Sterilization and Disinfection for Dummies
advertisement

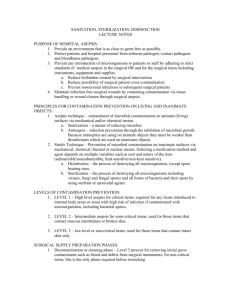
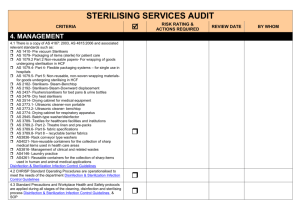
Mission Accomplished: Sterilization & Disinfection Robin Haag Sherry Chisholm 2011 Awardee Baltimore, Maryland What I Attended ? Anything and Everything related to sterilization and disinfection No matter how repetitive No matter how boring Why this topic? We “assume” others are doing the right thing Corners get cut Salary and titles do not equate with knowledge or expertise Common sense is not common TJC and CMS citations We are ultimately responsible Bill Rutala says…… Current surface disinfection practices are not effective 65% of high touch areas are not cleaned Inadequate terminal cleaning puts the next patients at risk for acquiring MDROs Improved methods are needed Risk of Acquiring MRSA, VRE and C Dif from Prior Occupants Admission to previously occupied MRSA or VRE room significantly increases odds of acquisition Prior environmental contamination measured by environmental culture or VRE colonized patients increases risk Huang et al Arch Intern Med 2006; 166;1945. Drees et al Clin Infect Dis 2008; 46:678. Prior room occupant with CDAD significantly increase risk Shaughnessy et al. ICHE 2011; 32:201 Novel Methods of Room Decontamination No touch methods Ultraviolet lights Work best in direct line of sight ~15 minutes for MDROs ~50 minutes for c dif spores Hydrogen Peroxide Systems Supplement, do not replace standard cleaning/disinfection May take hours Rooms need sealing Proposed self disinfecting surfaces Silver or silver ion impregnated Copper Sharklet pattern Deflects organisms from adhering New Approaches to Room Decontamination UV Decontamination Advantages Reliable biocidal activity Surface and equipment decon Room decon ~15 min for vegetative bacteria HVAC can stay on Room need not be sealed Low operating cost UV Decontamination Disadvantages No studies regarding HAI reduction Not for daily cleaning Terminal cleaning only Initial capital equipment cost Does not remove dust or stains Need to determine UV parameters Hydrogen Peroxide Decontamination Advantages Reliable biocidal Surface and equipment decontamination Decreases C difficile Residual free Minimal health or safety concerns Can use on complex equipment Hydrogen Peroxide Decontamination Disadvantages Can only be used for terminal cleaning All patients and staff may not be in room Process takes 3 – 5 hours HVAC must be disabled Room must be sealed with tape Does not remove dust or stains Need to determine HP concentration C. difficile Factors that facilitate transmission Survives in environment for hours to days Remains virulent in the environment Low inoculating dose Colonizes patients Surface contamination Frequently touched by HCWs Direct transmission from contaminated hands Relative resistance to antiseptics and disinfectants Controlling the Spread of C dif Practice Contact precautions Ensure thorough disinfection Products 5000 – 6000 ppm chlorine Products with c dif claims When Areas with increased C dif rates All patient rooms? Surface Disinfection Exposure time Close attention by TJC and CMS Following manufacturers’ directions Dilution Contact time: may require repeat applications Appeals denied by for following findings of peer reviewed studies supporting shorter exposure times Wipes Wet time Size of wipe 2011 Multi-Society for Reprocessing Flexible Endoscopes Changes since 2003 HLD efficacy is unchanged High level disinfectants Automated reprocessors Endoscopes Endoscopic accessories Principles remain valid Outbreaks associated with: ASCs Unfamiliarity with endoscope channels, accessories and attachments Endoscope Procedure Transmission: Non scope related IV lines Anesthesia administration Medication administration Multidose vials Reuse of needles and syringes IV tubing Endoscope Procedure Transmission: Scope related Failure to sterilize forceps between patients Lapses in reprocessing channels used in irrigation Unresolved Endoscope Issues Interval of storage between reprocessing and scope use suggests negligible contamination 7 – 14 days Insufficient data to determine maximal duration Data Need for microbiologic surveillance Disinfection Boot Camp: Rose Seavey and Martha Young Evidence based Guidelines Focus on AAMI/ANSI Standards 2010 NPSGs AORN 2011 CDC 2008 Environmental Concerns 68 – 70° F in clean area 60 – 65° F in decon area 30 – 60% humidity in decon area Not over 70% humidity in sterile storage Separate housekeeping and decontamination cleaning supplies Eye wash stations 60 – 100° F Test weekly for 3 minutes Use AAMI Work flow diagrams Dirty to clean Decontamination Personnel Attire Scrubs Cover all facial hair No artificial nails Prefer no nail polish No jewelry Bouffant caps only Heavy long gloves, not surgical Face masks with full protection splash guards Decontamination Decrease bioburden Water Prepare devices Disassemble Lubricate Keep instruments moist Brush and clean under water Use disposable brushes or decontaminate once per shift Prefer automatic washers Initial rinse can be tap water Final rinse should be sterile, de-ionized, distilled Sterilization Do not use preset parameters for cycles Maintain sterility in storage Event related sterility Potential Problems With Automated Cleaners Wrong water temperature Wrong detergent concentration Problem with mechanical functioning Human element How machine is loaded How Do You Know Your Automatic Washer is Working Right? Verification of Cleaning TOSI (Test Object Surgical Instruments) Monitoring of the Cleaning Efficiency of WasherDisinfectors Surrogate device for surgical instruments soiled with blood Test weekly, preferably daily Maintain records Sterilization Caveats Count sheets should not be inside sets or containers Load configuration Item density Your hand should fit between items Ink transfers Paper shreds Peel packs No more than 1 or 2 small light items Double packing not needed No folds in packs BIs preferred daily Do not exceed 25 lbs including container and wrapper Do process audits Cooling in a high AC environment Immediate use sterilization Old “flash sterilization” Loaners May lead to wet packs Have in 3 days ahead of time Keep repair logs Storage 75°F 4 air exchanges per hour Under 70% humidity Don’t stack Keep items covered 8 – 10 inches above floor 2 inches from outside wall Solid bottom shelf Prevents condensation No corrugated boxes No shipping boxes Tracer Activity Trace a set from patient in OR through reprocessing Look for competencies Certification within 2 years of hire Review all paperwork for reprocessing parameters Better that staff look like a deer in headlights with you, than with a TJC or CMS surveyor Implants Require a BI in each load Quarantine loads until BI results are known Early release of implant loads Can only be released by the surgeon A written policy is required In an emergency a Class 5 indicator can be used Sterilizer Qualification Testing Testing a sterilizer after certain events 3 consecutive cycles Events may adversely impact process Installation of new sterilizer Relocation of sterilizer Sterilizer malfunction Process failures Major repairs Gasket replacement Welding After annual boiler maintenance After a water main break In Summary……Why this topic? We “assume” others are doing the right thing Corners get cut Salary and titles do not equate with knowledge or expertise Common sense is not common TJC and CMS citations We are ultimately responsible Don’t Get Caught With Your Pants Down Class 6 process challenge packs Not a substitute for Class 5 integrating BIs No matter what the sales rep told the reprocessing administrator Sharing memos and recall notices Credentialing Inservice records