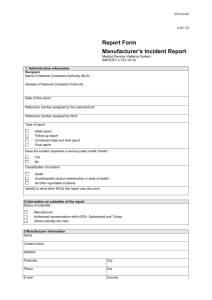
5.3. Acceptance of Medical Devices
advertisement

Medical Devices Policy Version Ver. 2.0 Replacing Medical Devices Policy Ver. 1 (2012) Name of responsible (ratifying) committee Medical Devices Management Committee (MDMC) Date ratified 16 October 2012 Document Manager (job title) Dr Matthew Wood (Chair of MDMC) Date issued 08 November 2012 Review date January 2015 (unless requirements change) Electronic location Management Policies Standing Financial Instructions Policy; Decontamination Policy; Procurement; record keeping; prescribing; maintenance; decontamination; storage; Key Words (to aid with searching) replacement; disposal; loan; single-use; adverse incident In the case of hard copies of this policy the content can only be assured to be accurate on the date of issue marked on the document. For assurance that the most up to date policy is being used, staff should refer to the version held on the intranet Related Procedural Documents Medical Devices Version 2.0 16/10/2012 Review date: January 2015 unless requirements change) Page 1 of 24 MEDICAL DEVICES POLICY CONTENTS 1. PURPOSE ................................................................................................................................... 3 2. SCOPE ........................................................................................................................................ 3 3. DEFINITIONS .............................................................................................................................. 3 4. DUTIES AND RESPONSIBILITIES ............................................................................................. 4 5. PROCESS ................................................................................................................................... 5 6. 7. 5.1. PROCUREMENT ...................................................................................................................... 5 5.2. RECORD-KEEPING .................................................................................................................. 6 5.3. ACCEPTANCE OF MEDICAL DEVICES ........................................................................................ 6 5.4. CLOCK SETTING ..................................................................................................................... 7 5.5. MONITORING, DEPLOYMENT AND CONTROL.............................................................................. 7 5.6. PROCEDURES ........................................................................................................................ 8 5.7. PRESCRIBING ......................................................................................................................... 8 5.8. MAINTENANCE AND REPAIR ..................................................................................................... 8 5.9. DECONTAMINATION ................................................................................................................. 9 5.10. STORAGE ........................................................................................................................... 9 5.11. REPLACEMENT PLANNING .................................................................................................. 10 5.12. DISPOSAL ......................................................................................................................... 10 5.13. LOAN EQUIPMENT ............................................................................................................. 10 5.14. SINGLE-USE EQUIPMENT ................................................................................................... 11 5.15. MANUFACTURING AND MODIFICATIONS OF MEDICAL DEVICES .............................................. 12 5.16. ADVERSE INCIDENTS AND MANAGEMENT OF SAFETY NOTICES ............................................. 12 TRAINING ................................................................................................................................. 13 6.1. RESPONSIBILITIES ................................................................................................................ 13 6.2. PROCESS ............................................................................................................................. 13 REFERENCES AND ASSOCIATED DOCUMENTATION ......................................................... 15 7.1. INTERNAL ............................................................................................................................. 15 7.2. EXTERNAL ............................................................................................................................ 15 7.3. CARE QUALITY COMMISSION’S SCHEDULE OF APPLICABLE PUBLICATIONS ............................... 15 APPENDIX A. SUBGROUPS ...................................................................................................... 20 APPENDIX B. PURCHASE OF A NEW MEDICAL DEVICE ........................................................ 21 APPENDIX C. GUIDANCE TO FOLLOW IN A MEDICAL DEVICE ADVERSE INCIDENT ......... 23 Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 2 of 24 MEDICAL DEVICES POLICY INTRODUCTION The term “medical device” covers a broad range of products, used every day throughout the Trust to support the diagnosis treatment and care of patients. These devices have a direct impact on the quality of care and can also be a source of risks to the patients and the staff. Regulations and safety of medical devices are guided by national legislations [6]. Care Quality Commission Outcome 11 [8] requires NHS Trusts to ensure that there is a system in place to manage risks associated with the use of medical devices. This policy, when read in conjunction with other relevant policies and procedures, ensures that whenever a medical device is used throughout the Portsmouth Hospitals NHS Trust (PHT), it is: Suitable and available for its intended purpose Properly understood by the user Used in accordance with the manufacturer’s instructions Maintained in a safe and reliable condition Disposed of safely and legally 1. PURPOSE This policy is written to enable the safe, efficient and effective deployment, monitoring and control of medical devices throughout the Trust. If in exceptional circumstances it is necessary to contravene any part of this policy, approval must be sought from the most senior manager on duty and the details recorded as an adverse incident. 2. SCOPE This policy applies to all permanent, locum, agency, bank and voluntary staff of Portsmouth Hospitals NHS Trust and the MDHU (Portsmouth) who have involvement in evaluation, selection, purchasing, commissioning, training, storage, maintenance, prescribing and disposal of medical devices owned wholly, in part, or loaned to the Trust, whilst acknowledging that for staff other than those directly employed by the Trust the appropriate line management or chain of command will be taken into account. ‘In the event of an infection outbreak, flu pandemic or major incident, the Trust recognises that it may not be possible to adhere to all aspects of this document. In such circumstances, staff should take advice from their manager and all possible action must be taken to maintain ongoing patient and staff safety. 3. DEFINITIONS Medical Device According to Medical Devices Directive [10], any instrument, apparatus, appliance, material or health care product (excluding drugs), used for a patient or client for the purpose of: Diagnosis, prevention, monitoring, treatment or alleviation of disease Diagnosis, monitoring, treatment or alleviation of or compensation for, an injury or Handicap Investigation, replacement or modification of the anatomy or of a physiological process Control of Conception Prescriber Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 3 of 24 MEDICAL DEVICES POLICY A person who decides which is an appropriate device for a given patient or client. Professional users Those appropriately trained and qualified to operate medical devices for the benefit of a patient. User Qualified person using devices as tools. End User A patient or client who uses a medical device unsupervised at home (e.g. wheelchair user). 4. DUTIES AND RESPONSIBILITIES Medical Devices Management Committee (MDMC) is responsible for monitoring the implementation of this policy throughout the organisation. This will be achieved through monitoring and ensuring adherence to this policy by the Clinical Service Centres (CSC). MDMC will have responsibility for managing all pieces of medical devices owned by or used within the Trust and for monitoring training implementation to ensure the safety of staff, visitors and others. Subgroups will be chaired by clinicians and be responsible for ensuring good governance in relation to the management of disposable and non-disposable medical devices governed by their subgroup. This will be achieved through: Safe use of devices by promoting responsibility of the CSCs and individual clinicians ensuring users are appropriately and adequately trained in the use of medical devices Record keeping of: lifecycle history, maintenance and repair, utilisation, training of users Responding to alerts from various sources: internal adverse incident reports; MHRA alerts and manufacturer recalls/alerts. Analysis of technical and clinical evaluations of medical devices Ensuring appropriate procurement of medical devices The Chair has responsibility for ensuring the appropriate membership and meetings of the subgroup and providing leadership to the subgroup. They will ensure minutes of meetings are produced and kept. The Chair of the subgroup will: Advise the CSCs and the MDMC on the priorities for the annual replacement of existing equipment to assist the CSCs in developing their annual business plans (see flow chart for purchase of replacement medical devices). Advise the MDMC and the Trust Planning Committee (TPC) or equivalent on whether new medical devices should be introduced into clinical practice in the Trust Be standing members of MDMC and will be expected to attend meetings as required or to ensure appropriate deputies attend in their place. The Chairs will report to the Chair of MDMC and will on occasion be asked to deputise for them. The structure of subgroups can be found in APPENDIX A. Clinical Service Centre Management Teams, Department and Line Managers are responsible for ensuring this policy is implemented in their areas. They must also ensure necessary resources are available to enable staff to attend appropriate training. Professional users are those appropriately trained and qualified to operate medical devices for the benefit of a patient. They have a duty of care to the patient and others to ensure they understand the Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 4 of 24 MEDICAL DEVICES POLICY purpose, operation, and limitations of devices together with measures to minimise risks. Those who are competent to decide on the appropriateness of a device for use with a specific patient, may act as prescribers. Clinical Engineering Department (ClinEng) Is responsible for providing an in-house maintenance and repair facility to the Trust for Medical devices agreed at purchase. They are responsible for accepting medical devices to the Trust and disposing of equipment at the end of their life cycle. Acceptance and disposal is in line with recommendations made in DB2006 (05) [7]. Is in charge of the medical devices management database and central inventory. Provides assistance and advice to all Trust members on procuring, selecting devices, selecting maintenance, co-ordinating training and investigating adverse incidents. Procurement Department will lead tender / quotation exercises and place purchase order(s) after Medical Equipment forms and pre purchase questionnaires have been approved. All staff involved directly or indirectly in healthcare are responsible for following the procedures laid down in this policy and for ensuring that they have the skills and knowledge required to work safely with any medical device. 5. PROCESS 5.1. Procurement A flowchart that details the steps to be taken during a procurement procedure can be found in APPENDIX A. This flowchart is a guidance tool and must be used in conjunction with the Trust’s Standing Financial Instructions Policy. Medical Equipment Procurement (MEP) form and relevant documents can be found on the MDMC page on the Trust’s Intranet. Any specific standards or guidance that needs to be met will be considered prior to writing suitable specifications. Following the instructions and guidance will ensure that these issues will be appropriately considered: Life cycle / replacement Fitness for intended applications Guarantee/Warranty Safety Reliability Service Support Maintenance Requirements Technical Support Training (including on site training if appropriate) Decontamination Standardisation Once the need for the device and the source of funding are identified, a risk assessment procedure and full consideration of relevant standards and guidelines will results in technical specifications for the device. The medical device subgroup determines if the device should be considered as a Trust Medical Device Standard (MDS). If identified as an MDS it will generally remain current for the term negotiated by the Procurement Department with the supplier, typically 5 years. This period may be extended if the device remains suitable beyond the end of the initial contract. Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 5 of 24 MEDICAL DEVICES POLICY Prior to any purchase, a multidisciplinary team will evaluate the available medical devices that meet the clinical need. The relevant Subgroup of MDMC is in charge to design and carry out the technical and clinical appraisals. Ideally a minimum of three alternative suppliers should be considered to ensure compliance with EU procurement legislation and the Trust’s Standing Financial Instructions. Completed NHS Pre-Purchase Questionnaire form (PPQ) will be obtained from each candidate supplier and reviewed by ClinEng to verify compliance with national standards. Using a scoring system, devices will be evaluated against the following criteria: Compliance with national legislation Minimisation of all risks Ability to provide essential clinical function Reliability and availability of technical and user support The subgroup will report the results together with full lifetime costs to MDMC who will inform the relevant CSC for items costing under £25000 or the Trust’s Planning Committee (TPC) or equivalent for items costing over £25000. Maintenance arrangements must also be considered at this stage. Next, the signed ME form will be sent to ClinEng who will pass the form to the Procurement team for placing the order. Further guidance and advice can be sought from MDMC, DB2006 (05) [7] and Trust’s Standing Financial Instructions. A flowchart in PURCHASE OF A NEW MEDICAL DEVICE will be used to assist with the procurement process. 5.2. Record-keeping ClinEng keep a record of all medical devices in the Trust, which provides evidence of: A unique identifier for the device, where appropriate A full history, including date of purchase and where appropriate when it was put into use, deployed or installed Any specific legal requirements and whether these have been met Proper installation Where it was deployed and utilisation Scheduled maintenance Maintenance and repairs The end-of-life date. The records will also show that users: Know how to use the device safely Can carry out routine checks and maintenance Have been trained and had relevant refresher training. 5.3. Acceptance of Medical Devices When a new medical device is delivered to ClinEng, a series of tests will be carried out to ensure safety and verify the performance of the device, before it is deployed in service. Delivery checks will include: Checking that the correct product, complete with usage and maintenance information and any relevant accessories, has been supplied Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 6 of 24 MEDICAL DEVICES POLICY Ensuring that devices have been delivered in good condition and, where relevant, in good working order. The details of the tests can be found in DB2006 (05) [7]. Assembly of the device and performance checks will be performed in line with manufacturer’s recommendations to ensure the accuracy prior to clinical use. The manufacturer’s user instructions will be supplied at purchase and delivered with the equipment. A signature will be obtained from the recipient user. A maintenance manual must be requested if not already provided, logged and filed. According to DB2006 (05) [7], some devices must be risk assessed before first use. See the table below for details: Category Examples Medical devices manufactured outside the scope of the Medical Devices Regulations. Purchased by an individual outside EU. In-house manufacture. Bought second-hand. Lent by another responsible organization. Equipment re-issued to second or subsequent users. Equipment which has, or may have, been used before. Devices within scope of Medical Devices Regulations, but not CE marked. Custom-made for a named patient. Under clinical investigation. The Medical Device Training Team will be informed of all new equipment purchases and they will decide the level of training required for staff, organise the training and record the user training. 5.4. Clock Setting The clock on all medical devices must be set to the correct time by the user. In some equipment the clock is not user settable and will be left at Greenwich Mean Time (GMT) and these devices will carry a label to that effect. 5.5. Monitoring, Deployment and Control Clinical Engineering Department (ClinEng) must ensure an inventory of all medical device is maintained. This will enable the organisation to take appropriate action following manufacturer’s recall or the issue of hazard warning notice. The inventory will ensure that medical devices are examined annually for electrical safety, calibrated and/or serviced as necessary and that scheduled maintenance takes place. All inventories must include the following: Order Number Date of purchase Unique asset number Supplier Manufacturer, Model, Manufacturer’s serial number, serial numbers of components modules Nominated team of ClinEng in charge of the device Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 7 of 24 MEDICAL DEVICES POLICY Results of acceptance test Warrant details Identified Maintenance/repair Organisation Date of first service and subsequent service dates (to include calibration) Information about/instructions relating to application e.g. safe working load, cleaning and decontamination etc. 5.6. Procedures ClinEng holds an inventory and service log of all diagnostic and therapeutic equipment used within the organization. Medical Devices Training Team (MDTT) will use separate matrices of “equipment vs. members of staff” for every ward and department within the Trust. Twice a month ClinEng will provide reports of newly purchased equipment to MDTT who will add them to the relevant matrices and ensure that appropriate training is arranged in advance. This will be supported and managed by MDMC to ensure that information is cascaded to ClinEng and MDTT to facilitate training at the earliest point. Training can be arranged in clinical areas or in the Training and Education Department. This can be facilitated in a number of ways and can include workshops, one to one training; ad hoc training can also be arranged. Once the training is provided, records of this training will be uploaded onto ESR. A completed competency statement will form evidence of competence. 5.7. Prescribing The prescription of medical devices must be made by healthcare professionals who are suitably qualified and experienced to understand the function of the device and its application. Those responsible for selection need to have been trained and need ready access to information about the device, including: The manufacturer’s description of the intended user, usage and the instructions for use Safety issues and any limitations on use Pre-use set up or testing requirements Maintenance and cleaning or decontamination requirements. Devices are chosen to best meet the requirements of the intended medical procedure or needs of the end user. Any short-term loan/issue of a device should be considered to provide benefit to end users until the most appropriate device is available. The needs of the carer should be taken into account where appropriate. In some instances devices remain with patients for periods extending beyond original episode (e.g. patient taking a device from acute to secondary care or patient with an implanted device) crossboundary prescribing may exist. In such cases the prescribing professional must clarify where professional and legal responsibility for prescription lies and where continuing responsibility lies to monitor the device and the condition of the end-user. 5.8. Maintenance and Repair All medical devices require routine maintenance and/or calibration at a frequency recommended by the manufacturer whether it be checks by the user, maintenance by ClinEng or maintenance by the manufacturer. It is a requirement of NHSLA standard 5 – criterion 4 [9] that the Trust has an approved documented process for managing the maintenance of reusable diagnostic and therapeutic equipment. Guidance is taken from DB2006 (05) [7]. Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 8 of 24 MEDICAL DEVICES POLICY Maintenance may be provided by the manufacturer or supplier, in-house organisation, third party provider or partnership arrangements between any of these. Accurate detailed records of all maintenance and repair work must be provided by the maintenance provider and kept by the ClinEng on the equipment management database with copies readily available to user manager if required. Labels are affixed to devices to show when next maintenance is due. The equipment management database will also hold details on the servicer, service schedule and contract reference. It is the responsibility of each individual to ensure the equipment they use is in a serviceable state prior to clinical use. Serviceable state would mean there is no visible damage to the equipment, the equipment passes pre use checks, the equipment has not been reported as faulty and that the service due date hasn’t expired. All reusable medical devices must be scheduled for Planned Safety and Performance Testing (PSPT). Medical devices are retrieved from their location by ClinEng with the agreement of the user and returned to service after the completion of the PSPT. The level and frequency of maintenance is decided based on manufacturer’s recommendation but may be adjusted to take account of local factors and experience. All faulty medical devices must be removed from service immediately. For all faults occurring on medical devices ClinEng should be contacted by email or on the phone: 02392286000 (7700) 6101. ClinEng will then initiate the process to resolve the problem depending on how the maintenance support is provided i.e. in-house or by external contract. All medical devices must be decontaminated by the user prior to release for maintenance or repair. Any spare parts used will be supplied by the manufacturer or to the same specification. Pre-used parts will only be used under exceptional circumstances for example to replace a faulty part that is no longer available from the manufacturer. A record of spare parts replaced during maintenance or repair will be kept by ClinEng with traceability of critical parts back to the manufacturer. 5.9. Decontamination Most medical devices can become contaminated and hence present a risk to patients, users and support staff. Contamination may be chemical, biological, or radiological in nature. Specific guidance on decontamination can be found in the Trust Decontamination Policy. However the following basic principles must be followed: All medical devices must be free from contamination and if necessary sterile prior to use. A medical device must be decontaminated as soon as practicable after use. If it is not possible to decontaminate a device it must be isolated, e.g. bagged and labeled, with the nature of contamination and date. Medical devices must be decontaminated prior to service. Medical devices must be decontaminated before loan to other organisations or end users. Decontamination must be performed according to procedures specified in Trust policy. Manufacturers are required to provide information regarding suitable methods of decontamination. 5.10. Storage Poor storage conditions prior to deployment can adversely affect medical devices. Ward and Department managers who have responsibility for use of medical devices must operate systems to avoid the following: Dirty or wet storage conditions Inappropriate temperature or humidity Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 9 of 24 MEDICAL DEVICES POLICY Physical damage due to poor stacking Mix of contaminated and decontaminated items due to inadequate space or zone demarcation. Failure to maintain charge and capacity of device batteries The Medical Equipment Library (MEL) provides a central repository of widely used medical devices. This will be the preferred storage location for many common devices. The Supply Chain team within the Procurement Department is responsible for ensuring the majority of disposable or single use medical devices are: Available when required Stored with appropriate stock rotation Use by and sterilisation dates are not exceeded. Storage records will be maintained and periodic audit of the above factors will be undertaken. Stock takes of all library equipment, verifying locations within the hospital, should be performed on a quarterly basis. 5.11. Replacement Planning A device will not be considered serviceable if any of the following criteria apply: Worn / damaged beyond economical repair Unreliable (poor service history) Clinically or technically obsolete Spare parts no longer available If because of design, wear and tear or damage the equipment cannot be cleaned effectively prior to disinfection / sterilisation Subject to MHRA Issued Medical Device Alert/ Safety Notice/Manufacturer recommended removal from use / service It is the responsibility of the CSCs to secure funds for medical devices either through revenue monies, capital, Trust funds or charitable funds. The Trust Planning Committee (TPC) or equivalent are responsible for monitoring and authorising capital bid purchases. MDMC is responsible for monitoring and authorising all medical device purchases although responsibility for routine purchase is delegated to the ClinEng. The flowchart in APPENDIX B, is an assistive tool for this procedure. 5.12. Disposal The reuse, resale and disposal of medical devices is described DB2006 (05) [7]. Prior to disposal the device will be removed from any maintenance schedule and be marked as disposed on the equipment management database. 5.13. Loan Equipment 5.13.1. Medical Devices loaned to the Trust for Trials, Evaluation or Clinical Use Prior to any agreements/arrangements for delivery of such equipment to the Trust, members of staff must liaise with the general manager of the relevant CSC who will contact Solent Supplies Team for the advice on the appropriate procedure (Solent Supplies Suppliers Representative Policy). Solent Supplies Team will then contact the MDMC Subgroup chair. All such equipment is subject to acceptance checks and procedures as Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 10 of 24 MEDICAL DEVICES POLICY described in section 5.3 above. Appropriate indemnity forms and delivery notes must be completed prior to clinical use. All users must be given instruction in the safe use of the equipment prior to the equipment being put into service. All guidelines relating to the cleaning and decontamination of medical devices must be applied to any equipment on loan to the Trust. Full certification must be provided confirming that the equipment is fully traceable and has been effectively decontaminated prior to delivery. Equipment and devices (including surgical instruments) loaned to the Trust must be accompanied by appropriate reprocessing instructions (if relevant) and a comprehensive inventory detailing all contents. All surgical instruments loaned to the Trust will be processed in HSDU prior to and following use. Loan equipment must be collected promptly when no longer required or when the date on the indemnity expires. 5.13.2. Medical Devices Loaned to Other (Third Party) Organisations Medical Devices (including surgical Instruments) that are the property of the Trust must not be loaned to any third party unless the borrower can guarantee full systems of traceability, safe transport, competency of users and effective decontamination. The duration of the loan can be realistically forecast. This process will be managed by ClinEng under MDMC’s guidance. 5.14. Single-use Equipment Some medical devices are designated by the manufacturer as “single use” and are identified with the symbol shown above either on the device or the packaging. Devices with this designation may be either, unsuitable for sterilisation or decontamination due to their materials or construction or be insufficiently robust to withstand more than one use. Governance arrangements of these devices will come under the relevant MDMC Subgroup (APPENDIX A) Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 11 of 24 MEDICAL DEVICES POLICY Under the Medical Device Directive (93/42/EEC) [10], if a device has been reprocessed for reuse, it is no longer the original manufacturer but the reprocessor who must ensure that they comply with the requirements of the Medical Device Directive. When reprocessing single use devices, whether for in-house reuse or for reprocessing to supply to others, if the device causes damage or injury during reuse, the reprocessor and the user may become personally liable. The MHRA published advice on this matter in DB 2006(04). In almost all circumstances the MHRA advice is pertinent to medical device use within PHT. As a default requirement, no medical device designated as single use by the manufacturer shall be reused or reprocessed. In exceptional circumstances, where there could be higher probability of other risks, the Trust may authorise re-use of single use devices after a full risk assessment by MDMC. 5.15. Manufacturing and Modifications of Medical Devices PHT policy is not to modify medical devices. All plans to manufacture or modify medical devices locally within the Trust must be reported to the MDMC via the appropriate subgroup. Whilst the Medical Devices Regulations [6] do not apply to devices manufactured “in-house” provided they are used only within the same legal entity, the standards of manufacture must be equivalent. Adequate documentation must be produced for all devices manufactured in-house and of modifications to commercial devices. The documentation must include details of risk assessment in accordance with BS EN 14971 [11]. In-house manufactured devices must comply with the principles of this policy. 5.16. Adverse Incidents and Management of Safety Notices An adverse incident is any event or circumstances arising during NHS care that could have or did lead to unintended or unexpected harm, loss or damage. All adverse incidents involving medical devices must be reported according to the Trust Adverse Incident Reporting Policy. A flowchart providing guidance is shown in APPENDIX A. The Risk Management Department (RMD) will notify the MHRA via the Medical Devices Liaison Officer (MDLO) if appropriate. According to Central Alert System (CAS) Policy, head of Risk Management and Legal Services is the Trust’s nominated CAS officer. Users are requested not to contact MHRA direct except in the case of incidents where there is extreme and immediate danger of reoccurrence. Devices involved in an adverse incident together with other material evidence (e.g. packaging of single use device) must be clearly labeled and where practicable kept in quarantine until the incident investigation is complete. If this is not practical, the identification and state of the device at the time of the incident must be recorded. Any clearly dangerous device must be effectively disabled to prevent it being used. The RMD will send copies of adverse incidents involving medical devices to the relevant Subgroup. Adverse incidents will be considered at each Subgroup meeting. If the RMD has considered it necessary to report to MHRA the subgroup will be required to communicate with RMD all measures taken to prevent reoccurrence. Receipt and distribution and response to MHRA and manufacturer safety notices on medical devices is managed by the MDLO. Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 12 of 24 MEDICAL DEVICES POLICY 6. TRAINING Training is a key element in medical device safety. It is a requirement of NHSLA standard 5 – criterion 5 [9] that the Trust has an approved document which sets out the training requirements of all permanent staff in relation to the use of diagnostic and therapeutic equipment. 6.1. Responsibilities MDMC has the responsibility to ensure that the training of medical devices is provided to all the users of medical devices and the service personnel. They will promote the safe and appropriate use of medical devices available in the Trust and ensure members of staff have access to training which provides them with the necessary knowledge and skills to operate medical devices they may be required to use. Line Managers at all levels have a duty to ensure that their staff required to use medical devices are competent and supporting records exist, e.g. training and assessment. They must also support the medical device training program and allow staff time for adequate and appropriate training. Medical Device Training Team (MDTT), Specialist Technical/ Clinical Advisers & Practice Educators act as a source of expert information and, where appropriate, training for other staff. Such advisers must ensure that their own competence is continually updated, verified and recorded. Medical Device Training Section can be contacted via telephone extension (7700) 3786 or email. Users Department managers are responsible for identifying training needs within their areas of responsibility and organising appropriate training. Healthcare professionals working for the organisation, as employees or contractors, have a professional duty to ensure their own skills and training are appropriate and remain up to date. End User The Prescriber is responsible for ensuring that the End Users receives training for the prescribed device and is competent in its use prior to release. Technical Staff The ClinEng Section Head is responsible for identifying training needs of technical staff maintaining and repairing medical devices and for arranging appropriate training as described in local quality procedures. 6.2. Process 6.2.1. Medical Device Training information is included in mandatory corporate induction; this provides all new staff with awareness of the existence and role of the MDTT. 6.2.2. Permanent staff are identified through the Electronic Staff Record (ESR). 6.2.3. These self-assessment documents and associated questions are available from the MDTT or can be accessed on the Intranet. They are validated every two years or when new equipment is added to the inventory. The statements are completed by staff and returned to the MDTT. This information is then recorded on ESR and staff will receive automatic notification on ESR before their competency expires. The competency statement identifies whether the user is currently competent, requires training or does not use any items of the listed equipment. 6.2.4. Staff who require training complete the relevant box on the form giving details of their availability for training in the next month. If the member of staff does not give suitable dates for training or does not attend, they, and their ward manager, receive a reminder email and have two weeks to respond. This ensures that staff absence does not compromise receipt Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 13 of 24 MEDICAL DEVICES POLICY of required training. If there is no response after this period it is assumed that training is no longer required and their form will be updated to indicate that they no longer require training. 6.2.5. During the yearly Appraisal and Personal Development Review (APDR) process, Line Managers go through the training records of each permanent member of staff to verify that their training is up-to-date on all the Medical Devices they use as part of their role. 6.2.6. Training is delivered in a variety of ways: ward based; attendance at specialty training days; ad hoc and on a one to one basis. This ensures all staff can receive appropriate training. In addition, E-learning refresher courses and user instruction manuals for Medical Devices are available to all members of staff on Medical Devices Training Intranet page. This ensures all staff can receive appropriate training. 6.2.7. Staff verification of competence for each item of equipment are recorded on ESR. Line Managers can access this information in ESR under Manager Self-service, Manage Staff Careers heading, the Competence section. This allows the Line Managers to ensure that any member of staff who does not complete and return the Medical Devices Group Competency Statement form can be followed up. 6.2.8. Once training is completed in a Department, information on staff competence is sent to the Department Managers and Heads of Nursing. 6.2.9. The Learning and Development Team provide a monthly heat map from ESR to each CSC, to enable monitoring of competence. ??? 6.2.10. Compliance is further monitored through the CSC performance reviews with the Executive Team. 6.2.11. Once trained, the member of staff is deemed competent for the following two years, when a further self-assessment Medical Devices Group Competency Statement form must be completed. Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 14 of 24 MEDICAL DEVICES POLICY 7. REFERENCES AND ASSOCIATED DOCUMENTATION 7.1. Internal [1]. Policy for the Management of Adverse Incidents and Near Misses [2]. Policy for the Management of Serious Incidents Requiring Investigation [3]. Central Alert System Policy [4]. Decontamination Policy [5]. Standing Financial Instructions 7.2. External [6]. Medical Device Regulations, 2002 [7]. Device Bulletin DB2006 (05), Managing Medical Devices - Guidance for healthcare and social services organisations: MHRA, Nov 2006. www.mhra.gov.uk/Publications [8]. The Essential Standards of Quality and Safety: Care Quality Commission, 2009 [9]. NHSLA Risk Management Standards 2012-13 Version 1. NHS Litigation Authority (NHSLA), January 2012 [10]. Medical Devices Directive: The Council of the European Communities, Directive 93/42/EEC, 1993 [11]. The Application of Risk Management to Medical Devices: EN 14971:2009 Standard, British Standards Institution [12]. The Electricity at Work Regulations. Statutory Instrument 1989 No. 635. ISBN 011096635X. http://www.opsi.gov.uk/si/si1989/Uksi_19890635_en_1.htm [13]. Health and Safety at Work etc. Act 1974. London: HMSO, 1974. ISBN 0105437743 7.3. Care Quality Commission’s Schedule of Applicable Publications [14]. MHRA DB2008(03) Guidance on the safe use of lasers, IPL systems and LEDs [15]. MHRA DB 2006 (4) Single-use Medical Devices: Implications and Consequences of Reuse (MHRA, 2006) [16]. MHRA DB 2006(5) Managing Medical Devices: Guidance for health care and social care organisations (MHRA, 2006) [17]. Safety alerts, rapid response alerts, guidance and directives relating to equipment published by expert and professional bodies including: National Institute of Clinical Excellence National Patient Safety Agency Medicines and Healthcare products Regulatory Agency Royal Pharmaceutical Society of Great Britain DH Product manufacturers [18]. DH IRMER Guidance and Good Practice Notes Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 15 of 24 MEDICAL DEVICES POLICY [19]. Mental Health Act 1983 and Mental Health Act Code of Practice (DH, 2008 relating to seclusion facilities) Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 16 of 24 MEDICAL DEVICES POLICY EQUALITY IMPACT STATEMENT Portsmouth Hospitals NHS Trust is committed to ensuring that, as far as is reasonably practicable, the way we provide services to the public and the way we treat our staff reflects their individual needs and does not discriminate against individuals or groups on any grounds. This policy has been assessed accordingly. Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 17 of 24 MONITORING COMPLIANCE As a minimum the following elements will be monitored to demonstrate compliance. Medical Devices Version 2.0 16/10/2012 Review date: January 2015 unless requirements change) Page 18 of 24 MEDICAL DEVICES POLICY Minimum requirement to Lead be monitored Process for ensuring Head of that all reusable medical Clinical devices and equipment Engineering are maintained: 95% maintained within designated timescales Process for ensuring Head of that all reusable medical Clinical devices and equipment Engineering are repaired: 95% repaired within designated timescales Process for identifying Medical which permanent staff Devices are authorized to use the Training equipment identified on Team the inventory: 95% of staff identified Process for determining Medical the training required to Devices use the equipment Training identified on the Team inventory and the frequency of updates required: 100% Process for ensuring Medical that the identified Devices training needs of all Training permanent staff are met: Medical Devices Version 2. Team 16 October 2012 85% Review date: January 2015 unless requirements change) Tool Frequency of Report Annually Reporting arrangements Policy audit report to: Medical Devices Management Committee Lead(s) for acting on recommendations Chair of Medical Devices Management Committee Audit of Clinical Engineering Dashboard Annually Policy audit report to: Medical Devices Management Committee Chair of Medical Devices Management Committee Medical Devices Training Database Annually Policy audit report to: Medical Devices Management Committee Chair of Medical Devices Management Committee Medical Devices Training Database Annually Policy audit report to: Medical Devices Management Committee Chair of Medical Devices Management Committee ESR Annually Policy audit report to: Medical Devices Management Committee Page 19 of 24 Chair of Medical Devices Management Committee Audit of Clinical Engineering Dashboard APPENDIX A. SUBGROUPS There are 5 subgroups of the Medical Devices Management Committee (MDMC): General Medical Technology Patient Handling and Mobility Specialist Surgical Devices Imaging and Radiotherapy Pathology Subgroups. Pathology Autoclaves (Laboratory) ACT monitors Blood gas, Haemoglobin and other Point Of Care Testing analysers Blood glucose & HbA1C measuring devices Cholesterol test kits Fridge & Freezers (non domestic) Fume cabinets Microscopes (Laboratory) Other IVDs Pharmacy devices Pregnancy test kits Specimen collection receptacles, syringes, swabs Urine test strips Imaging & Radiotherapy CT scanners Gamma Cameras Linacs & RT devices MR scanners Nuclear medicine equipment Radiation monitors Ultrasound imaging systems X ray imaging systems X ray therapy systems Specialist Surgical Autoclaves and other HSDU Cryosurgical Equipment Cardiac Pacemakers (implantable) Dental equipment and materials Implants e.g. orthopaedic prostheses Incontinence aids Insulin injectors Lasers Operating and diagnostic microscopes Operating tables Ophthalmology devices Powered implants e.g. pacemakers Plaster saws Rigid Endoscopes & video systems Surgical and dental instruments Surgical diathermy Patient handling & mobility Bathing equipment Chiropody and podiatry equip Commodes Clinical chairs Dental chairs Medical Devices Version 2.0 Hospital beds & mattresses Patient hoists Pat slides Prescribable footwear Pressure relief equipment Prostheses Stretchers and trolleys Walking aids Wheelchairs General Medical Technology Anaesthesia machines Audiometers Blood warmers Continuous passive motion devices (CPM) Defibrillators Dialysis equipment Domiciliary O2 therapy equip Drip stands ECT devices EEG EMG analysis systems Flexible Endoscopes & video systems Endoscope washers Electrocardiographs Humidifiers Respiratory Infusion control devices Laryngoscopes etc Illuminating Light Sources Light therapy sources Medical gas equip. regulators suction controllers cylinder holders etc Nebuliser compressors Nebuliser ultrasonic Patient monitoring NIBP, SpO2 ECG etc Patient warming / cooling devices Peak flow meters Physio. electro-therapy Pulse oximeters Respiratory lung function analysis Resp. support devices, domiciliary vents. Resuscitation equipment Sphygmomanometers Stress test systems Suction equipment Thermometers Ultrasound Doppler Ventilators ICU & Anaesthesia Weighing scales 16/10/2012 Review date: January 2015 unless requirements change) Page 20 of 24 MEDICAL DEVICES POLICY APPENDIX B. PURCHASE OF A NEW MEDICAL DEVICE On the following Page Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 21 of 24 MEDICAL DEVICES POLICY Identify source of funding in principle Seek advice from chair of Subgroup Yes New Technology? Prepare proposal for evaluation Proposal approved by subgroup ? Yes No No Clinical and technical evaluation – report result to Subgroup Prepare proposal for purchase Proposal for purchase approved by subgroup? No Yes No < £25000? Submit to TPC or equivalent for approval Yes Send MEP form to Clinical Engineering Purchase by Procurement Team Delivery to MED Training of users Commissioning the equipment Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 22 of 24 MEDICAL DEVICES POLICY APPENDIX C. GUIDANCE TO FOLLOW IN A MEDICAL DEVICE ADVERSE INCIDENT On the following Page Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 23 of 24 MEDICAL DEVICES POLICY Incident Occurs PATIENT HARM? YES NO Respond to patient and carer need Alert all relevant clinical staff Mark all devices clearly as potentially faulty Quarantine device and accessories (e.g. infusion pump AND disposable item including packaging) Do not send to supplier Identify “lead” staff member to act as contact/liaison Grade incident and follow procedure as detailed in Adverse Event Reporting policy. Complete Adverse Incident Report form In case of extreme and immediate danger of reoccurrence, contact MRHA directly via link ‘report incidents’ http://www.mhra.gov.uk/Safetyinformation/Reportingsafety problems/Devices/index.htm Advise Trust Liaison Officer of incident via email sheena.king@portho sp.nhs.uk Contact Clinical Engineering or other specialist technical department for advice Advise other areas/users of potential problem if appropriate. Notify Manufacturer or Supplier Staff “Lead” review incident with Liaison Officer re further action/roles i.e. incident investigation, contact with MRHA, Clinical Engineering, Manufacturer etc. Staff “Lead” to feedback results of investigation/incident to staff (including Risk Management) highlighting any lessons learned Report results of investigation/incident to Chair of appropriate Medical Device Subgroup Medical Devices Version 2. 16 October 2012 Review date: January 2015 unless requirements change) Page 24 of 24