Metachromatic Leukodystrophy: Molecular Diagnostic Service
advertisement
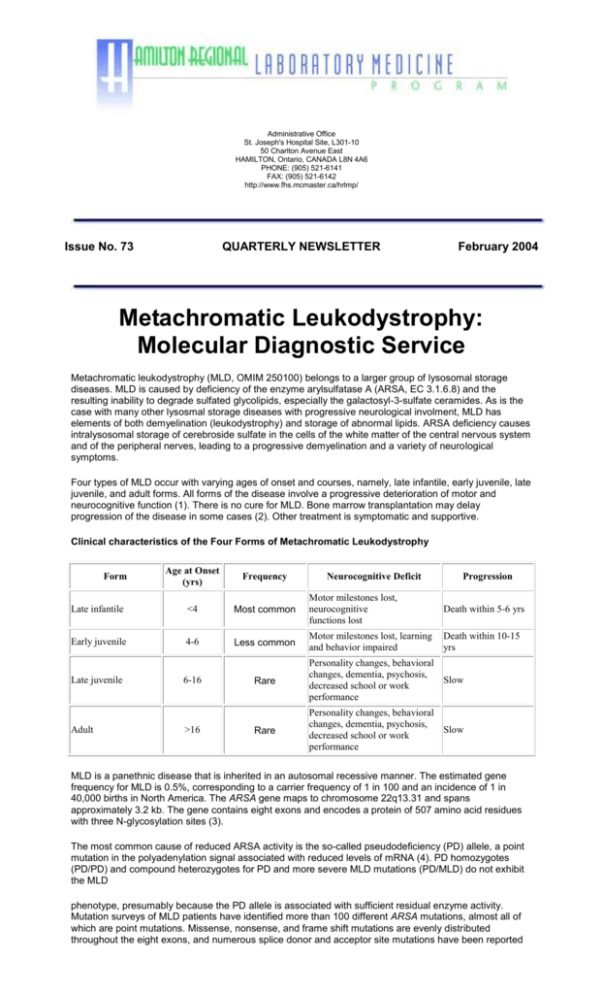
Administrative Office St. Joseph's Hospital Site, L301-10 50 Charlton Avenue East HAMILTON, Ontario, CANADA L8N 4A6 PHONE: (905) 521-6141 FAX: (905) 521-6142 http://www.fhs.mcmaster.ca/hrlmp/ Issue No. 73 QUARTERLY NEWSLETTER February 2004 Metachromatic Leukodystrophy: Molecular Diagnostic Service Metachromatic leukodystrophy (MLD, OMIM 250100) belongs to a larger group of lysosomal storage diseases. MLD is caused by deficiency of the enzyme arylsulfatase A (ARSA, EC 3.1.6.8) and the resulting inability to degrade sulfated glycolipids, especially the galactosyl-3-sulfate ceramides. As is the case with many other lysosmal storage diseases with progressive neurological involment, MLD has elements of both demyelination (leukodystrophy) and storage of abnormal lipids. ARSA deficiency causes intralysosomal storage of cerebroside sulfate in the cells of the white matter of the central nervous system and of the peripheral nerves, leading to a progressive demyelination and a variety of neurological symptoms. Four types of MLD occur with varying ages of onset and courses, namely, late infantile, early juvenile, late juvenile, and adult forms. All forms of the disease involve a progressive deterioration of motor and neurocognitive function (1). There is no cure for MLD. Bone marrow transplantation may delay progression of the disease in some cases (2). Other treatment is symptomatic and supportive. Clinical characteristics of the Four Forms of Metachromatic Leukodystrophy Age at Onset (yrs) Frequency Late infantile <4 Most common Motor milestones lost, neurocognitive functions lost Death within 5-6 yrs Early juvenile 4-6 Less common Motor milestones lost, learning and behavior impaired Death within 10-15 yrs Form Late juvenile Adult 6-16 >16 Neurocognitive Deficit Progression Rare Personality changes, behavioral changes, dementia, psychosis, Slow decreased school or work performance Rare Personality changes, behavioral changes, dementia, psychosis, Slow decreased school or work performance MLD is a panethnic disease that is inherited in an autosomal recessive manner. The estimated gene frequency for MLD is 0.5%, corresponding to a carrier frequency of 1 in 100 and an incidence of 1 in 40,000 births in North America. The ARSA gene maps to chromosome 22q13.31 and spans approximately 3.2 kb. The gene contains eight exons and encodes a protein of 507 amino acid residues with three N-glycosylation sites (3). The most common cause of reduced ARSA activity is the so-called pseudodeficiency (PD) allele, a point mutation in the polyadenylation signal associated with reduced levels of mRNA (4). PD homozygotes (PD/PD) and compound heterozygotes for PD and more severe MLD mutations (PD/MLD) do not exhibit the MLD phenotype, presumably because the PD allele is associated with sufficient residual enzyme activity. Mutation surveys of MLD patients have identified more than 100 different ARSA mutations, almost all of which are point mutations. Missense, nonsense, and frame shift mutations are evenly distributed throughout the eight exons, and numerous splice donor and acceptor site mutations have been reported (5,6). Two mutations, c.459+1G>A and c.1277C>T (p.Pro426Leu), account for almost one-half of all MLD alleles in patient surveys (7), with the remaining alleles being rare or private. Given the broad spectrum of ARSA gene mutations associated with MLD, it is important that molecular diagnostic strategies be capable of detecting common alleles as well as rare or private alleles. We have developed rapid and reliable allele-specific assays based on the amplification refractory mutation system (ARMS) (8) to detect the three most common MLD alleles [c.459+1G>A, c.536T>G (p.Ile179Ser), c.1277C>T (p.Pro426Leu)], as well as the pseudodeficiency allele (c.1620A>G). This is followed by comprehensive nucleotide sequence analysis of the entire ARSA gene exons and intron/exon boundaries (9). Lastly, Southern blot analysis is used to identify rare cases of MLD involving deletion of the ARSA gene (10). Since 1998, the Molecular Diagnostic Genetics laboratory at the McMaster site has provided DNA diagnosis for MLD as Provincial service. The above diagnostic protocol has been used to identify ARSA gene mutations in more than 50 patients with MLD, with a mutation detection sensitivity of >95%. In our patient sample, the C.459+1G>A and c.1277C>T (p.Pro426Leu) mutations accounted for almost 40% of the mutant alleles. The remaining alleles were extremely rare, and included nine point mutations and a complete ARSA gene deletion that had previously not been reported in the literature (9,10). This information has been invaluable for identifying couples at risk for having children with MLD, and for providing prenatal diagnosis for at-risk pregnancies. To date, we have provided prenatal diagnosis for eight such pregnancies. References 1) von Figura K, Gieselmann V, Jaeken J. Metachromatic leukodystrophy. In: Scriver CR, Beaudet AL, Valle D, Sly WS, Childs B, Kinzler KW, Vogelstein B, eds. The metabolic and molecular bases of inherited diseases. 8th ed. (2001) New York: McGraw-Hill, 3695-3724. 2) Koc ON, Day J, Nieder M, Gerson SL, Lazarus HM, Krivit W (2002) Allogeneic mesenchymal stem cell infusion for treatment of metachromatic leukodystrophy (MLD) and Hurler syndrome (MPS-IH). Bone Marrow Transplant 30:215-222. 3) Kreysing J, von Figura K, Gieselmann V (1990) The structure of the arylsulfatase A gene. Eur J Biochem 191:627-631. 4) Gieselmann V, Polten A, Kreysing J, von Figura K (1989) Arylsulfatase A pseudodeficiency: loss of a polyadenylation signal and a N-glycosylation site. Proc Natl Acad Sci USA 86:9436-9440. 5) Gieselmann V, Zlotogora J, Harris A, Wenger DA, Morris CP (1994) Molecular genetics of metachromatic leukodystrophy. Hum Mutat 4:233-242. 6) Gieselmann V, Matzner U, Hess B, Lullmann-Rauch R, Coenen R, Hartmann D, D’Hooge R, DeDeyn P, Nagels G (1998) Metachromatic leukodystrophy: molecular genetics and an animal model. J Inherit Metab Dis 21:564574. 7) Polten A, Fluharty AL, Fluharty CB, Kappler J, von Figura K, Gieselmann V (1991) Molecular basis of different forms of metachromatic leukodystrophy. N Engl J Med 324:18-22. 8) Newton CR, Graham A, Heptinstall LE, Powell SJ, Summers C, Kalsheker N, Smith JC, Markham AF (1989) Analysis of any pint mutation in DNA: the amplification refractory mutation system (ARMS). Nucleic Acids Res 17:2506-2516. 9) Eng B, Nakamura LN, O'Reilly N, Schokman N, Nowaczyk MM, Krivit W, Waye JS (2003) Identification of nine novel arylsulfatase a (ARSA) gene mutations in patients with metachromatic leukodystrophy (MLD). Hum Mutat 22:418-419. 10) Eng B, Heshka T, Tarnopolsky MA, Nakamura LM, Nowaczyk MJM, Waye JS (2004) Infantile metachromatic leukodystrophy (MLD) in a compound heterozygote for the c459+1G>A mutation and a complete deletion of the ARSA gene. Am J Med Genet (in press). John S. Waye, PhD Małgorzata J.M. Nowaczyk, MD, FRCPC, FCCMG Discipline of Genetics Hamilton Regional Laboratory Medicine Program