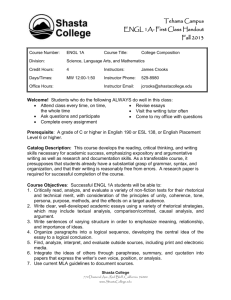
internal medicine residency program
advertisement

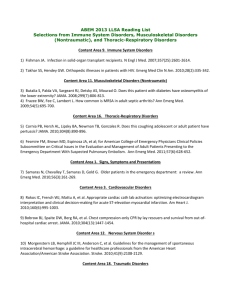
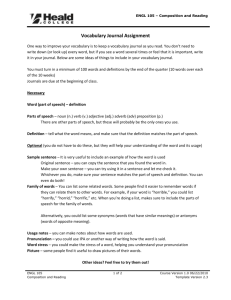
PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM SECTION 13: HEMATOLOGY/ ONCOLOGY This section has been reviewed and approved by the Chief, Division of Hematology and Oncology as well as the Program Director, Internal Medicine Residency Program at Prince George’s Hospital Center. ______________________________ ______________________________ Chief, Division Of Hematology/Oncology Program Director, Residency Program I. Overview Medical Oncology involves the diagnosis and management of benign and malignant neoplasms. The general internist should have a wide range of competencies in the evaluation and management neoplastic disease. They must be able to do the following: (1) Identify patients at risk for malignancy and counsel them regarding risk reduction and screening (2) Investigate clinical syndromes suggestive of underlying malignancy (3) Undertake the palliative care of patients with common solid and hematologic tumors (4) Identify neoplasms with a potential for cure and direct affected patients to the appropriate centers or providers (5) Participate in the difficult decisions regarding all aspects of management including diagnostic evaluation and screening, treatment, and palliative care. (6) Be familiar with the administration, side effects, and drug interactions of therapeutic agents commonly used for the treatment of malignant disease. Hematology relates to the care of patients with disorders of the blood, bone marrow, and lymphatic systems. These disorders include the anemias, hematologic malignancies and other clonal processes, and congenital and acquired disorders of hemostasis, coagulation, and thrombosis. The general internist should be competent in the following: (1) Detection of abnormal physical, laboratory, and radiologic findings relating to the lymphohematopoietic system (2) Assessment of the need for bone marrow aspirate and biopsy or lymph node biopsy (3) Initial diagnostic evaluation and management of the hemostatic and clotting system (4) Assessment of the indications and procedure for transfusion of blood and its separate components (5) Management of therapeutic and prophylactic anticoagulation (6) Diagnosis and management of the common anemias (7) Management of neutropenia / immunosuppression (8) Recognition and management of elevated RBC, WBC and platelets (9) Pharmacology and use of common chemotherapies II. Principle Teaching Methods It consists of frequent encounters with the attending physician regarding patient care. The resident will discuss all patients with the attending physician and interpret clinical data to formulate a differential. The attending will assign reading topics on a regular basis and review the material with the residents. This will include accepted national guidelines used in the diagnosis and treatment of various hematologic and oncologic diseases. The faculty will also critique the residents consult notes, examination and management plan. Rounds will include short 15-30 minute discussions on current topics driven by patient encounters and initiated by resident and completed by the attending physician on most days. Latest information dealing with the topic as provided by literature search and pertinent articles should be discussed. Residents will attend the outpatient clinic with Dr. Chhabra three half days each week during the rotation to gain experience in issues related to outpatient management of hematologic and oncologic illnesses. This includes issues related to : Intravenous Access for chemotherapy Follow-up of patients with malignancies and those on chemotherapy and radiation therapy Follow-up of cancer survivors Follow up of patients with hematologic diseases like sickle cell The Outpatient attendance sheet is attached at the end of this section. Residents must have the sheet signed by the supervising attending for each outpatient encounter and submit the sheet to the program coordinator at the end of the rotation. There will be lectures on a Heme/Onc related topic each month (“Disease of the Month”). The discussions will be as follows: January- lung cancer February- breast cancer March- colon cancer April- leukemia May- lymphoma June- myelodysplasia July- oncologic and hematologic emergencies August- anemias September- thrombocytopenia October- coagulopathies November- measuring performance status, introduction to malignant disease, radiation therapy December- prostate cancer The residents will therefore receive lectures and updates on cancer each month throughout their residency. During their rotation in the subspecialty residents will be required to present a case related to the Disease of the Month. The resident must also review and discuss with the attending the topics highlighted in the logsheet at the end of this section. The residents must print out a double sided copy of the Logsheet and complete the requirements during the rotation. At the end of the rotation the residents must submit the completed logsheet to the program coordinator as requirement for successful completion of the rotation. III. Strengths and Limitations The residents will be exposed to a broad range of clinical problems typical of a community-based practice with emphasis on inpatient illness and care. The teaching faculty for the rotation is committed to teaching and patient care with strong role model presentation. For patients with exceptionally unusual clinical problems, the care may require transfer to a tertiary referral center. Outpatient experience in the subspecialty can be obtained by shadowing the attending physician in their private office. Patients in the continuity clinic at Glenridge Medical Center also offer some learning opportunities regarding prevention, screening and long term follow-up of patients with hematologic illnesses or cancers. IV. Goals and Objectives Legend of Learning Activities Learning Venues: 1. Direct Patient Care/Consultation 2. Attending Rounds 3. Core Lecture Series 4. Self Study Evaluation Methods: A. Attending Evaluation B. Direct Observation C. Nurses’ Evaluation D. In-training Examination Competency: Patient Care Learning Venues Evaluation Methods Demonstrate the ability to obtain an accurate patient history regarding risks for cancer / prior malignancy / hematologic abnormalities / bleeding disorders / status of disease / prior treatment Demonstrate the ability to perform a thorough physical examination on patients with malignancy and/or hematologic disease 1,2,4 A, B 1,2 A, B Demonstrate ability to generate differential diagnosis, diagnostic strategy, and to define appropriate therapeutic plan and modifications to ongoing therapy in patients with malignancy 1,2,3,4 A, B Demonstrate the ability to generate differential diagnosis, diagnostic strategy, and to define appropriate therapeutic plan and modifications to ongoing therapy in patients with a hematologic disorder 1,2,3,4 A, B, Competency: Medical Knowledge Learning Venues Evaluation Methods Demonstrate the ability to recognize an oncologic or hematologic emergency 1,2,3,4 A, B Articulate the genetic predisposition to, and the pathophysiology, evaluation, and management of common hematologic disorders 1,2,3,4 A, B, D Articulate the genetic predisposition to, and the pathophysiology, evaluation, and management of common malignancies 1,2,3,4 A, B, D Demonstrate the ability to monitor a patient’s progress and respond to a change in the patient’s condition during treatment for malignancy (chemotherapy) 1,2,4 A, B, C Demonstrate the ability to order and interpret the appropriate diagnostic tests and studies for a given patient with hematologic abnormalities (bleeding/clotting disorders) 1,2,4 A, B, D Demonstrate the ability to order and interpret the appropriate diagnostic tests and studies for a given patient with malignancy 1,2,4 A, B, D Demonstrate an understanding of pertinent procedures in the work-up and treatment of hematologic/oncologic disease (bone marrow biopsy, lymph node biopsy, etc.), including indications, risks and complications of the procedures 1,2,4 A,B, D Competency: Interpersonal and Communication Skills Learning Venues Evaluation Methods Interact in an effective way with physicians and nurses participating in the care of patients with hematologic/oncologic diseases 1,2 A, B, C Show understanding of differing patient preferences in diagnostic evaluation and management of malignancy Demonstrate the ability to maintain accurate medical records Demonstrate the ability to serve as a patient advocate 1,2 A, B, C 1,2 A, B, C 1,2 A, B, C Competency: Professionalism Learning Venues Evaluation Methods Treat team members, primary care-givers, and patients with respect and empathy Demonstrate understanding of and adherence to a code of medical ethics 1,2 A, B, C 1,2 A, B, C Actively participate in consultations and rounds 1,2 A, B, C Attend and participate in all scheduled conferences 3 Attendance, A Competency: Practice-Based Learning Learning Venues Evaluation Methods Identify limitations of medical knowledge in evaluation and management of patients with hematologic and oncologic disorders and use medical literature (primary and reference) to address these gaps in medical knowledge 1,2,4 A, D Competency: Systems-Based Practice Learning Venues Evaluation Methods Understand need for effective communication between multiple caregivers and sites (eg, hematologists, oncologists, primary care physicians, surgeons, radiation oncologists, chemo nurses, social workers, hospitals, out-patient infusion units) in delivering optimal care to heme/onc patients Understanding of clinical trial design and the statistical methods for evaluating scientific studies, in cooperation with attendings, fellows and research nurses/personnel 1,2,4 A 1,2,5 A, B, C V. Educational Content A. Hemostasis and Thrombosis 1) Learn the causes and management of: Abnormal coagulation (abnormal prothrombin and partial thromboplastin times) Anticardiolipin antibody syndrome Anticoagulation, fibrinolysis (therapeutic) Disseminated intravascular coagulation Hypercoagulable state Hyperviscosity syndrome Heparin, Coumarin, Fibrinolytic Agents and Thrombolytic Disorders Hemophilia 2) Know indications and interpretation of the following: Bone marrow aspirate, biopsy, and special stains Chromosome analysis-peripheral blood and bone marrow Clotting assay, including factor levels and mixing studies Hemoglobin electrophoresis Iron studies B. Platelet disorders Platelet dysfunction Thrombocytopenia Thrombocytosis C. Leukocyte disorders Leukemoid reaction Immunosuppression Neutropenia D. Myeloproliferative disorders 1) Learn diagnosis and management of: Chronic myelogenous leukemia Polycythemia vera Essential thrombocytosis Polycythemia, secondary Acute Leukemia Chronic Leukemia 2) Understand indications and interpret results of Peripheral smear Radiologic, sonographic, and nuclear studies to assess adenopathy, splenomegaly, and red cell mass etc. E. Red Cell Disorders Anemia Hemoglobinopathies and Thalassemias Erythrocytosis Aplastic Anemia Pure Red Cell Aplasia PNH Myelodysplasia Transfusion and Component Therapy Transfusions reactions Iron Overload/ Hemochromatosis F. Miscellaneous Hypersplenism Immunoglobulins Monoclonal Protein Disturbance The Soluble Coagulation System Febrile neutropenia Management of pain, emesis, and nutrition Advance planning and management of end-of-life issues G. Dermatologic Actinic keratosis (see also Dermatology) Basal cell carcinoma (see also Dermatology) Melanoma (see also Dermatology) Squamous cell carcinoma (see also Dermatology) H. Gastrointestinal Cancer of the anus Cancer of the colon, rectum Cancer of the esophagus Cancer of the gallbladder, bile ducts Cancer of the pancreas I. Cancer of the stomach Hepatoma Metastatic disease to various sites Genitourinary Cervical dysplasia and cancer Endometrial cancer Kidney cancer Ovarian cancer Prostate cancer Testicular cancer Ureter, bladder cancer J. Head and Neck Cancer of the head, neck Cancer of the parathyroid Cancer of the thyroid K. Hematologic malignancies and lymphoma 1) Understand diagnosis and management of: Chronic lymphocytic leukemia Hodgkin’s and non-Hodgkin’s lymphomas Leukemia, acute Multiple myeloma Myelodysplastic syndrome 2) Understand indications and interpretation of results of: Lymph node biopsy and lymphoid cell immunophenotype Radiologic, sonographic, and nuclear studies to assess adenopathy, splenomegaly, and red cell mass L. Neurologic CNS lymphoma Metastatic disease to the CNS Primary brain tumors M. Oncologic Emergencies Depressed CNS function due to brain malignancy Hypercalcemia Pericardial tamponade Renal failure due to uteral obstruction Spinal cord compression Tumor lysis syndrome N. Pulmonary Bronchial carcinoid Cancer of the lung Mediastinal tumors Pleural malignancy Superior vena cava syndrome O. Breast cancer Premenopausal and postmenopausal Estrogen and progesterone receptor positive and negative P. Malignancies associated with HIV VI. Recommended Reading: All residents are encouraged to complete reading MKSAP sections on Hematology and Oncology. Additional readings on a case-by-case basis should be done using MD Consult and Up to Date. Other recommended readings are as follows: A. Anemia 1) Andrews, NC. Disorders of Iron Metabolism. N Engl J Med. 1999 Dec 23; 341(26): 1986-95. B. Myelodysplasia 1) Heaney ML, Golde DW. Myelodysplasia. N Engl J Med. 1999 May 27; 340(21): 1649-60. C. Acute Myeloid Leukemia 1) Lowenberg B, Downing JR, Burnett A. Acute Myeloid Leukemia. N Engl J Med. 1999 Sep 30; 341(14): 1051-62. 2) Cheson BD, Bennett JM, Kopecky KJ, et al. Revised Recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol. 2003 Dec 15; 21(24):4642-9. 3) Pui CH, Relling MV, Downing JR. Acute Lymphoblastic Leukemia. N Engl J Med. 2004 Apr 8; 350(15): 1535-48. D. Chronic Myeloid Leukemia 1) Sawyers CL. Chronic Myeloid Leukemia. N Engl J Med. 1999 Apr 29;340(17):1330-40. 2) Faderl S, Talpaz M, Estrov Z, et al. The Biology of Chronic Myeloid Leukemia. N Engl J Med. 1999 Jul 15; 341(3): 164-72. 3) Goldman JM, Melo JV. Chronic Myeloid Leukemia- Advances in Biology and New Approaches to Treatment. N Engl J Med. 2003 Oct 9; 349(15): 1451-64. E. Chronic Lymphocytic Leukemia 1) Shanafelt TD, Call TG. Current Approach to Diagnosis and Management of Chronic Lymphocytic Leukemia. Mayo Clin Proc. 2004 Mar; 79(3): 388-98. F. Hodgkin’s Disease 1) DeVita VT. Hodgkin’s Disease-Clinical Trials and Travails. N Engl J Med. 2003 Jun 12;348(24):2375-6. G. Non-Hodgkin’s Lymphoma 1) Coiffier B, Lepage E, Briere J, et al. CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large B cell lymphoma. N Engl J Med. 2002 Jan 24; 346(4): 235-42. 2) Ansell SM. Non-hodgkin lymphoma: diagnosis and treatment. Mayo Clin Proc. 2005; 89(8): 1087-1097 H. Multiple Myeloma 1) Barlogie B, Shaughnessy J, Tricot G, et al. Treatment of multiple myeloma. Blood. 2004 Jan 1; 103(1): 20-32. I. Chronic Myeloproliferative Disorders 1) Tefferi A. Polycythemia Vera: A Comprehensive Review and Clinical Recommendations. Mayo Clin Proc. 2003 Feb; 78(2): 174-94. 2) Tefferi A. Myelofibrosis with Myeloid Metaplasia. N Engl J Med. 2000 Apr 27; 342(17): 1255-65. J. Hemachromatosis 1) Beutler E. Penetrance in hereditary hemachromatosis. The HFECys282Tyr as a necessary but not sufficient cause of clinical hereditary hemachromatosis. Blood. 2003 May 1;101(9):3347-50. K. Thrombotic Disorders 1) Rosendaal FR. Venous Thrombosis: A multicausal disease. Lancet. 1999 Apr 3;353(9159):1167-73. 2) Levine M, Gent M, Hirsh J, et al. A Comparison of Low Molecular Weight Heparin administered primarily at home with Unfractionated Heparin administered in the hospital for Proximal Deep Vein Thrombosis. N Engl J Med. 1996 Mar 14;334(11):677-81. 3) Quinlan DJ, McQuillan A, Eikelboom JW. Low Molecular Weight Heparin Compared with intravenous Unfractionated Heparin for Treatment of Pulmonary Embolism. Ann Intern Med. 2004 Feb 3;140(3):175-83. 4) Shapiro SS. Treating Thrombosis in the 21st Century. N Engl J Med. 2003 Oct 30;349(18):1762-4. L. Bleeding Disorders 1) Mannucci PM, Tuddenham EGD. The Hemophilias-From Royal Genes to Gene Therapy. N Engl J Med. 2001 Jun 7;344(23):1773-9. 2) Mannucci PM. Treatment of von Willebrand’s Disease. N Engl J Med. 2004 Aug 12;351(7):683-94. M. Disorders of Platelets 1) Drachman JG. Inherited thrombocytopenia: when a low platelet count does not mean ITP. Blood. 2004 Jan 15;103(2):390-8. 2) Cines DB, Blanchette VS. Immune Thrombocytopenia purpura. N Engl J Med. 2002 Mar 28;346(13):995-1008. 3) Stasi R, Provan D. Management of Immune Thrombocytopenia in Adults. Mayo Clin Proc. 2004 Apr;79(4):504-22. 4) Moake JL. Thrombotic Microangiopathies. N Engl J Med. 2002 Aug 22;347(8):589-600. 5) George JN. Thrombotic Thrombocytopenic Purpura: From the Bench to the Bedside, but Not yet to the Community. Ann Intern Med. 2003 Jan 21;138(2):152-3. 6) Alving BM. How I treat heparin-induced thrombocytopenia and thrombosis. Blood. 2003 Jan 1; 101(1): 31-7. N. Hemoglobinopathies 1) Olivieri NF. The ß- Thlassemias. N Engl J Med. 1999 Jul 8;341(2):99-109. 2) Steinberg MH. Management of Sickle Cell Disease. N Engl J Med. 1999 Apr 1;340(13):1021-30. O. Breast Cancer 1) Clemons, M, Goss, P., Estrogen and the Risk of Breast Cancer, NEJM 344(4):276-85, January 25, 2001. 2) Meijers-Heijboer, H., et al., Breast Cancer after Prophylactic Bilateral Mastectomy in Women with a BRCA-1 or BRCA-2 Mutation, NEJM 345(3):15964, July 19, 2001. 3) Vallis, K.A., et al., Assessment of Coronary Heart Disease Morbidity and Mortality after Radiation Therapy for Early Breast Cancer, J Clinical Oncology 20(4):1036-42, February 15, 2002. P. Colorectal Cancer/Other GI Cancer 1) Huang, J.Q., Meta-analysis of the Relationship between Helicobacter Pylori Seropositivity and Gastric Cancer, Gastroenterology 114(6): 1169-79, June 1998. 2) Lieberman, D.A., et al., Use of Colonoscopy to Screen Asymptomatic Adults for Colorectal Cancer, Veterans Affairs Cooperative Study Group 380, NEJM 343(3): 162-8, July 20, 2000. Q. Lung Cancer 1) Newman, L., Larger Debate Underlies Spiral CT Screening for Lung Cancer, J National Cancer Institute, 92(8):592-4, April 19, 2000. R. Prostate Cancer 1) Sirovich, B.E., et al., Screening Men for Prostate and Colorectal Cancer in the United States:Does Practice Reflect the Evidence?, JAMA 289(11):1414-20, March 19, 2003. S. Miscellaneous Topics 1) Arany, I., Safirstein, R.L., Cisplatin Nephrotoxicity, Seminars in Nephrology 23(5):460-4, September 3, 2003. 2) Callee, E.E., et al., Overweight, Obesity, and Mortality from Cancer in a Prospectively Studied Cohort of U.S. Adults, NEJM 348(17):1625-38, April 24, 2003. 3) Lee, A., et al., Low-Molecular Weight Heparin versus Coumarin for the Prevention of Recurrent Venous Thromboembolism in Patients with Cancer, NEJM 349(2):146-53, July 10, 2003. 4) Rosen, L.S., et al, Long-Term Efficacy of Zolendronic Acid in Patients with Bone Metastases, Cancer 100:2613-2621, 2004. 5) Walter, L.C. et al., Relationship between Health Status and Use of Screening Mammography and Papanicolaou Smears among Women Older Than 70 Years of Age, Ann Intern Med 140(9):681-688, 2004. PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM HEMATOLOGY/ONCOLOGY LOGSHEET RESIDENT NAME______________________________________________ PGY LEVEL_______________ TEST MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE PERIPHERAL SMEAR ROTATION MONTH_____________ BIOPSY REVIEW PATHOLOGY REPORT( RECEPTORS/ TUMOR MARKERS) STAGING OF CANCER RESIDENT NAME: TEST MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE MR# Interpretation of result by resident (diagnosis) Comment by supervising attending (correct/not, missed findings etc) SIGNATURE of Supervising attending & DATE PERIPHERAL SMEAR BIOPSY REVIEW PATHOLOGY REPORT( RECEPTORS/ TUMOR MARKERS) STAGING OF CANCER PRINCE GEORGE’S HOSPITAL CENTER INTERNAL MEDICINE RESIDENCY PROGRAM HEMATOLOGY/ONCOLOGY OUTPATIENT ATTENDANCE SHEET RESIDENT NAME______________________________________________ PGY LEVEL_______________ DATE ROTATION MONTH_____________ COMMENTS (IF ANY) BY ATTENDING SIGNATURE OF ATTENDING