What Did We Gain from Cloning the CF Gene?
advertisement

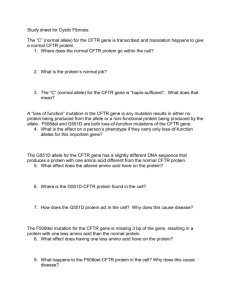
WHAT DID WE GAIN FROM CLONING THE CF GENE? Eitan Kerem Department of Pediatrics and CF Center, Hadassah University Hospital, Jerusalem, Israel Cystic fibrosis (CF) is caused by mutations in the CFTR gene which was cloned and sequenced twenty years ago. Today we know that the protein encoded by the gene is a chloride channel located in the apical membrane of exocrine epithelial cells. It has a molecular weight of ~170 kDa and comprises 1480 amino acids which are divided into five domains, i.e., two membrane-spanning domains (MSD1 and MSD2), each composed of six trans-membrane segments (TM1 to TM12) that form the channel, two nucleotide-binding domains (NBD1 and NBD2), capable of ATP hydrolysis, and a regulatory domain (R), which contains numerous phosphorylation sites. The protein structure indicates that CFTR belongs to the ATP-binding cassette transporter proteins. Phosphorylation of sites in the R domain by protein kinase A, regulated by cyclic adenosine monophosphate (cAMP), and the hydrolysis of ATP by NBDs, are essential for activating the chloride channel. This knowledge has not only enhanced our understanding of the mechanism of CF pathology, but has also provided explanations for phenotypic variations. Based on the known sequence of the gene, genetic testing has refined our ability to identify patients with CF and CF-related illnesses. Genetic mutations are grouped into 6 classes (I-VI) that can be directly related to the quantity of CFTR protein produced in the cells. The level of CFTR protein has a straight implication on the severity of the disease and may explain organ-specific sensitivity to the presence of normally functioning CFTR. Furthermore, seemingly organ-specific manifestations of CF, such as congenital bilateral absence of the vas deferens (CBVAD) can be accounted for by a mechanism based on the quantity of CFTR protein in cells. One of the earliest efforts, following the cloning of the gene, was invested in identifying the spectrum of disease-causing mutations. As of today over 1600 mutations are listed in the CFTR mutation database which in most countries is used as the basis for genetic testing. Increased usage of carrier screening and prenatal diagnosis has lead to a decline in the incidence of CF. Newborn screening (NBS) has been adopted in several countries leading to early diagnosis. Although the aim of NBS is to improve the life expectancy of patients with CF, it is probably associated with a decreased incidence in CF births as parents may opt not to have more children with CF. Many studies were already performed aiming to identify modifier genes for different phenotypes of CF using two main approaches. The first is analysis of candidate genes based on our current knowledge. By identifying modifiers of lung disease, already 40 candidate immune or inflammatory genes were studied for their effect on the severity of lung disease. Two genes, transforming growth factor b1 (TGFB1) a cytokine and mediator of fibrosis and mannose binding lectin 2 (MBL2), showed a possible effect on lung disease or infection prevalence. In recent years significant progress in technology and computational tools lead to techniques which enable association studies on the entire human genome by using a large number of patients. Recently, a new modifier gene for CF lung disease namely IFRD1was identified. This gene acts in a histone-deacetylase (HDAC)-dependent manner to mediate transcription of other genes and is expressed during terminal neutrophil differentiation. The knowledge gained so far has led to new therapeutic approaches that address key factors of cystic fibrosis pathophysiology. Past therapeutic successes were largely based on targeting the consequences of the cystic fibrosis trans-membrane regulator dysfunction, such as mucous retention, infection, and inflammation, but new therapies may be able to address the underlying abnormality rather than its downstream effects. The efficacy of these treatments still needs to be established, but early studies of several compounds look promising. In summary the cloning of the CFTR gene over 20 years ago provided us with tools for diagnosis of atypical and equivocal presentations, carrier testing for prenatal diagnosis and prevention of births of children with CF. This led to a decrease in the number of new cases in most countries. Understanding the molecular function of CFTR, and the mechanisms by which the different mutations cause CF led to the development of new therapies which are currently in different stages of development and in clinical trials.