Presented by New York State Council of Health

Presented by New York State Council of
Health-system Pharmacists’
Certificate Program for Pharmacists,
Infectious Disease Society of NY, and
Montefiore Medical Center
Antimicrobial Stewardship Program
June 17-18, 2011
St. John Fisher College, Rochester, NY
Antimicrobial Stewardship Certificate Program developed by the New York State Council of
Health-system Pharmacists, is supported in part by independent educational grants from
Greater NY Hospital Association Services.
2011 New York State Council of Health-system Pharmacists 1
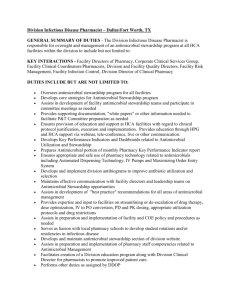
Course Directors/Assistants:
Acknowledgements
Course Faculty:
Brian Currie, MD, MPH Elizabeth Dodds Ashley, PharmD, MHS, BCPS
Director, Antimicrobial Stewardship Program
Professor of Clinical Medicine, Department of
Medicine, (Infectious Diseases), Professor of Clinical
Epidemiology & Population Health, Assistant Dean for Clinical Research, Albert Einstein College of
Medicine, Vice President and Medical Director for
Research, Montefiore Medical Center, Bronx, NY
Co-Director of the Antimicrobial Stewardship Program at University of Rochester Medical Center
Rochester, NY
Debra B. Feinberg, RPh, JD
Co-Director, Antimicrobial Stewardship Program
BS Pharmacy, JD, Executive Director, New York State
Belinda Ostrowsky, MD, MPH
Assistant Professor Department of Medicine
(Infectious Diseases), Albert Einstein College of
Council of Health-system Pharmacists, NY
Elizabeth Dodds Ashley, PharmD, MHS, BCPS
Associate Director of Clinical Pharmacy Services &
Co-Director of the Antimicrobial Stewardship Program at University of Rochester Medical Center
Rochester, NY
Medicine, Director Antimicrobial Stewardship
Program, Montefiore Medical Center, Bronx, NY
Thomas Lodise, PharmD
Associate Professor, Dept. of Pharmacy Practice
Albany College of Pharmacy, Albany, NY
Ben Lomaestro, BS, PharmD
Senior Clinical Pharmacy Specialist
Albany Medical Center Hospital, Albany, NY
Jeffrey Kennicutt, BS, PharmD
Clinical Pharmacist Specialist Infectious Disease
Co-Chairman Antimicrobial and
Infection Management Committee
St. Peters Hospital, Albany, NY
John Papadopoulos, BS, PharmD, FCCM, BCNSP
Associate Professor of Pharmacy Practice
Arnold & Marie Schwartz College of Pharmacy Critical
Care Pharmacist, NYU Medical Center, NY
The opinions or assertions expressed in this program are the private views of the writer(s) and advisors.
Every attempt has been made to ensure the accuracy of the information contained herein at the time of the writing. No part of this book may be reproduced, stored in a retrieval system or transmitted in any form or by any means- electronically, mechanically, photocopying, recording or otherwise- without permission from the publisher.
Copyright © 2010, New York State Council of Health-system Pharmacists. Printed in the United States of
America, New York State Council of Health-system Pharmacists, 2 Pine West Plaza, Washington Avenue
Extension, Albany, NY 12205.
2011 New York State Council of Health-system Pharmacists 2
BIOGRAPHIES:
Brian Currie, M.D., MPH
Director of Antimicrobial Stewardship Program
EDUCATION:
Dr. Currie started at the State University of New York at Buffalo, earning both a Bachelors of Biology and a
Masters of Biology and Mathematical Statistics. In 1984, he graduated with a Master of Public Health in
Epidemiology from Columbia University and then finished his education with a Doctor of Medicine at Albert
Einstein College of Medicine in 1988. He continues at the Albert Einstein College of Medicine teaching
Epidemiology and Population Health to the students as a Professor of Medicine. Dr. Currie is also the Assistant
Dean for Clinical Research at the college.
PROFESSIONAL POSITION:
Dr. Currie is the Vice President/Medical Director for Research, along with Attending Physician of
Medicine/Infectious Diseases and Director of Infection Control at the Montefiore Medical Center. He is also the
Director of Infection Control at Weiler Hospital. Dr. Currie has been principal investigator and co-principal investigator for several research projects involved with improving patient care quality. One of his older research projects, completed in 2001, worked to 1) establish a regional electronic surveillance system for monitoring multiple antibiotic resistance patterns among nosocomial pathogens, and 2) establish a unique pooled research data base to investigate the relationship of antibiotic use and antibiotic resistance factors.
With all of his experience in the Infectious Disease field, there could not be a better fit Director of the
Antimicrobial Stewardship Program.
PROFESSIONAL ACTIVITIES:
Dr. Currie is a member of several societies at this time, including, The Society for Healthcare Epidemiology of
America (Fellow), the American Society of Microbiology(Member),the Infectious Diseases Society of America
(Fellow), the New York State Infectious Disease Society (President-elect 2008, President 2009), and the New
York Academy of Medicine (Fellow). Dr. Currie has had many peer-reviewed articles published in many different journals such as the New England Journal of Medicine, Journal of Clinical Microbiology, and Clinical
Infectious Disease.
Dr. Brian Currie has disclosed that he is a member of the BioK Advisory Board (probiotics) and the
Merck Vaccine Advisory Board.
Debra B. Feinberg, RPh, JD
Co-Director of Antimicrobial Stewardship Program
EDUCATION:
Debra B. Feinberg is a New York Registered Pharmacist who received her Bachelor of Science degree in
Pharmacy from Albany College of Pharmacy and her Juris Doctor from Albany Law School.
PROFESSIONAL POSITION:
Debra is the Executive Director of the New York State Council of Health-system Pharmacists, an association for hospital and health-system pharmacists. She is also an Assistant Adjunct Professor at Albany College of
Pharmacy teaching Jurisprudence.
PROFESSIONAL ACTIVITIES:
Debra is a member of the American Society of Health System Pharmacists, New York State Council of Healthsystem Pharmacists, and American Society of Association Executives.
Debra Feinberg has disclosed that she has had no financial arrangement or affiliation with commercial interests during the 12 months directly preceding this CME activity.
2011 New York State Council of Health-system Pharmacists 3
Elizabeth S. Dodds Ashley, PharmD, MHS, BCPS
Co-Director & Course Faculty
EDUCATION:
Dr. Dodds Ashley first received a Doctor of Pharmacy Summa Cum Laude in 1998 from Bouvé College of
Pharmacy and Health Sciences Northeastern University in Boston, Massachusetts. The following two years she did a Pharmacy Practice Residency at Duke University Health System in Durham, North Carolina and a
Specialty Residency in Adult Internal Medicine/Infectious Disease/Academia at Campbell University also in
North Carolina. Most recently, in 2006, Dr. Dodds Ashley earned her Masters of Health Science in Clinical
Research from Duke University School of Medicine, where she continues there as an Adjunct Assistant
Professor in the Division of Infectious Diseases and International Health. She is also Board Certified
Pharmacotherapy Specialist since 1999.
PROFESSIONAL POSITION:
Currently, Dr. Dodds Ashley is the Associate Director of Clinical Pharmacy Services and Co-Director of the
Antimicrobial Stewardship Program at the University of Rochester Medical Center. At the hospital she is a part of the Research Subjects Review Board and the Antibiotic Subcommittee of the Strong Health Therapeutics
Committee.
Dr. Dodds Ashley has disclosed that she has been a consultant for Pfizer. She is on the Speaker’s
Bureau for Merck.
Thomas P. Lodise, PharmD
Course Faculty
EDUCATION:
Dr. Lodise, a 1999 summa cum laude doctor of pharmacy graduate of Temple University School of Pharmacy, joined the faculty at Albany College of Pharmacy in August 2002. Prior to Albany College of Pharmacy, he completed the APhA-ASHP–accredited Pharmacy Practice Residency at Thomas Jefferson University Hospital,
Philadelphia, Pennsylvania in 2000 and the Infectious Diseases Pharmacotherapy and Outcomes Fellowship at
Wayne State University, Detroit, Michigan in 2002.
PROFESSIONAL POSITION:
Dr. Lodise coordinates the antibiotic monitoring service at the Stratton VA Medical Center. He is a member of the Antibiotic Subcommittee at the Albany Medical Center Hospital and is a visiting professor at Ordway
Research Institute. He is also enrolled in the doctor of philosophy program in epidemiology at the State
University of New York School of Public Health, Albany, New York. Integrating his dual interests in research and patient care, his current research focuses on the epidemiology and outcomes of bacterial infections at the
Albany Medical Center and the Stratton VA Medical Center, Albany, New York. His work explores the antibiotic exposure-response relationship among patients. His specific objectives are 3-fold: develop patient care strategies and antibiotic regimens that improve outcomes, reduce the likelihood of toxicity, and minimize the emergence of antibiotic resistance.
PROFESSIONAL ACITIVIES:
Dr. Lodise is a member of the Society of Infectious Diseases Pharmacists, the American Association of Colleges of Pharmacy, and American College of Clinical Pharmacist (ACCP), and president of the New York ACCP chapter. He is a reviewer for numerous medical and pharmacy journals and has published over 30 peerreviewed articles in reputable scientific journals, including Clinical Infectious Diseases, Antimicrobial Agents
and Chemotherapy, Chest, and Journal of Antimicrobial Chemotherapy. He has also secured over $900,000 in grant funding.
Dr. Thomas Lodise has disclosed that he has received grant/research from Cubist, Pfizer, Astellas and Merck. He is on the Speakers Bureau for Cubist, Pfizer and Astellas, and is a consultant for
Cubist, Pfizer, Astellas and Forest. He intends to discuss the unlabeled or investigational use of extended infusion of beta-lactam antibiotics.
2011 New York State Council of Health-system Pharmacists 4
Ben M Lomaestro, Pharm.D., B.S.
Course Faculty
EDUCATION:
Dr. Lomaestro earned his Bachelor of Science and Pharmacy Doctorate degrees from the Albany College of
Pharmacy and is now an Adjunct Professor at the school.
PROFESSIONAL POSITION:
Dr. Lomaestro is a senior clinical pharmacist specializing in Infectious Diseases at the Albany Medical Center
Hospital and is currently involved in pharmacodynamic and pharmacokinetic research here. His appointments include secretary of the Antibiotic and Pharmacy and Theapeutics Committees and membership of the
Epidemiology and Resistance Committees as well as founding member of the hospital’s Antimicrobial
Stewardship team. Dr. Lomaestro is also a consultant for several pharmaceutical companies.
PROFESSIONAL ACTIVITIES:
Dr. Lomaestro serves as a reviewer for Annals of Pharmacotherapy and Pharmacotherapy and as an editor for the New York Health System Pharmacists and the Annals of Pharmacotherapy. He has published extensively in the field of antimicrobial therapy and presented numerous abstracts at state, national and international meetings. He is a member of the American Society of Medicine and Infectious Diseases Society of America.
He is a Past-President of the New York State Chapter of the American College of Clinical Pharmacy (ACCP) and of the Northeastern New York State Chapter of the American Society of Hospital Pharmacists (ASHP). In 2001 he was honored as New York State Council of Health-system Pharmacists Pfizer Health-system pharmacist of the year. In 2010 received the Society of Infectious Diseases Pharmacists award for Outstanding Clinical
Practice in Infectious Disease Pharmacotherapy Award.
Dr. Ben Lomaestro has disclosed that he is on the Speakers Bureau for Astellas and Pfizer, and a
Consultant for Ortho McNeil and Pfizer.
Jeffrey D. Kennicutt, B.S., Pharm. D
Course Faculty
EDUCATION:
Jeffrey received his Doctor of Pharmacy, Cum Laude and B.S. in Pharmacy from Albany College of Pharmacy in
Albany, N.Y. and serves as Adjunct Faculty there today. Additionally he provides classroom instruction on management of the infected patient for the Sage Colleges, Graduate School of Nursing.
PROFESSIONAL POSITION:
Dr. Kennicutt is the Clinical Pharmacy Specialist in Infectious Disease at St. Peter’s Health Care Services
Albany, NY. Dr. Kennicutt is Co-Chairman St Peter’s Hospital Antimicrobial and Infection Management
Committee. In collaboration with hospital administration, chief of medicine, infection control, microbiology, epidemiology and infectious disease specialists, Jeffrey has expanded the clinical pharmacy antimicrobial surveillance plan into current multidisciplinary Antimicrobial Stewardship Program based on ID rounding team and prospective review. His experience and leadership in ongoing hospital improvement initiatives such as antimicrobials for surgical procedure prophylaxis, including SCIP and HOP, have been important to the success of the surgical services at St. Peter’s Health Care Services. He also has career-long publishing and clinical practice experience in geriatrics and long-term care facilities with St. Peter’s and other health systems. Dr.
Kennicutt’s comprehensive geriatric pharmacotherapy program includes ID items such as antibiogram development, influenza outbreak management, clinical guidelines and critical pathways involving the use of antimicrobials in the institutionalized geriatric patient.
PROFESSIONAL ACTIVITIES:
Dr. Kennicutt enjoys involvement in several state and national professional organizations including New York
State Council of Health-system Pharmacists (NYSCHP). With NYSCHP he has served as member and
Chairman Continuing Competency Committee directly responsible for educational program development for the membership.
Dr. Kennicutt has disclosed that he has had no financial arrangement or affiliation with commercial interests during the 12 months directly preceding this CME activity.
Belinda Ostrowsky, M.D., M.P.H.
2011 New York State Council of Health-system Pharmacists 5
Course Faculty
EDUCATION:
Dr. Ostrowsky attended the Sophie Davis Biomedical Program at City University of N.Y and received her MD from SUNY Stony Brook. She did an Internal Medicine Residency at the Mayo Clinic in Rochester, MN and then an Infectious Diseases Fellowship at the Beth Israel Deaconess Medical Center in Boston, MA. During her fellowship she obtained an MPH from Harvard School of Public Health.
PROFESSIONAL POSITION:
Dr. Ostrowsky brings with her a background of expertise in healthcare epidemiology, experience in public health and is the director of the burgeoning Montefiore Medical Center (MMC)/Albert Einstein College of
Medicine (AECOM) Antimicrobial Stewardship Program. Prior to joining the facility at MMC/AECOM in 2008, Dr.
Ostrowsky was the Director of Communicable Diseases and STD/TB at the Westchester County Department of
Health. And before this, Dr. Ostrowsky was an Epidemiology Intelligence Service Officer at the CDC working on issues relating to healthcare acquired infections, resistance and related issues. As an EIS officer Dr.
Ostrowsky led 2-years of a multi-state infection control initiative to control the resistant pathogen vancomycin resistant enterococcus, which has been held as a model for regional cooperatives and was subject of a New
England Journal of Medicine Article (she is the first author).
PROFESSIONAL ACTIVITIES:
Dr. Ostrowsky and MMC/AECOM multidisciplinary antimicrobial stewardship team have been instrumental in revamping the approval system for restricted antibiotics, addressing hospitals performance on CMS and other quality measures, MMC facilities nimble and large scale response to H1N1 influenza and many other exciting activities. In addition, Dr. Ostrowsky is involved in healthcare epidemiology and stewardship on the regional
(serving on the GNYHA steering committee on stewardship) and national level [a practice counselor to the
Board of Director’s of Society of Healthcare Epidemiology of America (SHEA) and on national committees in past.
Dr. Belinda Ostrowsky has disclosed that she has had no financial arrangement or affiliation with commercial interests during the 12 months directly preceding this CME activity.
John Papadopoulos, Pharm.D
Course Faculty
EDUCATION:
Dr. Papadopoulos received his Bachelor of Science degree in Pharmacy from Saint John’s University in 1993.
He pursued his Doctor of Pharmacy degree at the Arnold & Marie Schwartz College of Pharmacy and Health
Sciences where upon completion of the degree requirements received the first Pharm.D. degree from the college in June of 1996. A passion for critical care pharmacotherapy propelled Dr. Papadopoulos to purse and complete a specialized residency in critical care at the Medical University of South Carolina.
PROFESSIONAL POSITION:
Currently, he is an Associate Professor of Pharmacy Practice at the Arnold & Marie Schwartz College of
Pharmacy and Health Sciences. Dr. Papadopoulos is also the Director of Pharmacotherapy – Division of
Pharmacotherapy, a Critical Care Pharmacist, the Residency Program Director, and a Clinical Assistant
Professor of Medicine at the New York University Langone Medical Center. Dr. Papadopoulos is a Fellow of
Critical Care Medicine in the American College of Critical Care Medicine and is Board Certified in Nutrition
Support Pharmacy.
PROFESSIONAL ACTIVITIES:
His areas of interest include critical care pharmacotherapy, cardiology, infectious diseases, thromboembolic disorders, nutrition, neurology, and pulmonary disorders. Dr. Papadopoulos has published a handbook and several articles in the area of critical care. His handbook is entitled “Pocket Guide to Critical Care
Pharmacotherapy”. Some of his published work includes “The Critical Care Pharmacist: An Essential Intensive
Care Practitioner”, “Pharmacological Management of Acute Arterial Atherothrombotic and Cardioembolic
Cerebrovascular Accidents”, “Utilization of a Glucagon Infusion in the Management of a Massive Nifedipine
Overdose”, and “Hematogenous Candidiasis in Critically-Ill Adult Patients- Epidemiology, Risk Factors, and
Management”.
Dr. Papadopoulos has disclosed that he is a consultant for Pfizer.
2011 New York State Council of Health-system Pharmacists 6
Statement of Need:
Antimicrobial Stewardship utilizes a team approach of physicians and pharmacists working together to manage antibiotic use in an institution. The goal of antimicrobial stewardship is “The optimal selection, dosage, and duration of antimicrobial treatment that results in the best clinical outcome for the treatment or prevention of infection, with minimal toxicity to the patient and minimal impact on subsequent resistance” (Gerding DN. The
search for good antimicrobial stewardship. Joint Commission J Qual Improv 2001;27:403-4). The goal of the
Antimicrobial Stewardship Certificate Program is to provide the knowledge base and a mentoring program to work with clinical pharmacists and infectious disease physicians who will implement an antimicrobial stewardship program at their institutions as an essential component of patient safety.
Conflict of Interest Statement:
The “Conflict of Interest Disclosure Policy” of Albert Einstein College of Medicine requires that faculty participating in any CME activity disclose to the audience any relationship(s) with a pharmaceutical or equipment company. Any presenter whose disclosed relationships prove to create a conflict of interest with regard to their contribution to the activity, or who refuses to provide all their conflict of interest information, will not be permitted to present.
The Albert Einstein College of Medicine also requires that faculty participating in any CME activity disclose to the audience when discussing any unlabeled or investigational use of any commercial product, or device, not yet approved for us in the US. Albert Einstein College of Medicine CCME staff, the staff of NYSCHP, and IDSNY have no conflicts of interest with commercial interests related directly or indirectly to this educational activity.
Special Needs:
If any participant of the “Antimicrobial Stewardship Program” given by Albert Einstein College of Medicine is in need of accommodations, please do not hesitate to submit written requests to Debra Feinberg at dfeinberg@nyschp.org or 518-456-8819, at least 2 weeks prior to the activity.
Certificate Program Purpose and Instructions:
The purpose of this educational program is to:
1.
Provide a comprehensive understanding of antimicrobial resistance and management of
2.
antimicrobials in the institution.
Provide physicians and pharmacists with the knowledge, skills and resources necessary to establish and promote successful antimicrobial stewardship in their institutions.
Provide a knowledge base to physicians and pharmacists for implementation of an antimicrobial 3.
4.
stewardship program.
Establish a physician-pharmacist network for continued mentoring in antimicrobial stewardship.
The Antimicrobial Stewardship Certificate Program is conducted in two parts: the self study and the live training workshop. To earn a Certificate of Achievement for the entire certificate training program, participants must successfully meet the following requirements:
1.
Read the Self Study Materials in their entirety and successfully complete the Self Study Assessment.
A score of 70% or better is required.
2.
3.
Submission of your antibiogram from your institution.
A Certificate of Achievement is awarded to participants who successfully complete all program requirements.
Attend Conference: On Site Training and successfully complete the open book Final Exam. A score of 70% or better is required.
Activity type: Practice Based.
Target Audience: This program has been designed for pharmacists, specialists, and physicians who are involved with antimicrobial culturing, diagnosing, and treatment, and who are interested in, improving their skills in these fields and improving patient care.
2011 New York State Council of Health-system Pharmacists 7
Accreditation:
Credit Designation:
Physicians:
This activity has been planned and implemented in accordance with the ‘Essential Areas and
Policies’ of the Accreditation Council for Continuing Medical Education (ACCME) through joint sponsorship of
Albert Einstein College of Medicine, NYSCHP and IDSNY. Albert Einstein College of Medicine is accredited by the ACCME to provide continuing medical education for physicians.
Home Study: Albert Einstein College of Medicine designates this educational activity for a maximum of 5 AMA
PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Conference: Albert Einstein College of Medicine designates this educational activity for a maximum of 10 AMA
PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Pharmacists:
Antimicrobial Stewardship Certificate Program was developed by the New York State Council of Health-system Pharmacists, Infectious Disease Society of NY and Montefiore Medical Center and supported in part by independent education grants from Greater NY Hospital Association Services, Inc.
The New York
State Council of Health-system Pharmacists is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education.
Credit Designation:
Self study learning portion of the Antimicrobial Stewardship Program is approved for 5 hours (0.5 CEUs) of continuing education credit. ACPE Universal Program Number is 0134-0000-11-0310H01-P (Initial release date: 3/18/2011; expiration 3/18/2014)
Live training seminar is approved for 11.5 hours (1.15 CEUs) of continuing education credit. ACPE Universal
Program Number is 0134-000-11-031-L01-P (Initial release date: 3/18/2011; expiration date 3/18/2014).
*Statement of Credit and Certificate of Achievement will be mailed to participants 6 weeks following receipt of completed program materials.
Self Study Description and Learning Objectives
The self study component is meant to ensure that all participants have an understanding of antimicrobial resistance and the need for antimicrobial stewardship in our institutions.
A.
Define the components of an antimicrobial stewardship program (ASP) in the acute care setting.
B.
C.
Identify factors contributing to increasing antimicrobial resistance.
Develop and implement evidence-based treatment guidelines utilizing local microbiology data.
D.
Review antimicrobial order forms and determine their use in your institution.
E.
Discuss the preparation of antibiograms and potential pitfalls in their preparation.
F.
G.
Evaluate mechanisms for managing nosocomial infections and prevention/reduction of resistance.
Strategize the process for setting up an ASP, insuring hospital administration commitment as a quality assurance and patient safety initiative.
H.
Describe mechanisms for monitoring and reporting outcomes of an ASP.
I.
Identify barriers in your own facility to the implementation of an ASP.
J.
K.
Debate the pros and cons of antibiotic cycling.
Review and understand the advantages and disadvantages to the 2 core strategies: prospective audit with intervention and feedback versus formulary restriction and preauthorization.
L.
Determine how education of the health care team will be implemented and incorporated with active
M.
intervention.
List the advantages to shorter antimicrobial treatment durations for treating various infections utilizing data from primary literature to support this approach.
2011 New York State Council of Health-system Pharmacists 8
Live Seminar Description and Learning Objectives
Review antimicrobial restriction policies and their use in the ASP.
Develop and implement evidence-based practice guidelines to improve antimicrobial utilization and patient safety.
Discuss and review antimicrobial order forms from participating institutions.
Discuss utilization of antibiograms, including the role of unit-specific antibiograms.
Determine ways to support cost-justification of ASPs.
Develop strategy for obtaining multi-discipline commitment to the ASP.
Review case studies addressing antimicrobial combination therapy.
Assess the use of de-escalation or streamlining of empiric antimicrobials and the desired outcomes.
Compare and contrast the components of dose optimization in ASPs.
Review and evaluate process measures and outcome measures in determining the impact of the ASP on antimicrobial use and resistance data.
Discuss mechanisms to monitor outcomes and utilize antimicrobial data for program improvement.
Discuss tools to insure effective multidisciplinary collaboration in the ASP.
Evaluate the role technology plays in the effectiveness of ASPs.
Review and evaluate the role of the clinical microbiology laboratory in the success and effectiveness of the ASP.
Home Study Materials:
The required readings for the home study are listed below. You are required to read the home study materials, complete the case studies and be prepared to discuss the case studies at the live session and complete the home study examination. The home study examination answers must be faxed to NYSCHP no later than 3-14-11, 518-456-9319. You must obtain a score of 70% or higher on the home study examination to obtain a statement of credit for the home study portion of the Antimicrobial Stewardship Program.
Overview of Antimicrobial Stewardship in 2009; Dellit TH, Owens RC, McGowan JE, et al .
Infectious
Diseases Society of American and the Society for Healthcare Epidemiology of America Guidelines for
Developing an Institutional Program to Enhance Antimicrobial Stewardship: CID 2007;44:159-77
Kamarasamy K, Toleman M, et al. Emergence of a new antibiotic resistance mechanism in India, Pakistan and
the UK: a molecular, biological and epidemiological study Lancet infect Dis 2010, 10:597-602.
MRSA: Reimbursement, Throughput, Guidelines; Ryback M, Lomaestro BM, Rotschafer JC, et al.
Therapeutic Monitoring of Vancomycin in Adult Patients: A Consensus Review of the American Society of
Health-System Pharmacists, the Infectious Diseases Society of America and the Society of Infectious Diseases
Liu C, Rayer, A, et al. Clinical Practice Guidelines by the Infectious Diseases Society of America for the
Treatment of Methicillin-Resistant Staphylococcus Aureus Infection in Adults and Children: CID 2011:52
Bush K, Jacoby G. MDR GNRs: What to Do With Them, Optimal Therapy; Paterson D; Impact of
Antibiotic Resistance in Gram-Negative Bacilli on Empirical And Definitive Antibiotic Therapy; CID
2008;47:;S14-S20; Nicasio A, Kuti J, Nicolau D; The Current State of Multidrug-Resistant Gram-Negative
Bacilli in North America; AM Pharmacotherapy 2008;28(2):235-249.
De-escalation, Short Course Therapy Strategies; Kollef MH, Appropriate Empirical Antibacterial Therapy
for Nosocomial Infections; Drugs2003:63(20):2157-2168
Optimizing Dosing Strategies: PK PD from Bench top; Lodise TP, Lomaestro BM, Drusano GL;
Application of Antimicrobial Pharmacodynamics Concepts into Clinical Practice: Focus on -Lactam Antibiotics;
Pharmacotherapy 2006;26(9):1320-1332
Updated Functional classification of ß-Lactamases: Antimicrobial Agents and Chemotherapy 2010; 960-976
Stewardship Role in HOPS and SCOP; Anderson DJ, Kaye KS, Classen D, et al; Strategies to Prevent
surgical Site Infections in Acute Care Hospitals; Infection and Control and Hospital Epidemiology; 2008;29:1-
11
Antibiograms; Cumulative Antibiogram Development, Summary Checklists for the Collection, Analysis and
Presentation of Cumulative Antimicrobial Test Data; Constructing a Cumulative Antibiogram
CDC Tools and Resources: Get Smart for Healthcare http://cdc.gov/getsmart/healthcare/improveefforts/resources/index.html
2011 New York State Council of Health-system Pharmacists 9
CASE STUDIES
Case #1
The pharmacy director states the hospital is floundering for the last 2 years in Core Measure improvement goals taken from the Surgical Care Improvement Project (SCIP) quality improvement measures. The discussion continues with a display of internal data showing 4 of the 7 procedures the federal government collects publicly transparent data on (hip arthroplasty, knee arthroplasty, vaginal hysterectomy, and colorectal surgery) performed poorly on antimicrobial prophylaxis at your hospital. Further examination of more detailed internal statistics reveal SCIP quality measure #1- Delivery of intravenous antimicrobial prophylaxis within 1 hour before incision and SCIP quality measure 2- Use of an antimicrobial prophylactic agent consistent with published guidelines are both very acceptable across all 7 procedures. However the third SCIP quality measure- Discontinuation of use of the prophylactic antimicrobial agent within 24 hours after surgery shows compliance of 38% to 63% against a hospital goal of 95% for the four procedures mentioned above. Clearly this data analysis points to the procedures with discontinuation of antimicrobial prophylaxis within 24 hours as the problem to focus on.
The pharmacy director asks what you think the pharmacy department can do to support the organization’s desire to improve performance on the third SCIP quality measure- Discontinuation of use of the prophylactic antimicrobial agent within 24 hours after surgery? Please select potentially appropriate step(s) from the proposals listed below.
A) Suggest asking the Quality Assurance and Improvement staff to identify from their data base the names of the surgeons associated with the failures form the last 3 quarters.
B) Suggest reviewing a sample of cases deemed failures for antimicrobial order discontinuation for the four procedures (hip arthroplasty, knee arthroplasty, vaginal hysterectomy, and colorectal surgery).
Look for potential treatment of infection or perhaps clearly written order for continuation of prophylaxis greater than 24 hours.
Suggest a meeting with the Chief of Surgery and the Chief of Medicine to discuss your findings focusing C) on the providers and reasons identified as a trend linking the poor performance for timely discontinuation of antimicrobials for the target procedures.
D) Suggest redesign standardized post-operative order sets insuring the duration of therapy be no more than 24 hours post-op when ordered correctly.
E) All of the above are in potentially appropriate steps.
Case #2
70 year old man with COPD who has failed extubation following an emergent AAA repair. He has been ventilated for the past 10 days. Over the past 48 hours he has required increased ventilator support and is now febrile (38.5).
PMH: HTN X 15 years
COPD X 10 years
SH: 30 pack year smoking history, quit 5 years ago
Pertinent Labs/Data: WBC: 13,000
Scr: 1.2
BUN: 18
Weight: 80 kg
Blood cultures are obtained and a chest x-ray is performed that reveals a left lower lobe infiltrate. A bronchbrush specimen targeted to the site of the infiltrate is obtained. While the team awaits initial results from the microbiology laboratory, the following empiric antibiotic regimen is started:
Piperacillin/tazobactam 4.5g q8h
Vancomycin 1.25g IV q12h
Briefly outline a therapeutic plan (including duration of therapy) for the following 2 scenarios:
1.
Culture results are negative and the patient clinically improves on the prescribed regimen
2.
Culture results reveal 3+ Pseudomonas aeruginosa susceptible to quinolones, aminoglycosides and anti-pseudomonal beta-lactams
2011 New York State Council of Health-system Pharmacists 10
Case study #3
Your hospital pharmacy director recently attended a talk at a national pharmacy meeting on extended infusion beta-lactam therapy. Based on the presentation, he would like to implement extended infusion beta-lactam protocols at your hospital and he tasked you with presenting the idea to the hospital antibiotic subcommittee.
He wants you to discuss the science and rationale for extending the infusion time of beta-lactam antibiotics and review the supporting clinical data. He also believes it is important that you explain “Monte Carlo” simulation to the committee and how “Monte Carlo” can be used to determine optimal dosing of antibiotics.
He also wants you to discuss the factors that need to be considered when selecting the optimal dosing scheme for a beta-lactam antibiotic.
Questions
What is the rationale for extending the infusion time of beta-lactam antibiotics? 1.
2.
What is Monte Carlo simulation and how is it used to determine optimal dosing of antibiotics?
3.
What clinical data are available to support the use of extended infusion beta-lactam therapy?
4.
What factors should be considered when selecting an optimal dosing scheme for a beta-lactam antibiotic?
Case Study #4
J.M. is a 27 year old construction worker who developed a painful abscess on his right forearm and a low grade fever one week ago. Upon seeing his primary care physician three days ago, he was started on amoxicillin/clavulanate 875 mg po twice daily. He now presents to the Emergency Department with a worsening abscess, continuing fever and an elevated white blood cell count.
Question:
1.
A reasonable treatment option would be to a.
Continue the amoxicillin/clavulanate for a few more days b.
Drain the abscess c.
Change to intravenous ampicillin/sulbactam and admit for a few days d.
Drain the abscess and change to an antimicrobial appropriate for MRSA
2011 New York State Council of Health-system Pharmacists 11
ASP Home Study Quiz
Please make one selection and circle your selection on the attached answer sheet for the Home Study
Program. Please fax your answer sheet to NYSCHP no later than 3-14-2011, 518-456-9319.
1.
Vancomycin trough concentrations between 15 – 20 mg/L are recommended for which of the following indication(s)? a.
endocarditis b.
meningitis c.
hospital acquired pneumonia d.
all of the above
2.
Which of the following concentration determinations are most often recommended to monitor vancomycin therapy lasting several days ? a.
Vancomycin “peak” concentration b.
Vancomycin “trough” concentration c.
Vancomycin levels are not required d.
None of the above are true
3.
Your MRSA isolate has a mean inhibitory concentration (MIC) 2.0 mg/L for vancomcyin. The patient has hospital acquired pneumonia. What is the best vancomycin intervention ? a.
Use something else b.
c.
Change to continuous infusion
Change to q6h but keep the same total daily dose d.
Add cefazolin
4.
5.
Which of the following is not an established risk factor for an SSI? a.
Smoking b.
Diabetes mellitus c.
Previous surgical site infection unrelated to current surgery d.
Shaving the surgical site with a razor
The Centers for Medicare and Medicaid Services, Surgical Infection Prevention Collaborative identified 3 performance measures for quality improvement related to antimicrobial prophylaxis.
Identify which statement does NOT represent these measures. a.
Delivery of intravenous antimicrobial prophylaxis within 3 hours before incision. b.
Delivery of the antimicrobial prophylaxis within 1 hour before incision with exceptions for 2 hours for vancomycin and fluoroquinolones. c.
Use of an antimicrobial prophylactic agent consistent with published guidelines d.
Discontinuation of use of the prophylactic antimicrobial agent within 24 hours after surgery
(discontinuation within 48 hours is allowable for cardiothoracic procedures for adult patients).
6.
7.
Negative outcomes associated with SSI include which of the following statements. a.
Each SSI is associated with approximately 7-10 additional postoperative hospital days. b.
Patients with an SSI have a 2-11 times higher risk of death, compared with operative patients without an SSI and 77% of deaths among patients with SSI are directly attributable to SSI. c.
Attributable costs of SSI vary, with ranges from $3,000 to $29,000. d.
None of the above e.
All of the above
Which ONE of the following statements is TRUE regarding Minimum Inhibitory Concentration (MIC-
24)? a.
MIC breakpoints are determined based on clinical outcomes and can be considered accurate predictors of success or failure. b.
The MIC is defined as the lowest antimicrobial concentration which can still kill an organism after c.
d.
24 hours of incubation in a specific growth media.
The determination of MIC does not account for the post-antibiotic effect of antibiotics.
The MIC reflects the rate of bacterial killing.
2011 New York State Council of Health-system Pharmacists 12
8.
9.
Which ONE of the following statements is FALSE? a.
Aminoglycosides exhibit concentration-dependent killing. b.
β-lactams exhibit concentration-independent or time-dependent killing. c.
Fluoroquinolones exhibit concentration-independent killing. d.
For β-lactams, time that the concentration exceeds the MIC of the organism during the dosing interval appears to be the best predictor of bacterial killing and microbiologic response.
For beta-lactams, which ONE of the following is the least effective strategy for increasing T>MIC? a.
Increasing the dose b.
Continuous infusion c.
Increasing the dosing frequency d.
Extending the administration time
10.
Which ONE of the following statements is FALSE? a.
The primary goal of antimicrobial stewardship is to optimize clinical outcomes while minimizing unintended consequences of antimicrobial use, including toxicity, the selection of pathogenic b.
organisms and the emergence of resistance.
Collaboration between the antimicrobial stewardship team and the Center for Disease control is essential. c.
Hospital administrative support for the necessary infrastructure to measure antimicrobial use d.
and to track use is essential.
Prospective audit with intervention and feedback is a core strategy for any antimicrobial stewardship program.
11.
Which of the following are key supplements to the core active antimicrobial stewardship strategies? a.
Education b.
Antimicrobial order forms c.
Dose optimization d.
All of the above
12.
Prospective audit of antimicrobial use with direct interaction and feedback to the prescriber, performed by a clinical pharmacy with infectious disease training can result in reduced inappropriate use of antimicrobials? a.
True b.
False
13.
What is the most effective means of antimicrobial restriction? a.
Formulary limitation b.
c.
Requirement of preauthorization and justification a & b d.
None of the above
14.
Routine use of antimicrobial cycling is an essential component of a stewardship management program? a.
True b.
False
15.
The use of antimicrobial order forms can be an effective component of antimicrobial stewardship and can facilitate implementation of practice guideline? a.
True b.
False
16.
In which of the following contexts does routine use of combination therapy prevent the emergence of resistance? a.
TB b.
HIV c.
a & b d.
None of the above.
2011 New York State Council of Health-system Pharmacists 13
17.
Which antimicrobial activity correlates with the percentage of time that the drug concentration remains greater than the MIC? a.
Fluoroquinolones b.
Aminoglycosides c.
–lactams d.
Vancomycin
18.
Which of the following may occur with a systemic plan for parenteral to oral conversion of antimicrobials? a.
Increase length of patient hospital stay b.
Decrease health care cost c.
a & b d.
None of the above.
19.
What information does the clinical laboratory provide in antimicrobial management? a.
Patient-specific culture and susceptibility b.
Surveillance data of resistant organisms c.
a & b d.
None of the above.
20. Inappropriate initial antimicrobial therapy has been linked to which of the following negative outcomes: a.
Antimicrobial resistance b.
Increased mortality c.
Increased cost d. B and C
e.
All of the above
21 Appropriately applied localized susceptibility data can be used to: a.
Prepare prophylaxis protocols for ventilator-associated pneumonia b.
Select empiric antimicrobial regimens with a high likelihood of treating the majority of infections encountered c.
Determine the appropriate duration of therapy for nosocomial pneumonia in patients with documented infection d.
Predict an antibiotic drug budget for your institution e.
All of the above
22. Antibiotic de-escalation is one approach to limit the emergence of resistance. Which of the following are additional strategies that can be employed: a. Develop localized antibiotic use guidelines b. Develop guidelines to assure appropriate cultures are ordered to aid in diagnosis c. Provide education to key prescribers regarding appropriate antibiotic use d.
Use antibacterial cycling e.
All of the above
23.
Which of the following antimicrobial classes has the best clinical outcomes in the management of infections due to extended-spectrum beta-lactamase producing gram-negative bacteria? a.
aminoglycosides b.
Fluoroquinolones c.
d.
Carbapenems
Macrolides e.
Lincomycins
2011 New York State Council of Health-system Pharmacists 14
24.
25.
26.
27.
28.
29.
30.
Resistance mechanisms that Pseudomonas aeruginosa possess against carbapenems include which of the following?
I.
II.
III.
Porin mutations
Expression of efflux pumps
Production of metallo -lactamases a.
I only b.
III only c.
d.
I and II only
II and III only e.
I, II, and III
Which of the following statements is true? a.
AmpC beta-lactamases fall under the Bush-Jacoby-Meideros group 2f beta-lactamases b.
The drug-of choice for carbapenemase-producing Klebsiella (KPC) infections is cefepime c.
Extending the infusion duration from 30-minutes to 3-hours may increase the probability of bactericidal target attainment for some gram-negative pathogens
Polymixin B has greater bactericidal activity against Klebsiella spp. than polymixin E d.
e.
All of the above statements are true
Programmatic primary antimicrobial stewardship strategies considered appropriate by the
ISDA/SHEA guidelines include the following: a.
Restricting pharmaceutical representative access to hospitals b.
Prospective audit with education and feedback c.
Antimicrobial restrictions d.
b & c only
Recommended supplemental strategies that support a primary antimicrobial stewardship strategy include the following: a.
b.
Intravenous to oral antimicrobial therapy
De-escalation/streamlining antimicrobial therapy c.
Rotating antimicrobial therapy d.
a & b only
Computerized antimicrobial decision support programs are designed to supplant human decision. a.
True b.
False
The IDSA/SHEA guidelines target which of the following facilities? a.
Long term care b.
Acute care c.
Prisons d.
Adult homes
The Infectious Diseases Society of America-United States Public Health Service grading system for ranking recommendations in clinical guidelines utilizes which letter as “Good evidence to support a recommendation for use”? a.
A b.
B c.
C d.
D
2011 New York State Council of Health-system Pharmacists 15
ASP Self Study Examination Answer Sheet June 2011
Complete both sections of this Examination Answer Sheet and fax to NYSCHP at 518-456-9319 no later than
6-13-2011.
Please print clearly or type: Statements of Continuing Pharmacy Education Credits and Certificate of
Achievements will be mailed to the address indicated below:
Name
____________________________________ __________________ ________ ___________
Street Address City State Zip Code
________________ _________________ _________________________________________
Phone Fax Email
Employer
_______________________________________________________________________________
Program Date and Location
_________________________________
Approximate time for complete self study
Physicians Credit Designation:
Home Study: Albert Einstein College of Medicine designates this educational activity for a maximum of 5 AMA
PRA Category 1 Credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity.
Pharmacists Credit Designation:
The New York State Council of Health-system Pharmacists is accredited by the Accreditation Council for Pharmacy
Education as a provider of continuing pharmacy education. The self study component of Antimicrobial Stewardship
Program is approved for 5 hours (0.5CEUs) of continuing pharmacy credit. The ACPE Universal Program Number for the self study is 0134-0000-11-030-H01-P. A statement of continuing pharmacy education credit will be awarded upon successfully achieving a passing score of 70% or higher. To earn a Certificate of Achievement for the complete certificate training program, participants must also complete a live training seminar in addition to the self study modules and the final assessment examination.
Please circle your answers (only one answer per number).
1.
a b c d 9.
a b c d
2.
a b c d 10.
a b c d
3.
a b c d
4.
a b c d
11.
a b c d
12.
a b
5.
a b c d
6.
a b c d e
13.
a b c d
14.
a b
7.
a b c d 15.
a b
8.
a b c d 16.
a b c d
17.
a b c d
18.
a b c d
19.
a b c d
20.
a b c d e
21.
a b c d e
22.
a b c d e
23.
a b c d e
24.
a b c d e
2011 New York State Council of Health-system Pharmacists
25.
a b c d e
26.
a b c d
27.
a b c d
28.
a b
29.
a b c d
30.
a b c d
16
ASP Self Study Activity Evaluation for Pharmacists June 2011:
Please evaluate the program using the following scale: 4- Excellent; 3- Good; 2- Fair; 1-Poor.
A.
Please rate this self study activity for overall Quality: a.
4 b.
c.
3
2 d.
1
B.
How well did this self study activity meet your individual educational needs for professional development? a.
4 b.
3 c.
2 d.
1
C.
Please rate the effectiveness of the home study reading materials. a.
4 b.
3 c.
2 d.
1
D.
Please rate the appropriateness of the self study and self study exam questions. a.
4 b.
3 c.
2 d.
1
E.
This self study activity did not promote a particular product or company. a.
Agree b.
Disagree
F.
The information from the reading materials (please select all that apply): a.
Reinforced my current practice. b.
Will improve my practice/patient outcomes. c.
Provided new ideas or information I expect to use. d.
Enhances my current knowledge base.
G.
Will the information from the reading materials cause you to make any changes in your practice? a.
Yes b.
No
H.
How committed are you to making these changes: a.
Very committed b.
c.
Committed
Not very committed d.
Not at all committed.
I.
Do you feel future activities on the subject matter are necessary and/or important to your practice? a.
Yes b.
No
J.
Did this self study activity meet the stated learning objectives? a.
b.
Yes
No
(If you indicated no please identify the learning objectives that were not met by the program.)
Additional comments:
2011 New York State Council of Health-system Pharmacists 17
ASP Self Study Activity Evaluation for Physicians June 2011:
Please evaluate the program using the following scale: 4- Excellent; 3- Good; 2- Fair; 1-Poor.
A.
Please rate this self study activity for overall quality: a.
4 b.
c.
3
2 d.
1
B.
How well did this self study activity meet your individual educational needs for professional development? a.
4 b.
3 c.
2 d.
1
C.
Please rate the effectiveness of the home study reading materials. a.
4 b.
3 c.
2 d.
1
D.
E.
Please rate the appropriateness of the self study and self study exam questions. a.
4 b.
3 c.
2 d.
1
This self study activity did not promote a particular product or company. a.
Agree b.
Disagree
F.
The information from the reading materials (please select all that apply): a.
Reinforced my current practice. b.
Will improve my practice/patient outcomes. c.
Provided new ideas or information I expect to use. d.
Enhances my current knowledge base.
G.
Will the information from the reading materials cause you to make any changes in your practice? a.
Yes b.
No
H.
How committed are you to making these changes: a.
Very committed b.
c.
Committed
Not very committed d.
Not at all committed.
I.
Do you feel future activities on the subject matter are necessary and/or important to your practice? a.
Yes b.
No
J.
Did this self study activity meet the stated learning objectives? a.
b.
Yes
No
(If you indicated no please identify the learning objectives that were not met by the program.)
Additional comments:
2011 New York State Council of Health-system Pharmacists 18
New York State Council of
Health-system Pharmacists
2 Pine West Plaza, Washington Avenue Extension,
Albany, NY 12205
518-456-8819
2011 New York State Council of Health-system Pharmacists 19