2 major components of the immune system:
advertisement
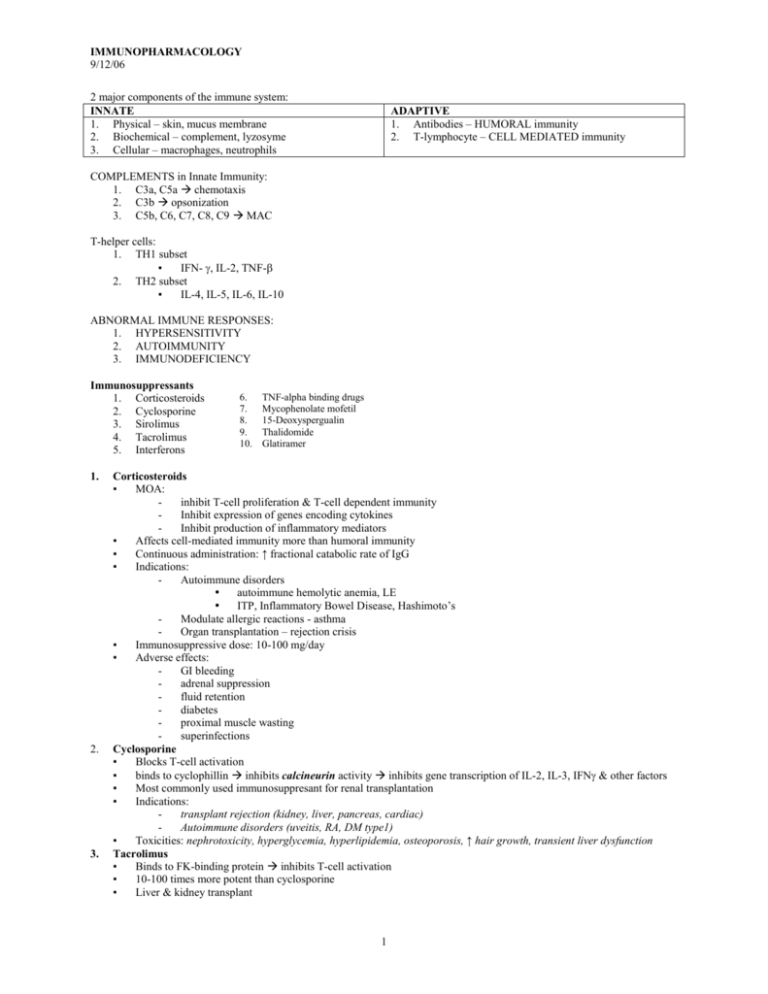
IMMUNOPHARMACOLOGY 9/12/06 2 major components of the immune system: INNATE 1. Physical – skin, mucus membrane 2. Biochemical – complement, lyzosyme 3. Cellular – macrophages, neutrophils ADAPTIVE 1. Antibodies – HUMORAL immunity 2. T-lymphocyte – CELL MEDIATED immunity COMPLEMENTS in Innate Immunity: 1. C3a, C5a chemotaxis 2. C3b opsonization 3. C5b, C6, C7, C8, C9 MAC T-helper cells: 1. TH1 subset ▪ IFN- , IL-2, TNF- 2. TH2 subset ▪ IL-4, IL-5, IL-6, IL-10 ABNORMAL IMMUNE RESPONSES: 1. HYPERSENSITIVITY 2. AUTOIMMUNITY 3. IMMUNODEFICIENCY Immunosuppressants 1. Corticosteroids 2. Cyclosporine 3. Sirolimus 4. Tacrolimus 5. Interferons 1. 2. 3. 6. 7. 8. 9. 10. TNF-alpha binding drugs Mycophenolate mofetil 15-Deoxyspergualin Thalidomide Glatiramer Corticosteroids ▪ MOA: inhibit T-cell proliferation & T-cell dependent immunity Inhibit expression of genes encoding cytokines Inhibit production of inflammatory mediators ▪ Affects cell-mediated immunity more than humoral immunity ▪ Continuous administration: ↑ fractional catabolic rate of IgG ▪ Indications: Autoimmune disorders autoimmune hemolytic anemia, LE ITP, Inflammatory Bowel Disease, Hashimoto’s Modulate allergic reactions - asthma Organ transplantation – rejection crisis ▪ Immunosuppressive dose: 10-100 mg/day ▪ Adverse effects: GI bleeding adrenal suppression fluid retention diabetes proximal muscle wasting superinfections Cyclosporine ▪ Blocks T-cell activation ▪ binds to cyclophillin inhibits calcineurin activity inhibits gene transcription of IL-2, IL-3, IFN & other factors ▪ Most commonly used immunosuppresant for renal transplantation ▪ Indications: transplant rejection (kidney, liver, pancreas, cardiac) Autoimmune disorders (uveitis, RA, DM type1) ▪ Toxicities: nephrotoxicity, hyperglycemia, hyperlipidemia, osteoporosis, ↑ hair growth, transient liver dysfunction Tacrolimus ▪ Binds to FK-binding protein inhibits T-cell activation ▪ 10-100 times more potent than cyclosporine ▪ Liver & kidney transplant 1 IMMUNOPHARMACOLOGY 9/12/06 4. 5. ▪ Oral or IV : t½ = 9-12 hrs ▪ Toxicity: nephrotoxicity, neurotoxicity, hyperglycemia, GI dysfunction Sirolimus (Rapamycin) ▪ Binds also to immunophyllin blocks the response of T-cell to cytokines ▪ Potent inhibitor of B-cell proliferation & Ig production ▪ Indications: Kidney & heart allografts C syclosporin psoriasis & uveoretinitis Interferon ▪ Type 1: induced by viral inf. IFN-alpha prod. by leukocytes IFN-beta fibroblasts & epithelial cells ▪ Type 2: IFN-gamma produced by activated T-lymphocytes ▪ Indications: cancer ▪ IFN- multiple sclerosis ▪ IFN- chronic granulomatous disease Newer Immunosuppressants 1. TNF-α binding drugs: ▪ INFLIXIMAB Chimeric IgG1 monoclonal antibody with human region & murine regions Suppress generation of cytokines Crohn’s disease; RA ▪ ETANERCEPT Chimeric protein with human regiom Similar MOA with infliximab but shorter half-life RA 2. Mycophenolate Mofetil ▪ Inhibits a series of T & B lymphocyte responses ▪ Inhibit de novo pathway of purine synthesis ▪ Renal & heart transplantation ▪ Mizoribine – inhibits nucleotide synthesis PW; kidney transplants ▪ Brequinar Sodium – inhibits de novo pathway of pyrimidine synthesis; cancer & organ transplantation 3. 15-Deoxyspergualin ▪ Potent antimonocytic & antilymphocytic effect ▪ Inhibits T & B lymphocyte response ▪ Renal transplants; pancreas & heart transplants 4. Thalidomide ▪ Sedative drug ▪ Favors TH2 over TH1 ▪ Suppress TNF-α production ▪ Antiangiogenesis action: teratogenicity & anticancer ▪ Indications i. Erythema nodosum leprosum (skin manifestations of SLE) ii. Lung transplantation 5. Glatiramer ▪ Relapsing-remitting form of multiple sclerosis ▪ Subcutaneous injection ▪ Toxicities: Transient post-injection reaction CYTOTOXIC Agents: 1. Azathioprine Metabolized to 6-mercaptopurines Inhibit purine synthesis interferes with nucleic acid metabolism inhibits cellular & humoral responses Highly teratogenic Well absorbed from GI tract Renal allograft, AGN, SLE(renal), RA, Crohn’s disease Prednisone-resistant antibody-mediated ITP Autoimmune hemolytic anemia Toxicities: Bone marrow suppression GI disturbances: N&V, diarrhea 2 IMMUNOPHARMACOLOGY 9/12/06 2. 3. Skin rashes, drug fever, hepatic dysfunction Leflunomide Prodrug of an inhibitor of pyrimidine synthesis Inhibits lymphoid cells Orally active RA Toxicities: Headache, nausea & diarrhea Hepatic dysfunction, renal impairment Teratogenic Cyclophosphamide Most potent immunosuppressive drug Destroys proliferating lymphoid cells Autoimmune disorders: SLE Acquired factor XIII antibodies Bleeding syndromes Toxicities: Pancytopenia, hemorrhagic cystitis Antibodies as Immunosuppressive Agents Antibodies as Immunosuppressive Agents 1. Antilymphocytic antibody 2. Immune Globulin IV 3. Hyperimmune Immunoglobulins 4. Monoclonal Antibodies 5. Rho(D) Immune Globulin Micro-Dose Prevention of hemolytic disease of the newborn Given to mother within 72 hrs after delivery of an Rh-negative baby i. Muromonab- CD3 A T-cell specific antibody Renal transplantation, heart / renal ii. Palivizumab – RSV iii. Rituxumab – follicular B-cell non-hodgekins lymphma iv. Trastuzumab – metastatic breast CA IMMUNOMODULATORS 1. CYTOKINES ▪ Interferon-alpha: hairy cell leukemia chronic myelogenous leukemia malignant melanoma Kaposi’s sarcoma anticancer renal cell CA, carcinoid syndrome, T cell leukemia Interferon-beta Interferon-gamma Interleukin-2 TNF-alpha Interferons & IL-2 GM-CSF 2. 3. Relapsing type multiple sclerosis Chronic granulomatous disease Metastatic renal cell CA Malignant melanoma Malignant melanoma Soft tissue sarcoma of extremities (+) effects in response to Hep B vaccine Melanoma and Prostate cancer LEVAMISOLE: antiparasitic agent potentiate action of fluorouracil in adjuvant therapy of Dukes class C colorectal CA other uses: hodgkin’s lymphoma RA BCG (Bacille-Camille-Guarin): immunization against tuberculosis Adjuvant in intravesical therapy for SF bladder CA 3








