file
advertisement
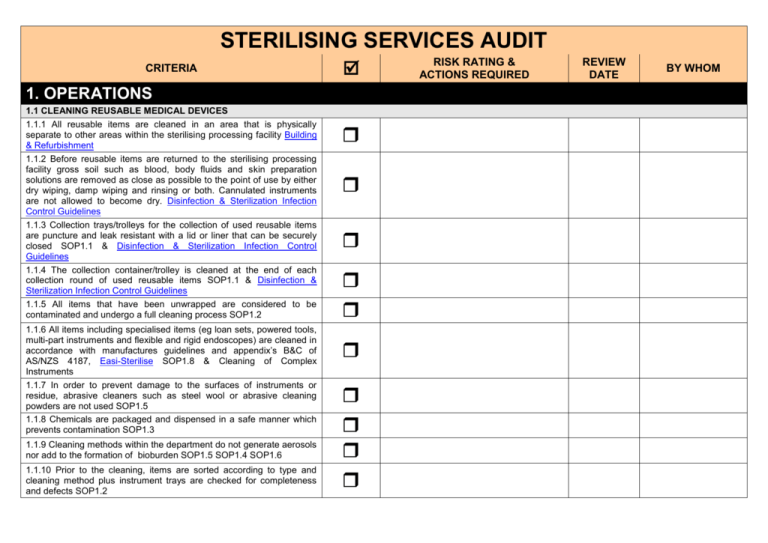
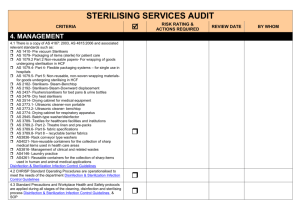
STERILISING SERVICES AUDIT CRITERIA 1. OPERATIONS 1.1 CLEANING REUSABLE MEDICAL DEVICES 1.1.1 All reusable items are cleaned in an area that is physically separate to other areas within the sterilising processing facility Building & Refurbishment 1.1.2 Before reusable items are returned to the sterilising processing facility gross soil such as blood, body fluids and skin preparation solutions are removed as close as possible to the point of use by either dry wiping, damp wiping and rinsing or both. Cannulated instruments are not allowed to become dry. Disinfection & Sterilization Infection Control Guidelines 1.1.3 Collection trays/trolleys for the collection of used reusable items are puncture and leak resistant with a lid or liner that can be securely closed SOP1.1 & Disinfection & Sterilization Infection Control Guidelines 1.1.4 The collection container/trolley is cleaned at the end of each collection round of used reusable items SOP1.1 & Disinfection & Sterilization Infection Control Guidelines 1.1.5 All items that have been unwrapped are considered to be contaminated and undergo a full cleaning process SOP1.2 1.1.6 All items including specialised items (eg loan sets, powered tools, multi-part instruments and flexible and rigid endoscopes) are cleaned in accordance with manufactures guidelines and appendix’s B&C of AS/NZS 4187, Easi-Sterilise SOP1.8 & Cleaning of Complex Instruments 1.1.7 In order to prevent damage to the surfaces of instruments or residue, abrasive cleaners such as steel wool or abrasive cleaning powders are not used SOP1.5 1.1.8 Chemicals are packaged and dispensed in a safe manner which prevents contamination SOP1.3 1.1.9 Cleaning methods within the department do not generate aerosols nor add to the formation of bioburden SOP1.5 SOP1.4 SOP1.6 1.1.10 Prior to the cleaning, items are sorted according to type and cleaning method plus instrument trays are checked for completeness and defects SOP1.2 RISK RATING & ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA 1.1.11 Cleaning methods used are appropriate for the design of the items being processed SOP1.2 1. OPERATIONS cont. 1.1 CLEANING REUSABLE MEDICAL DEVICES 1.1.12 Any defective instruments are cleaned, dried and sterilised prior to being sent for repairs SOP1.2 1.1.13 Loan instruments undergo a cleaning process prior to being wrapped for sterilisation. Any soil or debris found on the loan instruments are reported to the supplier SOP1.2 1.1.14 Prior to returning loan instruments to the source they are to undergo a cleaning and sterilising process Disinfection & Sterilization Infection Control Guidelines 1.1.15 At the completion of the cleaning process, items are visually inspected to ensure they are clean and free from detergent residue SOP2.5 1.1.16 All equipment and instruments undergo a mechanical cleaning process appropriate for the item and the items are processed for the complete cycle SOP1.9 to SOP1.11 1.1.17 Automated washer disinfector machines have the following cycles: pre-rinse with water wash, in warm water and cleaning agent as per manufacturers recommendations one or more rinses with hot water at 80°C-90°C, with drying agent added drain, leaving contents at a temperature for quick drying drying, either by radiant heat from an element or hot air blast SOP1.9 to SOP1.11 1.1.18 All anaesthetic equipment undergo mechanical cleaning are disassembled as required prior to processing and care taken to ensure all surfaces and lumens are exposed to the cleaning process SOP1.13 1.1.19 Each time the ultrasonic cleaner is filled, water is added first, next the manufacturers recommended detergent followed by degassing of the machine before instruments are placed in the basket for processing SOP1.13 RISK RATING & ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA 1. OPERATIONS cont. 1.1 CLEANING REUSABLE MEDICAL DEVICES 1.1.20 Ultrasonic cleaner is used to clean jointed, serrated, cannulated instruments not insulated instruments, mirrors or lenses SOP1.13 1.1.21 When items are removed following being cleaned in an ultrasonic they are rinsed in warm to hot water prior to drying SOP1.13 1.1.22 The ultrasonic solution is replaced at least daily or when the solution is contaminated SOP1.13 1.1.23 On completion of a mechanical cleaning cycle items (including anaesthetic equipment) are placed in a drying cabinet where the temperature range is between 65° C to 75° C SOP1.15 1.1.24 Safety instructions are followed during the operation of all mechanical washers eg mechanical lifters for heavy equipment, lid is kept closed during ultrasonic operation and no part of the operators body is submerged inside the water tank of an ultrasonic cleaner during operation SOP1.13 1.1.25 At the end of each cleaning session the manual cleaning equipment is cleaned and thermally disinfected or sterilised SOP1.5 1.1.26 Powered instruments and hoses are cleaned as follows kept clean during surgical procedure cleaned with low-linting cloth, detergent and water not immersed in water not placed in a mechanical washer hose and handpiece to stay attached during cleaning inspect for wear and tear detergent rinsed off items drying cabinet to dry items test prior to sterilisation damaged tools and hoses sent for repair by a qualified person SOP1.8 RISK RATING & ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA ACTIONS REQUIRED REVIEW DATE BY WHOM 1. OPERATIONS cont. 1.1 CLEANING REUSABLE MEDICAL DEVICES 1.1.27 Cleaning flexible and ridged endoscopes involves immediately following the procedure the endoscope insertion tube is to be wiped clean using clean water and an enzymatic cleaning solution enzymatic solution is aspirated through the suction channel and water and air is fed via the water/air channels (if applicable) all endoscopes are leak tested prior to immersion the endoscope is dismantled according to manufacturers instructions components are cleaned with an enzymatic solution diluted according to manufacturers instructions all taps are opened channels/lumen of the endoscope are brushed to remove any debris cleaning process continues till the item is completely clean flush rinsing is carried out to remove traces of enzyme/detergent accessory items are placed in an ultrasonic cleaner following manufactures instructions accessory items are flushed and rinsed following cleaning brushes used for cleaning the channels and lumens are cleaned and thermally disinfected after each use after flush rinsing the endoscope and accessory item is thoroughly dried internal lumens are purged with air Endoscopy and Easi-Sterilise Cleaning of Complex Instruments ADEQUATE (100%) OVERALL COMMENTS FOR THIS SECTION: REQUIRES IMPROVEMENT (>70% = 19/27) INADEQUATE (<70%) STERILISING SERVICES AUDIT CRITERIA 1. OPERATIONS cont. 1.2 PACKAGING & WRAPPING 1.2.1 Individual packs do not include combinations of hollowware, instruments, dressings, drapes or tubing SOP2.5 1.2.2 Instruments with hinges or ratchets are opened and unlocked prior to packing SOP2.5 1.2.3 Instruments with multiple parts are dismantled or loosened prior to being packed in accordance with manufacturers instructions SOP2.5 1.2.4 When packaging instruments sets with delicate items, these items are protected to prevent damage SOP2.5 1.2.5 When packaging sharp instruments the tips are protected to prevent the perforation of the flexible packaging material SOP2.5 1.2.6 When packaging instruments that require lubrication the lubricant is water miscible, compatible with the sterilising process and used in accordance with manufacturers instructions SOP1.3 1.2.7 When packaging hollowware all openings face in the same direction non-porus spacers are used to separate each piece of hollowware contents cannot move inside the pack SOP2.5 1.2.8 When packaging powered instruments and hoses lubricate only as necessary, not inside the hose and follow manufacturers instructions test prior to sterilisation disassemble prior to sterilisation hoses are loosely coiled SOP1.8 1.2.9 When determining size, mass and contents of items, consideration is given to the sterilisers ability to effectively sterilise the pack facilitate the drying process of the pack establishing the efficiency of air elimination from the load SOP2.6 ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA 1. OPERATIONS cont. 1.2 PACKAGING & WRAPPING 1.2.10 Prior to use, textile wraps are laundered and checked for holes or threadbare patches SOP2.6 1.2.11 Only textile wraps as specified in AS3789.2, AS3789.8, AS1079.2, AS1079.5 are used Disinfection & Sterilization Infection Control Guidelines 1.2.12 Hollowware (gallipots) are placed with opening against the paper side of the flexible wrapping material SOP2.6 1.2.13 Nylon packaging material is only used with a dry heat steriliser Disinfection & Sterilization Infection Control Guidelines 1.2.14 Methods used to wrap items complies with AS 4187 page 31-32 SOP2.6 1.2.15 The method used to seal packs include heat sealers and sterilising indicator tape SOP2.6 & SOP2.7 1.2.16 Only suitable equipment is used for heat sealing bags and flexible packaging materials SOP2.7 1.2.17 After heat sealing packs the seal is checked to ensure that it is complete (especially over gusset folds of bags or pouches) SOP2.7 1.2.18 Only non-toxic solvent based felt-tipped marking pens and/or rubber stamps using simular ink are used for labelling packs prior to processing SOP2.6 1.2.19 Each packaged item labelling includes contents of pack batch control data - Steriliser identification number, date of sterilisation and cycle or load number batch control data information is also included in the steriliser log sheet (eg by an additional label) operating suite place the batch control label or barcode from the packaged item into the individual patients operating suite records (SOP3.1 & SOP3.2 ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA ACTIONS REQUIRED REVIEW DATE BY WHOM 1. OPERATIONS cont. 1.2 PACKAGING & WRAPPING ADEQUATE (100%) REQUIRES IMPROVEMENT (>70% = 13/19) OVERALL COMMENTS FOR THIS SECTION: 1.3 STERILISING EQUIPMENT 1.3.1 The methods for processing used in the sterilising facility includes (please identify) steam under pressure dry heat low temperature sterilisation Disinfection & Sterilization Infection Control Guidelines 1.3.2 The sterilising cycle and temperature reflects the type of load and wrapping material Disinfection & Sterilization Infection Control Guidelines 1.3.3 Flash sterilisation is only used in situations where a single instrument has been dropped and there is no duplicate instrument available Disinfection & Sterilization Infection Control Guidelines 1.3.4 Flash sterilisers are only used for unwrapped non-porus items NOT used to process cannulated, complex instruments, suction and other tubing, textiles or paper Disinfection & Sterilization Infection Control Guidelines 1.3.5 Portable sterilisers without a drying cycle are only used for processing unwrapped items Disinfection & Sterilization Infection Control Guidelines 1.3.6 Portable sterilisers with drying cycle are used to process small numbers of simple packs Disinfection & Sterilization Infection Control Guidelines INADEQUATE (<70%) STERILISING SERVICES AUDIT CRITERIA 1.3.7 Dry heat sterilisers are used only to sterilise anhydrous items and items sealed in impermeable containers which can not be sterilised by steam under pressure Disinfection & Sterilization Infection Control Guidelines ACTIONS REQUIRED REVIEW DATE BY WHOM 1. OPERATIONS cont 1.3 STERILISING EQUIPMENT 1.3.8 Instruments that have been processed with liquid sterilants are used immediately following processing Disinfection & Sterilization Infection Control Guidelines 1.3.9 Non-woven wraps or non-cellulose flexible packaging materials are used for Hydrogen Peroxide Plasma Sterilisers Disinfection & Sterilization Infection Control Guidelines 1.3.10 Peracetic acid sterilising equipment – all channels of the flexible endoscope are connected in line for both sterilising and water rinsing cycles, next a one minute purge of filtered air the unit remains sealed until released by the operator Disinfection & Sterilization Infection Control Guidelines ADEQUATE (100%) REQUIRES IMPROVEMENT (>70% = 7/10) OVERALL COMMENTS FOR THIS SECTION: 1.4 LOADING A STERILISER 1.4.1 When loading a steriliser, space is left between items being processed and the items do not come in contact with the chambers walls SOP3.2 1.4.2 Loading patterns and loading techniques are consistent with the sterilisers loading pattern during Performance Qualification SOP3.2 INADEQUATE (<70%) STERILISING SERVICES AUDIT CRITERIA 1.4.3 Flexible packaging material is loaded on the edge of the laminate or placed flat with the paper surface downwards SOP3.2 1.4.4 Flexible endoscopes are processed with the buttons and valves removed Endoscopy and Disinfection & Sterilization Infection Control Guidelines 1.4.5 Accessory items for flexible endoscopes are sterilised using chemical sterilant or packaged and sterilised Endoscopy and Disinfection & Sterilization Infection Control Guidelines 1. OPERATIONS cont. 1.4 LOADING A STERILISER 1.4.6 Once the steriliser is loaded the cycle is commenced SOP3.2 Portable (benchtop), downward displacement and pre-vacuum sterilisers 1.4.7 Hollowware is tilted on its edge at a 45º angle in a draining position and not placed above textile packs Disinfection & Sterilization Infection Control Guidelines 1.4 8 Packs of drapes are loaded with layers vertical Disinfection & Sterilization Infection Control Guidelines 1.4.9 Only a single layer of packs is placed on the loading tray Disinfection & Sterilization Infection Control Guidelines 1.4.10 Items to be sterilised unwrapped are placed on a perforated mesh tray flat on the steriliser shelf with a new chemical indicator placed in the loading tray Disinfection & Sterilization Infection Control Guidelines Hydrogen Peroxide Plasma Sterilisation 1.4.11 Consideration is given to the balance of metal and plastic items being processed together to prevent inadequate processing SOP3.3 1.4.12 Adaptors/boosters are used for lumen instruments SOP3.3 Peracetic Acid Liquid Chemical Sterilisation 1.4.13 Care is taken when loading a machine with a direct flow processing container/tray so that all surfaces are penetrated by the liquid sterilant Endoscopy and Disinfection & Sterilization Infection Control Guidelines ACTIONS REQUIRED REVIEW DATE BY WHOM STERILISING SERVICES AUDIT CRITERIA 1.4.14 In machines with flexible processing trays each instrument channel is directly connected to machines fluid pathways via purposedesigned tubing adaptor kit Endoscopy and Disinfection & Sterilization Infection Control Guidelines ADEQUATE (100%) ACTIONS REQUIRED REVIEW DATE BY WHOM REQUIRES IMPROVEMENT (>70% = 10/14) INADEQUATE (<70%) OVERALL COMMENTS FOR THIS SECTION: 1. OPERATIONS cont. 1.5 UNLOADING OF STERILISERS 1.5.1 The steriliser door is not opened prior to completion of the processing cycle SOP3.2 1.5.2 Cooling items are placed on racks not solid surfaces SOP3.4 1.5.3 Processed items are cooled before being place into new polyethylene dust covers and sealed SOP3.4 1.5.4 When instruments are sterilised in an unwrapped cycle for a sterile set up, the items are unloaded and used immediately using aseptic technique Disinfection & Sterilization Infection Control Guidelines 1.5.5 Peracetic acid liquid chemical sterilisation system – air seal is only released when the cycle is completed Disinfection & Sterilization Infection Control Guidelines 1.5.6 The sterilising parameters are checked prior to a load being released SOP3.4 ADEQUATE (100%) OVERALL COMMENTS FOR THIS SECTION: REQUIRES IMPROVEMENT (>70% = 4/6) INADEQUATE (<70%) STERILISING SERVICES AUDIT CRITERIA ACTIONS REQUIRED REVIEW DATE BY WHOM 1. OPERATIONS cont. 1.6 STORAGE AND HANDLING OF PROCESSED ITEMS 1.6.1 Sterile items are not stored in ultraviolet cabinets or in disinfectants Disinfection & Sterilization Infection Control Guidelines 1.6.2 All unwrapped medical items (including critical, semi-critical and non-critical) undergo a cleaning and sterilising process prior to being stored in a clean dedicated container/draw Disinfection & Sterilization Infection Control Guidelines 1.6.3 Storage containers, trolley and cupboards are clean, dry and in good condition (cardboard boxes are not used) SOP4.2 1.6.4 Access to the sterile stock area is restricted SOP4.2 ADEQUATE (100%) OVERALL COMMENTS FOR THIS SECTION: REQUIRES IMPROVEMENT (>70% = 3/4) INADEQUATE (<70%)