence in relation to children with
anaphylaxis led the group to identify 4 key evidence-based recommendations which the group felt it
was important to include in the pathway chapter.
While the SIGN methodology allows for recommendations to be graded the AWG has chosen not to
do this. The evidence table clearly states the evidence levels applied to each paper. A full list of
evidence statements leading to the recommendations can be obtained from the RCPCH Science &
Research Department.
Recommendations
The Anaphylaxis Working Group (AWG) makes 4 key recommendations:
1. Prompt administration of adrenaline by intramuscular injection is the cornerstone of therapy both in
the hospital and in the community.
2. Children and young people at risk of anaphylaxis should be referred to clinics with specialist
competence in paediatric allergies.
3. Risk analysis should be performed for all patients with suspected anaphylaxis.
4. Provision of a management plan may reduce the frequency and severity of further reactions and is a
recommended part of anaphylaxis management.
Page 7
v15
Research Priorities
See: \\filesvr02\research$\RESEARCH\CURRENT PROJECTS\Allergy care
pathways\MEETINGS\Project Board\20091123_Meeting 3\Anaphylaxis Research Priorities.doc
Page 8
v15
Care Pathway for Children with Anaphylaxis
Entry points
Public places
Early years settings
School
Work
Further & Higher education
Home
Family
Self Care
GP/Primary Care
Immunisation clinic
Hospitals
NHS Direct/NHS 24
Emergency 999
i. Recognition that the child is seriously unwell
ii. An early call for help
iii. Early administration of IM injectable adrenaline, if indicated and available
iv. Identification and removal of trigger, if possible
1
Ambulance
Service/
Primary Care2
i. Recognition that the child is seriously unwell
ii. Initial assessment and treatments based on an ABCDE approach
iii. Early administration of IM injectable adrenaline, if indicated and available
iv. Transfer to Emergency Department (ED)
v. Other treatment, if necessary
ED: initial care3
i. Recognition that the child is seriously unwell
ii. Initial assessment and treatments based on an ABCDE approach
iii. Adrenaline therapy if indicated
i. Further treatment, observation and history
ii. Record all possible anaphylaxis triggers
iii. Provide adrenaline injector
iv. Train in use of adrenaline injector
v. Allergy clinic referral
vi. Provide basic avoidance advice
vii. Provide patient group information
ED/inpatient:
further care4
Medical Care5
i. Allergy focussed clinical history and examination5a
ii. Onward referral, if required5b
iii. Undertake investigations5c
iv. Identify trigger and exclude non-relevant triggers5d
v. Risk assessment5e
vi. Assess and optimise management of other allergies5f
vii. Provide trigger avoidance advice5g
viii. Provide dietary advice5h
ix: Communication5i
x. Immunotherapy, if indicated5j
Outpatient
management,
including follow
up
Provide an emergency management package6
i. Provide appropriate emergency medication
ii. Provide emergency treatment plan for future anaphylactic reactions
iii. Train to use emergency medication
School and early years settings care (SEYS)7
i. Adequate SEYS liaison
ii. Train in recognition of anaphylaxis and avoidance of identified trigger
iii. Provide training in the use emergency medication
Provide follow-up care8
i. Review diagnosis and update avoidance advice
ii. Update emergency treatment plan
iii. Repeat school training
GRADE A
Page 9
GRADE B
GRADE C
GRADE D
WORKING GROUP CONSENSUS
v15
Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction which is likely
when all of the following 3 criteria are met:
1. Sudden onset and rapid progression of symptoms
2. Life-threatening airway and/or breathing and/or circulation problems
3. Skin and/or mucosal changes (flushing, urticaria, angioedema)
Ideally all specialists will have paediatric training in line with the principles outlined in the Children's
National Service Framework (NSF) [56].
Children is an inclusive term that refers to children and young people (0-18years).
A specialist allergy clinic is defined by the competences laid out in this document.
The pathway is linear but it is important to recognise the entry points can occur at any part of the
pathway and that the pathway children follow may not be linear.
All deaths from suspected anaphylaxis should be recorded on a National Anaphylaxis Register.
Ref
1
Pathway stage
Self Care
2
Ambulance Service /
Primary Care
3
ED: initial care
4
ED /inpatients further care
5
Medical Care
Page 10
Competence
Know
the signs and symptoms of potential anaphylaxis
to call for help
when and how to administer injectable adrenaline, if indicated
and available
to identify and remove the trigger, if possible
Know:
the signs and symptoms of anaphylaxis
to transfer to the ED in all cases
Be able to
make an initial assessment and treatment based on an ABCDE
approach [51]
administer injectable adrenaline, if indicated
identify and remove the trigger, if possible
provide other treatment, if necessary
Know:
the signs and symptoms of anaphylaxis
Be able to
make an initial assessment and treatment based on an ABCDE
[51]
administer injectable adrenaline, if indicated
Know
to record any suspected trigger(s)
to observe the patient, ideally for 4-6 hours, and understand the
potential for biphasic reactions
to refer to an allergy clinic [57-60] directly, via the GP using a local
clinic or by checking the BSACI website
Be able to
provide ongoing observation and treatment of the episode
provide basic avoidance advice based on the suspected
trigger(s)
provide and train in the use of an adrenaline injector
provide access to patient/parent/carer support group information
This is best provided by a multidisciplinary team including allergy
specialist doctors, specialist nurse(s), paediatric dieticians and
appropriate school nurse liaison for the further management of
v15
Ref
Pathway stage
5a.
Clinical history and
examination
5b
Referral
5c
Investigation – all allergies
5d
Investigation – drug and
venom allergy
Page 11
Competence
children with anaphylaxis [58-61]
Be able to
recognise and distinguish the features of anaphylaxis from less
severe allergic reactions
recognise the clinical features of conditions which masquerade
as anaphylaxis (e.g. panic attacks, vocal cord dysfunction,
hereditary angioedema)
recognise that anaphylaxis can present as ‘asthma’ without any
cutaneous or other features
gather relevant information on exposure to potential triggers (e.g.
anaesthetic chart for GA anaphylaxis)
recognise the clinical features of anaphylaxis induced by
different triggers and appreciate important differences (e.g.
food, venom, drug, exercise induced and idiopathic)
take a full history including important co-morbidities (e.g.
asthma) and psychosocial issues and interpret the findings
examine and interpret findings in relevant body systems
including chest, ENT and skin
Know
to refer children with venom, drug allergy, idiopathic and
exercise induced anaphylaxis to specialist units with appropriate
expertise in investigation and management
to refer onwards if you do not have access to the appropriate
range of diagnostic techniques (refer to boxes 8. and 9.
investigation) or knowledge of their indications, limitations and
interpretation [45;57;58;60]
when to refer to other agencies, e.g. CAMHS
Have access to:
sufficient facilities, practical skill and knowledge to undertake
and interpret investigations including
– mast cell tryptase (know the time course of elevation during
anaphylaxis) [59]
– skin prick testing [59]
– serum specific IgE
– for food allergy - facilities to perform and interpret oral
challenges in a safe and controlled environment
Understand the
relationship between sensitisation and clinical allergy
performance (sensitivity and specificity) of tests for sensitisation
to allergens which commonly cause anaphylaxis
Know
which allergies commonly occur together in the same individual
(e.g. latex and kiwi fruit allergies) and therefore which additional
tests should be performed
that complementary and alternative medicine (CAM) allergy
tests, including kinesiology, serum specific IgG and Vega tests
have no place in the diagnosis and management of anaphylaxis
Be able to
interpret the results of investigations in the context of the clinical
history
Have access to
sufficient facilities, practical skill and knowledge to undertake
and interpret investigations including facilities to perform and
interpret (in a controlled and safe environment) [59]:
– intradermal tests for venom and drug anaphylaxis
– oral or subcutaneous challenges for drug allergy. For venom
v15
Ref
Pathway stage
5e
Identify trigger
5f
Risk Assessment [62]
5g
Assess and optimise
management of other
allergies
5h
Provide trigger avoidance
advice for family members
5i
Provide dietary advice
Page 12
Competence
allergy, understand potential cross reactivity between species
and the relative value of serum specific IgE and skin tests
For drug allergy be able to
exclude allergy to alternative related drugs (e.g. antibiotics and
anaesthetics)
Be able to
synthesise information gathered from history, examination and
diagnostic tests to identify the likely trigger factor
exclude non-relevant triggers which the patient may be
inappropriately avoiding
Know
the natural history of individual food allergies, venom, drug,
exercise induced, and food and exercise induced anaphylaxis to
be able to provide the patient with a reasonable risk assessment
indicating the likelihood of further anaphylactic episodes and the
need for provision of emergency medication
Be able to
recognise potential high risk situations and provide appropriate
advice to minimise the risk
Be able to
appreciate the importance of maintaining good asthma control in
children with anaphylaxis
assess asthma control using history, examination and
investigations (including spirometry)
identify allergic and non-allergic triggers for asthma
recognise that rhinitis control affects asthma and treat
appropriately
give written and verbal advice on reducing allergic triggers
prescribe asthma medication appropriately
provide a written emergency management plan for asthma as
required
Have the relevant skills and information to educate and empower
families on avoidance strategies including
food allergy: be able to provide comprehensive written and
verbal advice based on knowledge of the natural history of the
food allergy and the age of the child. Also, be able to provide
sufficient information to interpret labelling on food and non-food
products.
drug allergy: be able to provide written and verbal advice on
which specific drugs to avoid (main trigger and any crossreacting drugs). Also, the ability to inform the family which drugs
can be tolerated in future.
Venom: be able to provide advice to reduce chance of further
stings including practical measures and information on cross
reacting species.
For exercise induced and food and exercise induced
anaphylaxis be able to provide written and verbal advice on
reducing exposure to predictable high risk situations.
Be able to
provide additional appropriate information on patient support
groups and/or other sources
Have access to
a state registered dietitian competent in dealing with children
with food anaphylaxis
Be able to
recognise the potential effect of food allergen avoidance on
v15
Ref
Pathway stage
5j
Communication
5k
Immunotherapy
6
Emergency management
package for patients, their
families and other carers
[44;57;59;62-64]
7
Schools and Early Years
Settings (SEYS) care
8
Follow up
Page 13
Competence
growth and nutrition
supplement trigger avoidance advice and recommend suitable
alternatives to avoided foods
Be able to
communicate with patients, parents and carers, primary care,
other health care professionals, schools and early years settings
(SEYS) and where necessary social services
Know
how to share appropriate information to support other health
care professionals in performing a risk assessment
Have access to
a specialist unit, with full paediatric resuscitation facilities
the appropriate expertise and experience in performing
immunotherapy
Know
the indications and contraindications for immunotherapy
when to cease immunotherapy
Be able to
select patients appropriately for immunotherapy
Be able to provide an emergency management package that
includes:
a written or electronic emergency treatment plan for future
anaphylactic reactions that includes [57;63]
– contact details [63]
– allergen avoidance advice [44]
– advice on recognising symptoms [63]
– guidance when to use each medication during a reaction [35]
– age, language and psychosocially appropriate information
sources
appropriate emergency medication [26] based on risk
assessment (refer to box 11).
training in the use of emergency medication [35]
provision to review the management plan
repetition of training
Have
adequate liaison with SEYS
Be able to:
advise SEYS on the provision of rescue treatment
train SEYS personnel [65]
– in recognition of anaphylaxis
– on avoidance of identified trigger(s)
– to be able to use emergency medication when appropriate
repeat training annually
Have
facilities and expertise to be able to provide adequate follow up
Know
the natural history of allergy in childhood
Be able to
diagnose new allergies
modify allergen avoidance advice according to new information
adjust the dose of adrenaline injectors according to change in
body weight
update dietetic advice
access trained personnel to update school training as required
detect possible resolution by repeating investigations including
v15
Ref
Pathway stage
Page 14
Competence
allergen challenges if required
update emergency management plan
assess asthma control and adjust therapy as required
inform children and families about the process and appropriate
timing for obtaining a medical identity bracelet
v15
Conflict of interest
Table 3: Conflict of Interest
Name
Representation
Position
Conflict
Dr Andrew Clark
Tertiary Care - Paediatric
Allergist
Paediatric Allergist,
Addenbrookes Hospital
Consultancy: Schering Plough. Member: BSACI
council, BSACI Standards of Care Committee
Dr Mazin Alfaham
Secondary Care Paediatrician
Paediatric Consultant,
University Hospital of Wales
NIL
Dr Pamela Ewan
Secondary Care - Adult
Allergist
Mrs Louise Sinnott
Commissioning/DoH
Allergy Pilot
Adult Allergist, Addenbrookes
Hospital
NW Allergy and Clinical
Immunology Project Manager,
NHS North West Specialised
Commissioning Team
NIL
Dr Ian Maconochie
Emergency
ED Paediatrician, St Mary's
Hospital
Member: Resuscitation Council, UK (RCUK)
Dr Fiona Jewkes
JRCALC
Ms Rosie King
Nursing
Hon Secretary and RCPCH
representative, JRCALC
Allergy Nurse Specialist,
Southampton University
Hospital NHS Trust
TBC
Representative: RCGP/JRCALC on RCUK
Anaphylaxis Guidelines
Member: RCUK Executive
Member: BSACI
Employed by Anaphylaxis UK. Work with the
National Allergy Strategy Group
Member: BSACI
Ms Mandy East
Patient/Parent/Carer
Mr Stephen Tomlin
Pharmacist
Parent Rep, Anaphylaxis
Campaign
Consultant Pharmacist Children's Services, Evelina
Children's Hospital
Prof Aziz Sheikh
Primary Care / RCGP
Professor of Primary Care
Research and Development,
University of Edinburgh
Family members with anaphylaxis. Ongoing
programme of work funded by the Government
and charitable donors in relation to allergic
disorders which include anaphylaxis.
Ms Kate Lloydhope
Project Manager
Project Manager, RCPCH
NIL
Dr Dalbir Sohi
Secondary Care
General Paediatrician, Royal
Free Hampstead NHS Trust
NIL
Dr Susan Leech
Tertiary Care - Paediatric
Allergist
Paediatric Allergist, Kings
College Hospital
Member: BSACI
Paediatric Allergist, St Mary's
Hospital
Lectures/Consultancy: Novartis, Danone,
Airsonelte, Merck, Allergy Therapeutics. Trustee:
Anaphylaxis Campaign (until Jul 2009). Member:
steering committee for BTS/SIGN asthma
guideline. Research Funding/Support: GSK,
AstraZeneca, Merck, Danone, Airsonelte, Allergy
Therapeutics, ALK
Prof John Warner
Page 15
Tertiary Care - Paediatric
Allergist
NIL
v15
References
20
Pearson S, Goulart-Fisher D, Lee T. Critical Pathways as a Strategy for Improving Care: Problems and
Potential. Ann Intern Med 1998; 123:-941.
21
Bandolier. What is an integrated care pathway? Bandolier Journal 2001; 3(3):1-8.
22
Johansson SGO, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF et al. Revised nomenclature
for allergy for global use: report of the Nomenclature review Committee of the World Allergy
Organization, October 2003. J Allergy Clin Immunol 2004; 113:832-836.
23
Sampson HA, Munoz-Furlong A, Campbell RL, Adkinson NF, Bock SA, Branum A et al. Second
symposium on the definition and management of anaphylaxis: Summary report-Second National Institute of
Allergy and Infectious Disease/Food Allergy and Anaphylaxis Network symposium. J Allergy Clin Immunol
2006; 117(2):391-397.
Page 16
24
Chinn D, Sheik A. Epidemiology of anaphylaxis. In: Pawankar R, Holgate S, Rosenwasser L, editors.
Allergy frontiers: Epigenetics, allergens and risk factors. Tokyo: Springer, 2009: 123-144.
25
Bock S, Muñoz-Furlong A, Sampson H. Fatalaties due to anaphylactic reactions to foods. J Allergy
Clin Immunol 2001; 107:191-193.
26
Simons FE. Anaphylaxis, killer allergy: Long-term management in the community. J Allergy Clin Immunol
2006; 117(2):367-377.
27
Simons FE, Frew AJ, Ansotegui IJ, Bochner BS, Golden DB, Finkelman FD et al. Risk assessment in
anaphylaxis: current and future approaches. J Allergy Clin Immunol 2007; 120(1):S2-S24.
28
Simons FE. Anaphylaxis in infants: can recognition and management be improved? Journal of
Allergy & Clinical Immunology 2007; 120(3):537-540.
29
Simons F. Epinephrine autoinjectors: first-aid treatment still out of reach for many at risk in the
community. Ann Allergy Asthma Immunol 2009; 102(403):409.
30
Sheik A, Alves B. Age, sex geographical and socio-economic variations in admissions for
anaphylaxis: analysis of four years of English hospital data. Clin Exp Allergy 2001; 31(10):1571-1576.
31
Gupta R, Sheikh A, Strachan D, Anderson H. Increasing hospital admissions for systematic allergic
disorders in England: analysis of national admissions data. BMJ 2004; 327:1142-1143.
32
Sheikh A, Alves B. Hospital admissions for acute anaphylaxis: time trend study. BMJ 2000; 320:1441.
33
Alves B, Sheikh A. Age specific aetiology of anaphylaxis. Arch Dis Child 2001; 85(4):348.
34
Gupta R, Sheikh A, Strachan D, Anderson H. Time trends in allergic disorders in the UK. Thorax 2007;
62:91-96.
35
Sheikh A, Hippisley-Cox J, Netwon J, Fenty J. Trends in national incidence, lifetime prevalence, and
adrenaline prescribing for Anaphylaxis in England. J R Soc Med 2008; 101:139-143.
36
Simons FE, Sampson HA. Anaphylaxis epidemic: fact or fiction? J Allergy Clin Immunol 2008;
122:1166-1168.
37
Braganza S, Acworth J, Mckinnon D, Peake J, Brown A. Paediatric emergency department
anaphylaxis: different patterns from adults. Arch Dis Child 2006; 91:159-163.
38
Novembre E, Cianferoni A, Bernardini R, Mugnaini L, Caffarelli C, Cavagni G et al. Anaphylaxis in
Children: Clinical and Allergologic Features. Pediatrics 1998; 101(4):e8.
39
Mehl A, Wahn U, Niggemann B. Anaphylactic reactions in children – a questionnaire-based survey in
Germany. Allergy 2005; 60:1440-1445.
40
Lieberman P, Camargo CJr, Bohlke K, Jick H, Miller R, Sheikh A et al. Epidemiology of anaphylaxis:
findings of the American College of Allergy, Asthma, and Immunology Epidemiology of Anaphylaxis
Working Group. Ann Allergy Asthma Immunol 2006; 97:596-602.
41
Webb LM, Lieberman P. Anaphylaxis: a review of 601 cases. Annals of Allergy, Asthma, &
Immunology 2006; 97(1):39-43.
42
Gaeta J, Clark S, Pelletier A, Camargo C. National study of US emergency department visits for acute
allergic reactions, 1993 to 2004. Ann Allergy Asthma Immunol 2007; 98:360-365.
43
Pumphrey RS. Anaphylaxis: can we tell who is at risk of a fatal reaction? Curr Opin Allergy Clin
Immunol 2004; 4:285-290.
44
Kemp AS, Hu W. New action plans for the management of anaphylaxis. Australian Family Physician
2009; 38(1/2):31.
Page 17
45
Sheikh A, Shehata YA, Brown SGA, Simons FE. Adrenaline (epinephrine) for the treatment of
anaphylaxis. Cochrane 2008; 4.
46
Department of Health. A review of services for allergy - the epidemiology, demand for and provision
of treatment and effectiveness of clinical interventions. DH Allergy Services Review Team, editor.
2006. London, Department of Health.
47
Pumphrey RS. Lessons for management of anaphylaxis from a study fatal reactions. Clin Exp Allergy
2000;30, 8: 1144-1150.
48
CASP. Critical Appraisal Skills Program [Online]. [accessed: 26/09/2009] Available from: http://www
phru nhs uk/Pages/PHD/CASP htm 2009. CASP, Public Health Resource Unit, Oxford.
49
SIGN. Annex B: Key to evidence statements and grades of recommendations [Online]. [accessed:
26/09/2009] http://www sign ac uk/guidelines/fulltext/50/annexb html 2009. CASP, Public Health
Resource Unit, Oxford.
50
AGREE Collaboration. AGREE Instrument. [accessed: 26/09/09] Available from: http://www
agreecollaboration org/instrument/ 2001.
51
Resucitation Council (UK). The emergency medical treatment of anaphylactic reactions. Guidelines
for healthcare providers. 2008; 1-50. London, Resucitation Council (UK).
52
RCP. A new series of evidence-based guidelines for clinical management. In: Turner-Stokes L, editor.
Concise Guidance to Good Practice. London: RCP, 2003: 1-12.
53
RCPCH. A Framework of Competences for Level 3 Training in Paediatric Immunology, Infectious
Diseases and Allergy [Online]. [accessed: 05/10/2009] http://www rcpch ac uk/doc
aspx?id_Resource=4355 2008.
54
RCPCH. A Framework of Competences for training general paediatricians with an interest in allergy.
Forthcoming. 2010.
55
Skills for Health. Competence Application Tools [Online]. [accessed: 05/10/2009] https://tools
skillsforhealth org
uk/competence/searchResults?keywords=allergy&level%5B%5D=1&level%5B%5D=2&level%5B%5D=
3&level%5B%5D=4&adv_search x=4&adv_search y=8 2009.
56
Department of Health. National service framework for children, young people and maternity services
[Online]. [accessed: 12/11/09] http://www dh gov
uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4089100 2004.
Department of Health.
57
Clark AT, Ewan PW. Good prognosis, clinical features, and circumstances of peanut and tree nut
reactions in children treated by a specialist allergy centre. J Allergy Clin Immunol 2008; 122(2):286289.
58
de Silva I, Mehr S, Tey D, Tang M. Paediatric anaphylaxis: a 5 year retrospective review. Allergy 2008;
63(8):1071-1076.
59
Mirakian R, Ewan PW, Durham SR, Youlten LJ, Dugue P, Friedmann PS et al. BSACI guidelines for the
management of drug allergy. Clinical & Experimental Allergy 2009; 39(1):43-61.
60
Singh J, Aszkenasy OM. Prescription of adrenaline auto-injectors for potential anaphylaxis--a
population survey. Public Health 2003; 117(4):256-259.
61
Kapoor S, Roberts G, Bynoe Y, Gaughan M, Habibi P, Lack G. Influence of a multidisciplinary
paediatric allergy clinic on parental knowledge and rate of subsequent allergic reactions. Allergy
2004; 59(2):185-191.
62
Muraro A, Roberts G, Clark A, Eigenmann PA, Halken S, Lack G et al. The management of
anaphylaxis in childhood: position paper of the European academy of allergology and clinical
immunology. Allergy 2007; 62(8):857-871.
Page 18
63
Nurmatov U, Worth A, Sheikh A. Anaphylaxis management plans for the acute and long-term
management of anaphylaxis: A systematic review. J Allergy Clin Immunol 2008; 122(2):353-361.
64
Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clinical &
Experimental Allergy 2000; 30(8):1144-1150.
65
Anaphylaxis Campaign. Be AllergyWise - Training for school nurses [Online]. [accessed: 05/10/2009]
http://www anaphylaxis org uk/allergywise aspx 2008. Anaphylaxis Campaign.
Page 19
Appendix 1: Glossary
Acronym
AWG
CAHMS
CAM
CASP
ED
ENT
NICE
NSF
PICOS
RCP
RCPCH
RCUK
SEYS
SIGN
Page 20
Means
Anaphylaxis Working Group
Child & Adolescent Mental Health Services
Complementary and Alternative Medicine
Critical Skills Appraisal Program
Emergency Department
Ear, Nose and Throat
National Institute of Clinical Excellence
National Service Framework
Patient, Intervention, Comparison, Outcome, Studies
Royal College of Physicians
Royal College of Paediatrics and Child Health
Resuscitation Council, United Kingdom
Schools and Early Years Settings
Scottish Intercollegiate Network
Appendix 2: Evidence Table: systematic reviews and primary research
Table 4: Evidence table: systematic reviews and primary research
Bibliographic Reference
Choo, K. and A. Sheikh.
"Action plans for the long-term
management of anaphylaxis:
systematic review of
effectiveness." Clinical and
Experimental Allergy 37.7
(2007): 1090-94
Sheik A, ten Broek WM, Brown
SGA, Simons FE. “H1antihistamines for the
treatment of anaphylaxis with
and without shock.” Cochrane
Database of Systematic
Reviews 2007; 1.
Sheikh A et al. "Adrenaline
(epinephrine) for the treatment
of anaphylaxis." Cochrane 4
(2008)
Ewan P, Clark AT. “Efficacy of
a management plan based on
severity assessment in
longitudinal and case
controlled studies of 747
children with nut allergy:
proposal for good practice.”
Clin Exp Allergy 2005; 35:751756.
Page 21
Study
Systematic
Review
Systematic
Review – Part A
Systematic
Review – Part A
Nested casecontrol (N=112
cases, 112
controls) in
longitudinal
prospective cohort
study of children
with confirmed
peanut or treenut
allergy (N=615)
Quality Assessment
Systematic search for RCT's and
quasi-RCTs conducted in CENTRAL,
Cochrane, Medline and Embase. Mixed
child and adult study. This study
identified no RCTor quasi-RCT
evidence to guide clinical practice.
Systematic search for RCT's and quasiRCTs in CENTRAL, MEdline, CINHAL,
ISI web of science and grey literature
and pre-publication with clear inclusion
and exclusion criteria. Found no RCT
evidence. Evidence presented in the
discussion section of the systematic
review has no clear inclusion and
exclusion criteria .
Systematic search for RCT's and quasiRCTs conducted in CENTRAL,
Cochrane, Medline and Embase. Found
no RCT evidence. However, the
discussion evidence has no clear
inclusion and exclusion criteria listed.
Caseswere well defined (confirmed
diagnosis) and controls were matched
according to sex, age at onset, age at
enrolment and duration of follow up. No
power calculation is reported for the
sample size
Key outcomes
Although there are potential major benefits of routinely issuing anaphylaxis
action plans, there is currently no robust evidence to guide clinical practice.
Pragmatic randomized-controlled trials of anaphylaxis action plans are
urgently needed; in the meantime, national and international guidelines should
make clear this major gap
No high level evidence for or against the use of H1 antihistamines in
anaphylaxis, this may be due to: 1. anaphylaxis is a potentially life threatening
emergency situation. 2. Absence of a universally accepted definition on this
topic.
This review failed to uncover any evidence from prospective, randomized or
quasi-randomized trials on the effectiveness of adrenaline for the emergency
management of anaphylaxis. Conducting research in this area is challenging
due to : 1. The established position of adrenaline treatment making it difficult
to argue for placebo controlled trials, 2. the ethics of obtaining informed
consent in emergency situations, 3. the difficulty in conducted double blind
placebo controlled trials due to the transient nature of adrenaline treatment, 4.
the fact that anaphylaxis usually occurs without warning in non medical
settings, the difficulty in obtaining baseline measurements.
There was an eight fold reduction in reaction frequency after enrolment in the
management plan and a 60 fold reduction in the frequency of severe
reactions. Of mild-moderate reactions 77% required oral antihistamines alone
and 15% no treatment. Children who had follow up reactions had more
frequent and severe reactions pre follow up and were older (median age 13
years). Considerations for criteria for provision of injectable adrenaline were
difficult to devise. Children with mild reactions were not prescribed injectable
adrenaline unless there was ongoing asthma or only traces had ever been
ingested. All patients were asked to carry antihistamines. This study also
provides reassurance about the safety of intramuscular adrenaline.
Level
1+
1+
1+
2++
Bibliographic Reference
Murphy KR, Hopp RJ,
Kittelson EB, Windle ML. “Life
threatening asthma and
anaphylaxis in schools: a
treatment model for school
based programs.” Ann Allergy
Asthma Immunology 2006;
96:398-405.
Prospective
Cohort (78
schools serving
45,000 children,
N=98 children
successfully
treated)
Studying the implementation of a
protocol in schools. Trained staff
collected the data. No statistical
analysis is performed.
Rancé F, Abbal M, LauwersCancès V. “Improved
screening for peanut allergy by
the combined use of skin prick
tests and specific IgE assays.”
J Allergy Clin Immunol 2002;
109(6):1027-1033.
Diagnostic Test:
cross sectional
study of children
with suspected
food
hypersensitivity
(N=363)
Appropriate design with use of negative
and positive controls. Sensitivity and
specificity with confidence intervals
reported.
Page 22
Study
Quality Assessment
Key outcomes
Selected school staff were fully trained. This protocol resulted in students and
staff having more knowledge of severe allergies. For students to return to
school they must have anaphylaxis action plan (AAP) and medication (or a
waiver). Parents expressed a feeling of safety generated by the knowledge
that a rapid response network exists. The protocol has led to early
intervention for severe asthma attacks, anaphylactic events and allergic
reactions. Rapid access to emergency medical care, patient educations and
caregiver education are the key components to make this program successful.
1.The DBPCFC is the gold standard for diagnosing peanut allergy because it
has a sensitivity and a specificity of 100%. 2.In our study the combined use of
the 2 tests made it quite certain that children had peanut allergy when one of
the 2 test results was positive (≥16 mm for the raw SPT and ≥57 kUA/L for the
specific IgE assay) with a sensitivity of 27.7% and a specificity of 100%. 3.A
skin reaction diameter of less than 3 mm combined with a specific IgE assay
result of less than 57 kUA/L totally eliminated the possibility of peanut allergy
(100% NPV). 4.For other raw SPT and specific IgE assay values, there were
always false-positive and false-negative results that made it necessary to
perform an oral food challenge. 5. The clinical history must be taken into
consideration, and a DBPCFC should be undertaken when the history is
suspicious for a reaction. Our study corresponds to the first diagnostic step for
children with suspected food allergies. We did not observe children with
unequivocal histories of anaphylactic shock induced by ingestion of peanut.
This proposed diagnostic strategy must be confirmed in another population
with peanut allergy. 6. In the event of an unequivocal clinical history of
anaphylactic shock triggered by the ingestion of peanut, peanut consumption
must be forbidden, no matter what the values of the SPT and specific IgE
assay. However, when in doubt, a DBPCFC must be performed. A strong
suspicion of peanut allergy despite negative test results should lead to a
DBPCFC under medical supervision and not a return home with no specific
dietary advice. Superior effectiveness of raw extracts over commercial
extracts
Level
2+
2+
Bibliographic Reference
Sporik R, Hill DJ, Hosking CS.
“Specificity of allergen skin
testing in predicting positive
open food challenges to milk,
egg and peanut in children.”
Clin Exp Allergy 2000;
30:1540-1546.
Braganza, SC et al. "Paediatric
emergency department
anaphylaxis: different patterns
from adults." Arch Dis Child 91
(2006): 159-63
Clark AT and Ewan PW.
"Good prognosis, clinical
features, and circumstances of
peanut and tree nut reactions
in children treated by a
specialist allergy centre." J
Allergy Clin Immunol 122.2
(2008): 286-89
de Silva, IL et al. "Paediatric
anaphylaxis: a 5 year
retrospective review." Allergy
63.8 (2008): 1071-76
Page 23
Study
Diagnostic Test:
Prospective
cohort of children
referred to a
tertiary allergy
clinic with
suspected food
allergy (N=467,
with 555 food
challenges)
Retrospective
case series of
children under 16
(N=526,
generalised
allergic reaction,
N=57
anaphylaxis)
Prospective case
series of children
with peanut/nut
allergy (N=785)
Retrospective
case series of
children with
anaphylaxis
(N=117)
Quality Assessment
Positive and negative controls. No
blinding due to the life threatening
nature of anaphylaxis. Sensitivity,
specificity and likelihood ratios reported
with confidence intervals
Key outcomes
SPT cut-off levels will be different according to the clinical context, the allergen
extract used and the age of the child. Positive food challenges were always
seen when the skin weal diameter was greater than a certain size: cow milk, 8
mm; egg, 7 mm; and peanut, 8mm. In children aged less than 2 years these
diameters were correspondingly smaller: cow milk, 6 mm; egg, 5 mm; and
peanut, 4 mm. This implies that weal diameters equal to or greater than these
diameters were 100% specific in defining the outcome of food challenges.
The findings from this prospective study have changed the food challenge
policy of this unit. If a child has on initial evaluation a skin test weal to cow
milk, egg, or peanut exceeding the above defined limits the child is considered
allergic to that food and does not undergo further evaluation.
Those with a lesser skin reactivity are challenged. Children are restudied
annually and challenged according to the skin test results. All children with
adverse reactions to other foods (such as soy and wheat) were the predictive
value of skin testing has not been defined, and in our experience is not as
clear, also require food challenges. However, caution needs to be applied in
extrapolating our results with these allergen extracts to other populations, of
different ages, where different skin test reagents of varying potency, and
different methodologies may be used.
Retrospective case study is a weak
design. No validation of data entry or
cross checking for accuracy of data
inputting.
The annual incidence of paediatric emergency department generalised allergic
reactions was found to be 9.3:1000 presentations, and that of anaphylaxis
was 1:1000 presentations, with prevalence figures of 2.47:1000 and 0.27:1000
paediatric population respectively.
The commonest cause of paediatric emergency department anaphylaxis was
found to be food items, followed by drugs and then insect venom, with
respiratory clinical features predominating
Prospective case series design, which
is a weak study design to guide decision
making. Source of participants was
clinic population, this may introduce
bias.
Retrospective case study is a weak
design. Disease was clearly defined
and information was gathered from
hospital coded notes. Patient exclusion
was clear and strict.
With a comprehensive management plan (detailed written and verbal age
appropriate advice on nut avoidance, provision of emergency medication ,
training of family members in the use of emergency medication, notification of
each child’s school or nursery), accidental reactions were uncommon and
usually mild, most requiring little treatment; 99.8% self-treated appropriately
and 100% effectively. Favourable prognosis for children attending a specialist
allergy clinic with an annual incidence rate for accidental ingestion of peanut
and/or tree nuts after diagnosis of 3%. This rate is substantially lower than
rates in other studies of accidental exposure to peanut alone e.g. 14-55% in
previous studies
1. Most cases presenting with anaphylaxis were experiencing their first
reaction; 2. Most cases were triggered by food consumed at home; 3.
Reactions developed quickly; 4. Although many children received treatment
with adrenaline, treatment was often delayed and given through a sub-optimal
route; 5. Case fatality rate was low.
Level
2+
3
3
3
Bibliographic Reference
du, Toit G. "Food-dependent
exercise-induced anaphylaxis
in childhood." Pediatric Allergy
& Immunology 18.5 (2007):
455-63
Study
Educational series
(case reports)
(N=3)
Quality Assessment
The author presented 3 case reports of
a rare condition. To gain a thorough
evidence based perspective a single
site study, as in this case, is suboptimal.
Gold and Sainsbury. "First aid
anaphylaxis management." J
Allergy Clin Immunol 106.1
(2000): 171-76
Retrospective
telephone survey
of parents of
children with a
history of
anaphylaxis
(n=68)
Case series design, which is a weak
study design. Small number of
participants
Hu W, Grbich C, Kemp A.
“Parental food allergy
information needs: a
qualitative study.” Arch Dis
Child 2007; 92:771-775.
Semi structured
interviews of
parents of
children with food
allergy (48
families, N=84)
Semi structured interviews are a good
way to obtain information needs.
Selection well explained, potential bias
noted, no reasons for declining noted
though.
Page 24
Key outcomes
The diagnosis of food dependant exercise induced anaphylaxis (FDEIA) is
heavily dependent on the clinical history. Allergy tests may need to be
performed to a broad panel of food and food additives. Modified exercise
challenges (performed with and without prior ingestion of food) are frequently
required as allergy test results frequently return low-positive results. A
diagnosis of FDEIA facilitates the safe independent return to exercise and
reintroduction of foods for patients who otherwise may unnecessarily avoid
exercise and/or restrict their diet. The natural history of FDEIA is unknown;
however, a safe return is usually achieved when the ingestion of the causal
food allergen/s and exercise are separated.
Recurrent generalized allergic reactions occurred with a frequency of 0.98
episodes per patient per year and were more common in those with food
compared with insect venom anaphylaxis.
The adrenaline injector device was only used in 29% of recurrent anaphylactic
reactions. Parental knowledge was deficient in recognition of the symptoms of
anaphylaxis and use of the adrenaline injector device, and adequate first aid
measures were not in place for the majority of children attending school.
Those children in whom the adrenaline injector device was used were less
likely to be given epinephrine in hospital and to require subsequent hospital
admission.
The adrenaline injector device is infrequently used in children with recurrent
episodes of anaphylaxis; the reasons for this require further research. It is
likely that parents and other caregivers will require continuing education and
support in first aid anaphylaxis management. When the adrenaline injector
device is used appropriately, it appears to reduce subsequent morbidity from
anaphylaxis.
3 information phases: initial diagnosis, follow-up and milestone. Content
needs: 1. reasoning behind the doctor’s judgments about their child’s allergy,
including the likelihood of anaphylaxis, and the recommended management.
2. basic medical facts and practical advice related to daily management. l
What is anaphylaxis? What is not anaphylaxis? // l Recognising symptoms of
allergic reactions, the timescale of reactions. // l How accidental exposures
occur and how to manage risky situations. // l What to feed your child (rather
than what to avoid), maintenance of nutrition. // l Practical allergen avoidance:
label reading, shopping, cooking, social events, eating out and travel. How to
find allergen-free products. // l When and how to give the adrenaline injector.
Revision of techniques at each visit. // l How to educate extended family, other
carers and adults who may give the child food. // l Risks and benefits of skin
testing and oral challenges. Interpretation of results. // l When follow-up is
required, and why. // l Where more information may be found, e.g. nurse-led
education sessions, consumer organisations, contacting the clinic. // l How to
educate your child. // l Background information about allergy, the relationship
Level
3
3
3
Bibliographic Reference
Study
Quality Assessment
Key outcomes
between asthma, eczema and food allergy, natural history of food allergy.
information delivery: 1. clinic procedures and accessibility (multiple events,
overwhelming, bored child), 2. formats. Written take-home information was
strongly preferred, as it was difficult to recall details about food ingredients and
products, but not as a substitute for talking with a health professional. Parents
also spoke highly of videos. 3. third and most important aspect was the
doctor–parent–child relationship. The most common reasons for seeking a
second opinion were insufficient information provision
Kapoor S et al. "Influence of a
multidisciplinary paediatric
allergy clinic on parental
knowledge and rate of
subsequent allergic reactions."
Allergy 59.2 (2004): 185-91
Case series
(N=52) with
survey parent’s of
children with food
allergy
No comparator group - allergy
management plan was given to all
participants
Pumphrey, R. S. "Lessons for
management of anaphylaxis
from a study of fatal reactions."
Clinical & Experimental Allergy
30.8 (2000): 1144-50
Retrospective
case review of
164 allergic
fatalities of adults
and children
(1992-1998)
Weak study design (case series).
Subjects referred with food allergy were prospectively enrolled in this study.
Parental knowledge was reassessed after 3 months and rate of allergic
reactions after 1 year. The study found benefits of accessing a paediatric
allergy clinic. After one visit to the paediatric allergy clinic, there was a
significant improvement in parental knowledge of allergen avoidance (26.9%,
P < 0.001), managing allergic reactions (185.4%, P < 0.0001) and adrenaline
injector usage (83.3%, P < 0.001). Additionally, there was a significant
reduction in allergic reactions (P < 0.001).
Immediate recognition of anaphylaxis, early use of adrenaline, inhaled beta
agonists and other measures are crucial for successful treatment. Optimal
management of anaphylaxis is therefore avoidance of the cause whenever
this is possible. Predictable cross-reactivity between the cause of the fatal
reaction and that of previous reactions had been overlooked. Adrenaline
overdose caused at least three deaths and must be avoided. Kit for selftreatment had proved unhelpful for a variety of reasons; its success depends
on selection of appropriate medication, ease of use and good training.
Because all food related reactions caused difficulty breathing paramedics had
difficulty in deciding whether to use the protocol for asthma or anaphylaxis
A case series is a weak design. No
confidence intervals around calculated
parameters were reported.
Children with allergies should be treated in an allergy clinic. Also showing
effect of allergy on quality of life. Set out to assess the quality of training that is
provided for parents with children who were given adrenaline auto-injector,
adherence to recommendations regarding where these children should be
treated, and effect of allergy on quality of life. Training provided was very
poor. Almost 50% were not assessed in allergy clinic. 14.9% of children were
bullied as a result of their allergy. 28% of parents felt that their child could not
do something they really enjoyed as a result of the allergy, and 36.4% of
parents felt that their own lifestyle was affected.
Singh, J. and O. M.
Aszkenasy. "Prescription of
adrenaline auto-injectors for
potential anaphylaxis--a
population survey." Public
Health 117.4 (2003): 256-59
Page 25
Cross sectional
case series postal
survey of parents
of children
prescribed with
adrenaline injector
(N=154)
Level
3
3
3
Bibliographic Reference
Kemp, A. S and W. Hu. "New
action plans for the
management of anaphylaxis."
Australian Family Physician
38.1/2 (2009): 31
Nurmatov U, Worth A, and
Sheikh A. "Anaphylaxis
management plans for the
acute and long-term
management of anaphylaxis: A
systematic review." J Allergy
Clin Immunol 122.2 (2008):
353-61
Study
Quality Assessment
Comment
No methodology for the development of
the anaphylaxis management plans is
outlined.
Systematic
Review
Systematic search for conducted in
Medline, Embase, Science Citation
Index, Cochrane, , ISI proceedings,
TRIP, LILACS and CINAHL. No RCT
evidence and limited consensus on
what should be included in
management plans.
Sheik A, ten Broek WM, Brown
SGA, Simons FE. “H1antihistamines for the
treatment of anaphylaxis with
and without shock.” Cochrane
Database of Systematic
Reviews 2007; 1.
Systematic
Review – Part B
see part A
Sheikh A et al. "Adrenaline
(epinephrine) for the treatment
of anaphylaxis." Cochrane 4
(2008)
Systematic
Review – Part B
see part A
Page 26
Key outcomes
Standardised action plan templates are likely to reduce confusion caused by
varying instructions and differing plans formulated by medical practitioners or
by parents and carers. All action plans should:
• list allergens that need to be avoided
• provide instructions for action in the setting of an allergic reaction and/or
anaphylaxis
• be dated and signed by a medical practitioner, and
• be easily accessible by carers.
It is essential that patients provided with action plans be regularly reviewed.
Commonly this is done annually, but may vary depending upon
circumstances.
Anaphylaxis Management Plans should have emergency contact details,
advice on recognition of symptoms and treatment of reactions with
epinephrine. Written plans appear to be acceptable to patients and caregivers
and might when issued together with training reduce anxiety levels and
increase knowledge and self-efficacy among parents and school staff
Implications for practice: We found no relevant evidence. We are therefore
unable to make recommendations about H1-antihistamine use in the treatment
of anaphylaxis. Guidelines on the management of anaphylaxis need to be
much more explicit about the basis of their recommendations regarding the
use of H1-antihistamines. Implications for research: there is a case for RCTs
of high methodological rigour to define the true benefit from H1-antihistamines
in anaphylaxis. Specifically, more information is required on patients most
likely to benefit and the most appropriate preparations, route and dose of
administration. Any future trials would need to consider in particular: •
appropriate sample sizes with power to detect expected differences • careful
definition and selection of target patients • appropriate comparator therapy •
appropriate outcome measures including all those listed in this review • careful
elucidation of any adverse effects and the cost-utility of the therapy.
Intramuscular route for adrenaline is preferred.
Some disagreement exists about the recommended dose of adrenaline but
almost all of the literature agrees on 0.01 mg/kg in infants and children.
Delayed injection of adrenaline in anaphylaxis is reported to be associated
with mortality
Given that current evidence supports the relative safety of intramuscular
adrenaline, and early administration is believed to be associated with an
improved survival, any patient with a serious allergic reaction that is rapid in
onset should be a candidate for adrenaline by auto-injector.
Adrenaline has been associated with the induction of fatal cardiac arrhythmias
and myocardial infarction.
Level
4
4
4
4
Appendix 3: Evidence Table: Guidelines
Table 5: Evidence table: guidelines
Bibliographic Reference
Quality Assessment
RCPCH decision: Practice statement
A literature search of Medline, Scopus,
Cochrane, Embase, GoogleScholar was
conducted, search terms were [anaphylaxis OR
anaphylactic] AND [treatment OR management].
Search dates were 16/10/2006 and final search
07/01/2008 The guideline has not been sent for
external review but was available for comment on
the website for 6 weeks; lay people also
commented.
C*= consensus
Resuscitation Council (UK). The
emergency medical treatment of
anaphylactic reactions. Guidelines
for healthcare providers. 1-50.
2008. London, Resuscitation Council
(UK). [54]
Page 27
There are no key recommendations listed.
There are no grades for the recommendations in
the full guideline.
Grades are noted (according to the RCP
guideline development document) in the short
guideline.
The guideline is well supported with a short
guideline, an algorithm, posters, a slide set and
podcasts on the CKS. An update is planned for
2013, no audit is noted.
Conflict of interest was noted
Summary of Key Outcomes
The diagnosis of anaphylaxis is not always obvious. Clinicians must: use the
systematic approach to assess and treat the patient, treat life-threatening problems as
they are found and monitor the patient (minimum of pulse oximetry, non-invasive blood
pressure and a 3-lead electrocardiogram ASAP)
Patients having an anaphylactic reaction should expect the following as a minimum:
recognition that they are seriously unwell, an early call for help, initial assessment and
treatment based on ABCDE approach, adrenaline therapy, if indicated and
investigation and follow up by an allergy specialist.
Adrenaline is the most important drug for the treatment of anaphylaxis and should be
given to all anaphylaxis patients via the intramuscular (IM) route into the anterolateral
aspect of the middle third of the thigh, using a needle long enough to ensure it is
injected into muscle, monitor the patient to assess response to adrenaline, repeat the
IM adrenaline dose at 5-minute intervals if there is no improvement in the patient’s
condition. Intravenous (iv) adrenaline must only be given by clinicians experienced in
its use. The use of subcutaneous or inhaled adrenaline is not recommended.
All patients should be placed in a comfortable position: patients with airway/breathing
problems may prefer to sit up, lying flat (leg elevation) is helpful for patients with
hypotension, do not make patients sit/stand up if they feel faint as this can cause
cardiac arrest and place unconscious breathing patients in the recovery position.
All patients with anaphylaxis should receive supportive care in addition to definitive
treatment with adrenaline. This includes oxygen, fluids, antihistamines, corticosteroids
and other medications.
If the trigger for the patient’s anaphylactic reaction is identified, it should be removed if
possible. Do not delay treatment if removing the trigger is not feasible. After foodinduced anaphylaxis, attempts to make the patient vomit are not recommended.
If cardiorespiratory arrest occurs following an anaphylactic reaction start
cardiopulmonary resuscitation immediately and call the cardiac arrest team, commence
advanced life support (ALS) as soon as equipment is available, use the iv doses of
adrenaline recommended in the ALS guidelines.
Patients with suspected anaphylaxis should be observed in hospital for at least six
hours and reviewed by a senior clinician. Patients may need careful observation for up
to 24 hours.
Mast cell tryptase should be measured to confirm the diagnosis of anaphylaxis. Ideally,
three time samples should be taken with the minimum requirement of one sample
taken one to two hours after the start of the symptoms. Mast cell tryptase is not useful
in the initial recognition and treatment of anaphylaxis and should not delay
resuscitation of the patient.
Before discharge from hospital, all patients must be reviewed by a senior clinician,
given clear instructions to return to hospital if symptoms return, considered for
treatment with antihistamines and oral steroids for three days to decrease the chance
of a further reaction, considered for an adrenaline auto-injector or given a replacement
Grade
C*
C*
C*
C*
C*
C*
C*
C*
C*
C*
Bibliographic Reference
Mirakian, R. et al. "BSACI guidelines
for the management of drug allergy."
Clinical & Experimental Allergy 39.1
(2009): 43-61. [57]
Quality Assessment
RCPCH decision: Practice statement GDG
includes individuals from relevant professional
groups, including a paediatrician. There is no
patient representative and no patient views were
sought.
There was a systematic search in PubMed and
Cochrane (Jan 2005 and Jan 2007) with the
terms drug, allergy, and all drugs listed in each
section. Other than language criteria there were
no formal inclusion or exclusion criteria. Hand
searches were done via a collection of papers
from the expert team, references cited in articles
found by the systematic search and references of
relevance cited by MHRA’s publication called
‘Drug Safety Update’
The 13 recommendations are graded, there are
no key recommendations. They compiled
evidence tables and used SIGN Grades of
Recommendation from the evidence levels
assigned. There are no evidence sources
attached the recommendations.
All BSACI members reviewed the guideline
before publication. There was no external
review.
Page 28
Summary of Key Outcomes
and given a plan for follow up, including contact with their general practitioner.
All patients presenting with anaphylaxis should be referred to a specialist allergy clinic
to identify the cause of the reaction, reduce the risk of future anaphylactic reactions
and prepare the patient to manage future episodes themselves.
All patients/family/carers should be given information on the trigger allergen, avoidance
advice, how to recognise the early symptoms of anaphylaxis, how to use their
adrenaline auto-injector (if provided), the importance of seeking urgent medical
assistance when experiencing anaphylaxis and after using an adrenaline auto-injector.
A detailed history is required for an accurate diagnosis of a drug-induced reaction and
should include details of drug formulation, dose, an assessment of the time course and
clinical pattern of the reaction. This will inform the likely immunological mechanism and
direct investigation and management (grade of recommendation =A).
Skin prick test (SPT) and intradermal test provide evidence of IgE-mediated
sensitization and patch tests or delayed reading of an intradermal test provide evidence
for a delayed or T cell-mediated process to a specific drug. However, all skin test
results must always be interpreted within the appropriate clinical context (grade of
recommendation = B).
Skin testing for immediate hypersensitivity is not indicated for type III serum sickness
reactions or for T cell-mediated reactions including severe cutaneous reactions such as
Stevens–Johnson syndrome (SJS),toxic epidermal necrolysis (TEN) and drug
reaction/rash with eosinophilia and systemic symptoms(DRESS) (grade of
recommendation = B).
Drug challenge should only be considered after other investigations have been
exhausted and the diagnosis remains in doubt. The primary aim of provocation testing
should be to exclude drug sensitivity/intolerance but it can also be used to confirm
diagnosis or to demonstrate tolerance to an alternative drug (grade of recommendation
= B).
If there are no suitable alternatives, drug desensitisation may be possible for one
course of treatment particularly for antibiotics, aspirin, taxenes and platinum-based
cancer chemotherapeutic agents (grade of recommendation = B).
Prevention of future reactions is an essential part of patient management. The patient
should be provided with written information about which drugs to avoid, the drugs
highlighted in hospital notes and the GP informed (grade of recommendation = B).
Engraved allergy-bracelets are useful when there is a risk of intravenous drug
administration in an emergency ,e.g. muscle relaxants, opiates or penicillin or when
drugs, e.g. NSAIDs are readily available without prescription (grade of recommendation
= B).
When investigating reactions during general anaesthesia it is particularly important to
review the anaesthetic chart, medical notes, drug and nursing charts(grade of
recommendation = C).
If the reaction is not IgE-mediated, a negative skin test result does not exclude the drug
as the cause of the reaction and further investigation should be considered(grade of
recommendation = C).
Skin tests should not be used to screen for drug allergy in the absence of a clinical
Grade
C*
C*
A
B
B
B
B
B
B
C
C
C
Bibliographic Reference
Muraro, A. et al. The management of
anaphylaxis in childhood: position
paper of the European academy of
allergology and clinical immunology.
Allergy 62(8) (2007): 857-71. [60]
Sicherer SH, Simons FE. Selfinjectable epinephrine for first-aid
management of anaphylaxis.
Pediatrics 2007; 119(3):638-646.
[64]
Kemp AS, Hu W. New action plans
for the management of anaphylaxis.
Australian Family Physician 2009;
38(1/2):31.[42]
Quality Assessment
RCPCH decision: Practice statement
The guideline aims to provide practical guidelines
for managing anaphylaxis in childhood based on
the limited evidence available. The guideline
does not provide specific clinical questions but it
is clear from the sub headings what the questions
are.
RCPCH decision: No clear methodology, not a
clear guideline
Summary of Key Outcomes
history compatible with IgE mediated drug allergy (grade of recommendation = C)
Skin testing for delayed-type hypersensitivity with patch tests can be helpful in T cellmediated hypersensitivities such as DRESS syndrome and SJS/TEN.(grade of
recommendation = C).
Serial blood samples for serum tryptase should betaken at the time of suspected
anaphylaxis, at 2 and24 h or later (baseline sample) after onset of anaphylaxis (grade
of recommendation = C).
It is not usually advisable to carry out provocation testing if the reaction has resulted in
a life-threatening reaction. Drug provocation should be carried out by personnel
experienced in drug challenges with adequate resuscitation facilities readily available
(grade of recommendation = C).
Health Care Professionals should report ADRs via the Yellow Card Scheme run by the
Medicines and Healthcare products Regulatory Agency (MHRA) and the Commission
on Human Medicines. (NO GRADE)
Skin tests may be falsely negative even if the reaction is IgE-mediated because of
limitations in the availability of the relevant skin test reagents. (NO GRADE)
Skin tests are particularly difficult to interpret for drugs known to be direct histamine
releasers, e.g. opiates and some neuromuscular blocking agents(NMBA) or if the drug
has been tested at a concentration causing local skin irritation (NO GRADE)
Adrenaline is the cornerstone of therapy both in the hospital and in the community (C )
Each child with a history of a previous allergic reaction to a food or other allergen
should have a risk assessment to identify whether they are at high risk of anaphylaxis
(C)
Previous anaphylactic reactions are indicators of higher risk of severe reaction (B).
Previous anaphylactic reactions and co-existent persistent asthma (D) are indicators of
higher risk of severe reaction.
Other risk factors to consider are a reaction to small amounts of allergen including
airborne allergen and cutaneous contact, previous mild reaction to peanut or tree nut, a
long distance from emergency medical care and being a teenager (D).
Prescription of self-injectable adrenaline is mandatory for high-risk subjects (B).
An individualized management plan and education of all the child's care givers are
essential in the prevention of recurrences (C).
NA
RCPCH decision: Not a guideline
* These recommendations are not synthesised with the SIGN methodology but have used the RCP Concise Guidance to Good Practice
Page 29
Grade
C
C
C
D
D
D
C
C
B
D
D
B
C
Page 30