vandana mishra - Clinical Trials Registry
advertisement

EVALUATION OF LABETALOL AS AN ALTERNATIVE TO
MAGNESIUM SULFATE IN THE PREVENTION OF
ECLAMPSIA
Protocol of Thesis to be submitted to the University of Delhi towards
Partial Fulfillment of the Requirement for the Degree of
Doctor of Medicine (Obstetrics & Gynaecology)
(Batch : 2009-2012)
by
VANDANA MISHRA
Department of Obstetrics & Gynaecology,
University College of Medical Sciences &
Guru Teg Bahadur Hospital,
Delhi-110095
1
EVALUATION OF LABETALOL AS AN ALTERNATIVE TO
MAGNESIUM SULFATE IN THE PREVENTION OF
ECLAMPSIA
Protocol of Thesis to be submitted to the University of Delhi towards Partial
Fulfilment of the Requirement for the Degree of
Doctor of Medicine (Obstetrics & Gynaecology)
(Batch : 2009-2012)
…………………………………..
(Signature)
Student:
Dr. Vandana Mishra
Supervisor:
Dr. Gita Radhakrishnan
…………………………………..
Professor
(Signature)
Department of Obstetrics & Gynaecology
UCMS & GTB Hospital
Co-Supervisor: Dr. Suchi Bhatt
Senior Consultant
Department of Radiology
UCMS & GTB Hospital
…………………………………..
(Signature)
Place of Work:
Department of Obstetrics & Gynaecology
University College of Medical Sciences &
Guru Teg Bahadur Hospital, Delhi-110095
2
ABSTRACT
Background: Magnesium sulfate is use extensively for prevention of eclamptic
seizures. Empirical and clinical evidence supports the effectiveness of
magnesium sulfate, however, questions remain as to its mechanism of action
and safety profile. Labetalol, a known antihypertensive has been used safely for
many years to treat hypertension in preeclamptic women. Studies have shown
the role of labetalol in prevention of eclampsia in women with preeclampsia.
Study Design: Prospective randomized comparative active controlled clinical
trial.
Objective: To evaluate the efficacy of labetalol in prevention of eclampsia in
women with severe pre-eclampsia.
Subjects: 60 patients with severe preeclampsia either in labour or requiring
termination of pregnancy will be included in the study.
Intervention: Patients will be divided in two groups to receive either labetalol
(oral or parenteral) or magnesium sulfate as per the standard protocol. Nifedipine
will be the additional anti hypertensive agent added in both the groups to attain
the target blood pressure.
Outcome measure: Primary outcome measure will include the occurrence of
eclamptic seizure(s) after enrolment in the study. Need for additional
antihypertensive agent, delivery parameters and complications or adverse drugs
effects in mother and intrapartum fetal distress and need and duration of NICU
admission in babies will be included in the secondary outcome measures.
Statistical analysis: Chi-square and Fisher’s exact test will be used for
categoric variables and Student’s t-test for continuous variables. p<0.05 will be
considered significant.
3
INTRODUCTION
Hypertensive disorders of pregnancy constitute the commonest medical disorder
occurring in 6-8%of all pregnancies1. According to National High Blood Pressure
Education Programme (NHBPEP) Working Group and American College of
Obstetricians and Gynecologists (ACOG) hypertension in pregnancy is defined
as diastolic blood pressure (DBP) ≥90 mmHg or systolic blood pressure (SBP)
≥140 mmHg after 20 weeks of gestation in women with previously normal blood
pressure2,3. Pre-eclampsia is a multisystemic disorder of pregnancy usually
associated with raised blood pressure and proteinuria. Although the outcome in
mild cases is often good, in one-third cases the disease is severe and is a major
cause of maternal morbidity and mortality4,5 accounting for nearly 50,000 of direct
maternal deaths in a year worldwide6. Eclampsia, one of the most dreaded
complications of pre-eclampsia is defined as the occurrence in a woman with
pre-eclampia, of seizures that cannot be attributed to other causes. In developing
countries the estimates vary from 1 in 100 to 1 in 17007.
The pathophysiology of eclampsia is not clear but MRI and Doppler data suggest
that overperfusion of cerebral tissues is a major etiologic factor1,8. Doppler data
have shown that cerebral perfusion pressure (CPP) is abnormally increased in
severe preeclampsia and the autoregulation of middle cerebral artery is affected
by this condition leading to increased CPP9,10. The level of CPP required to
cause barotrauma and seizures varies between individuals. However, it has been
seen that seizures also occur in women who have mild to no hypertension at the
time of seizures. In these cases, seizure may be a result of abnormal
autoregulatory response consisting of severe arterial vasospasm with rupture of
vascular endothelium and pericapillary hemorrhage. This may lead to
development of foci of abnormal electrical discharge that may cause
convulsions11.
4
The practical implication of these ideas is that the dose and duration of
antihypertensive to be given in preeclampia for prevention of elampsia remains
controversial.
Magnesium sulfate (MgSO4) is the most widely accepted agent for treatment and
prophylaxis of eclamptic seizure. The largest trial conducted so far viz. the
Magpie Trial shows that magnesium sulfate is the drug of choice for seizure
prophylaxis in preeclampsia.
Despite the widespread use of magnesium sulfate, its mechanism of action is not
clear. Magnesium sulfate is given intravenous or intramuscular and requires
specialized nursing training and monitoring to minimize toxicity from respiratory
and cardiac depression. In addition, patients often require an additional
antihypertensive agent. An ideal drug may be one which can be orally
administered, requiring less rigid monitoring and can be given in low resource
settings.
Labetalol,a combined and block is know to reduce CPP in women with
preeclampsia10. It acts by reducing the peripheral vascular resistance with little or
no effect on cardiac output. The potential advantages of using this drug for
treatment of acute severe preeclampsia and for maintaining treatment of
hypertensive disorders include: its effectiveness, low incidence of side effects
and availability of oral and parenteral preparation. Patients who might not
otherwise received seizure prophylaxis with magnesium sulfate due to logistic,
personnel, safety or training issues, will be in position to have treatment started
earlier. If labetalol is proven to be at least as effective as magnesium sulfate,
there will be a simplicity of the management of severe preeclmapsia with a
significant saving in terms of cost and time to reach a tertiary level care.
The current study is a randomized controlled trial to evaluate the role of labetalol
in prevention of eclampsia in women with severe pre-eclampsia.
5
REVIEW OF LITERATURE
Hypertensive disorders during pregnancy form one of the deadly triad along with
hemorrhage and sepsis that contributes greatly to maternal morbidity and
mortality.
The pathophysiology of eclampsia is not known but it is thought to involve
cerebral vasospasm leading to ischemia, disruption of blood-brain barrier and
cerebral edema. Magnetic resonance imaging and Doppler data suggest that
overperfusion of the cerebral tissues is a major etiologic factor1,8. Hypertensive
encephalopathy6 from overperfusion, and vascular damage from excessive
arterial pressure (cerebral barotraumas) are believed to lead to vasogenic and
cytotoxic cerebral edema11, with resultant neuronal anomalies, seizure activity
and cerebral bleeding if left unchecked. Doppler studies have shown that
cerebral perfusion pressure (CPP)
is abnormally increased in severe
preeclampsia and that autoregulation of the middle cerebral artery is affected by
this condition leading to increased CPP.
Commonly used antihypertensive drugs in preeclampsia include labetalol,
hydralazine, nifedipine, nimodipine and for hypertensive emergencies IV
hydralazine, IV labetalol, nifedipine and sodium nitroprusside. According to the
Cochrane database review (2002), all these drugs have been found to be equally
efficacious12. Anticonvulsant therapy is recommended in the management of
severe pre-eclampsia to prevent seizures, and in eclampsia to prevent
recurrence of seizures. The evidence to date confirms the efficacy of magnesium
sulfate in reducing seizures in women with eclampsia and severe preeclampsia.
However, this benefit does not affect overall maternal and perinatal mortality and
morbidity.
A Multinational Eclampsia Trial Collaborative Group (1995) study involved 1687
women with eclampsia who were randomly allocated to different anticonvulsant
6
regimens13,14 and found magnesium sulfate to be superior to diazepam and
phenytoin in prevention of eclampsia. Superiority of magnesium sulfate therapy
over phenytoin was also shown by a study conducted by Lucas et al (1995)14. 10
of 1089 women randomly assigned to phenytoin regimen had eclamptic seizures
compared with no convulsions in 1049 women given magnesium sulfate
(p=0.004).
A randomized controlled trial conducted by Coetzee et al15 (1998) concluded that
the use of magnesium sulfate in management of women with severe preeclasmpsia significantly reduced the development of eclampsia.
The largest ever trial conducted till date, a multicentric randomized, placebo
controlled trial for anticonvulsants, The Magpie Trial7 (Magnesium sulfate for
Prevention of Eclampsia) in 175 hospitals in 33 countries worldwide enrolled
10,141 women with preeclampsia. The trial concluded that women who received
magnesium sulfate were 58% less likely to progress to eclampsia than those who
received placebo. In addition, these women were 45% less likely to die during
childbirth. There was no difference between the two groups in the risk of newborn
death.
Although the exact mechanism of action of magnesium sulfate is not known, the
proposed mechanisms include its cerebral vasodilatory effect (particularly on
small vessels)16, neuromuscular blockade as well as central action by means of
blocking cerebral N-methyl D-aspartate (NMDA) receptors17.But it does not have
any antihypertensive action.
Despite the beneficial effects of magnesium sulfate, it is not an innocuous drug
and requires careful monitoring and affects many maternal and fetal
parameters18. In the mother it can cause flushing, sweating, hypotension,
depressed reflexes, flaccid paralysis, hypothermia, circulatory collapse, cardiac
and CNS depression proceeding to respiratory paralysis which mostly occur due
7
to administration errors. However the benefits of magnesium sulfate therapy
outweigh its potential risks in. Studies have shown that it does not increase the
duration of labor16, maternal blood loss, or caesarean section rate 17, Pruett et al
(1988) found no significant effects on neonatal Apgar scores at the doses of
magnesium sulfate currently in use for seizure prophylaxis19. Many institutions in
developing world lacks lack the necessary expertise to administer the medication
and many preeclamptic patients thus do not receive magnesium sulfate prior to
their first seizure. Given the risks of magnesium sulfate, it is possible that the use
of labetalol may be a safe alternative.
Mahmoud et al20 (1993) prospectively studied the effects of oral labetalol therapy
in patients with blood pressure range 140-150/100-105 mmHg. They concluded
that labetalol is an effective drug in controlling blood pressure and does not
adversely affect umbilical artery flow velocity waveform (UAFVW). It allows safe
prolongation of pregnancies complicated by PIH with a satisfactory fetal
outcome.
ACOG in 1996 recommended labetalol as one of the first line antihypertensive
medication for preeclampsia21.Labetalol, a combined and blocker, has been
used for many years to safely treat hypertension in preeclamptic women. It is a
competitive antagonist of 1 and 2 adrenoreceptors. In humans, the ratio of
and blockade are estimated to be approximately 1:3 and 1:7 for oral and IV
compounds respectively. It lowers the high blood pressure by blocking 1
adrenoreceptors in the peripheral vessels,
thereby reducing peripheral
resistance. Its blockade predominates during IV administration, which prevents
reflex increase in heart rate, cardiac output and myocardial oxygen consumption.
In preeclampia, it rapidly reduces blood pressure without decreasing the
uteroplacental blood flow. It crosses placenta but neonatal bradycardia and
hypoglycemia are rarely seen. Its disadvantages in preeclampsia include interpatient variability in dose requirement and variable duration of action 10. It has
been used both IV and orally for rapid reduction in BP. The Working Group of
8
NHBPEP (2000) recommends starting with a 20 mg IV bolus dose in severe
preeclampsia. If not effective within 10 min, this is followed by 40 mg, then 80 mg
every 10 min, but should not exceed a total of 220 mg per episode. However a
dosage frequency of 20 min with a maximum of 300 mg has also been found to
be equally effective30.The onset of action of IV labetalol is within 5 min and peak
effect is reached within 10-20 min. The peak serum level of labetalol occurs
within 20-60 mins with an elimination half life of 1.7±0.27 hours22. The elimination
half life after intravenous administration in pregnant hypertensive patients is
similar to that seen with oral administration23. The oral dose is 100 mg which can
be increased to 400 mg BD with maximum of 1200 mg/day. The maintenance
dose is usually 200-400 mg BD.
Oral labtetalol has been used for acute control of severe pre-eclampsia and has
been found to be comparable to parenteral hydralazine21. A meta-analysis of
trials revealed that labetalol was no more effective than hydralazine or diazoxide
in decreasing severe hypertension. However, labetalol was associated with less
maternal hypotension, smooth blood pressure control and fewer cesarean
sections. In terms of fetal effects, blood pressure reduction with labetalol did not
result in fetal distress unlike acute BP reduction with hydralazine where 15% of
fetuses exhibited distress requiring immediate cesarean24,25,26. Labetalol also has
antiplatelet aggregation action27, a thromboxane reducing effect28, and fetal lung
maturation accelerating influence29. A meta-analysis of randomized controlled
trials using hydralazine for treatment of severe hypertension does not support the
use of this agent as first line drug when compared with labetalol and nifedipine.
A randomised double blind trial conducted by Vermillion et al30 (1999) to compare
the efficacies of oral nifedipine, a calcium channel blocker and intravenous
labetalol in acute management of hypertensive emergencies of pregnancy
concluded that both are equally effective in management of acute hypertensive
emergencies
of
pregnancy.
However
nifedipine
was
found
to
control
hypertension more rapidly and was associated with a significant increase in
9
urinary output. A study conducted by Belfort et al (2003)8 to compare magnesium
sulfate and nimodipine, a calcium channel blocker with cerebral vasodilatory
effect, for prevention of eclampsia concluded that women who received
nimodipine were more likely to have eclampsia (0.8% versus 2.6%).
Labetalol reduces the cerebral perfusion pressure while maintaining the cerebral
blood flow10. It is potentially an ideal agent for preventing eclampsia which is
believed to be the result of cerebral overperfusion.
Data reported by Walker et al31 over a 10 year period, show the rates of seizures
with labetalol is 1 in 455 (0.2%) in approximately 36000 pregnancies with a 10%
rate of hypertension during pregnancy. Inspired by the above study, LAbetalol
versus Magnesium Sulfate for the Prevention of Eclampsia Trial (LAMPET) was
planned. Labetalol may be a viable alternative to magnesium sulfate for the
prevention of eclampsia as suggested by preliminary data for first 202
participants
in
the
LAMPET
an
international,
multicentral,
non-blinded
randomized controlled trial.
The use of labetalol, which is more specific in mechanism of action, less toxic
agent, which can be administered orally, may simplify the management of severe
preeclampsia. In addition, the facility of administration and reduced risk of
respiratory and cardiac depression, lack of need of intensive monitoring and low
cost of regimen gives labetalol an attractive risk-benefit and cost-benefit ratios.
The drug requires investigations in developing countries as well to establish the
safety and efficacy in population which probably suffers the most from
hypertensive disorders during pregnancy and its complications.
Lacunae in existing knowledge:
Precise intervention for seizure prophylaxis in severe pre-eclampsia is still
unclear
10
Universally accepted regimen of magnesium sulfate requires considerable
training and expertise in administering the drug and rigid monitoring
protocols which are not feasible in many low resource settings in
developing countries like India
Magnesium sulfate regimen also requires an additional antihypertensive
agent
Documentation of the efficacy of an antihypertensive agent which can be
given orally and also brings about prevention of seizures with equal
efficacy as magnesium sulfate would be highly desirable
11
AIMS AND OBJECTIVES
Aim
Evaluation of Labetalol in prevention of eclampsia in patients with severe preeclampsia
Objective
1.
To evaluate the effect of labetalol in prevention of eclampsia in patients
with severe preeclampsia.
2.
To compare the efficacy of labetalol with magnesium sulfate regimen in
prevention of eclampsia in patients with severe preeclampsia.
12
MATERIALS AND METHODS
Study design: A prospective, randomized, comparative clinical trial with active
control.
Study setting: A total of 60 patients with severe preeclampsia either in labour or
requiring termination of pregnancy admitted in the Department of Obstetrics and
Gynaecology, Guru Teg Bahadur Hospital and University College of Medical
Sciences, Delhi will be enrolled in the study from November 2009-April 2011. A
clearance from ethical committee will be taken.
Inclusion Criteria
1 Systolic blood pressure 160mm Hg and diastolic 110mmHg with any
proteinuria (≥300mg/dl or ≥1+ on dipstick)
2 Blood pressure of any range with at least one of the following
a) proteinuria (≥2+ on dipstick or ≥5 g/24 hour urine collection)
b) Persistent frontal headache.
c) Visual or cerebral disturbances.
d) Epigastric or right upper quadrant pain.
e) Persistent clonus and/or hyperreflexia
f) HELLP syndrome - Hemolysis, elevated liver enzymes (LDH >600 U/l,
AST ≥70 U/l), low platelet (<100 x 109/l) or partial HELLP syndrome
consisting of only one or two elements of the above triad.
Exclusion Criteria
1. Eclampsia.
2. Deranged renal functions (urine output <100 ml/4 hour, urea >10 mmol/l
3. Pulmonary edema
4. Imminent LSCS indication
5. Received antihypertensive agent within 6 hours prior to enrollment
6. Already on magnesium sulfate
13
7. Known case of myasthenia gravis
8. Known hypersensitivity to magnesium
9. Refusal or inability to obtain informed consent.
Consent
All patients selected for the study will be explained about the trial. Written
informed consent (Annexure-1) will be taken.
Pre treatment workup (Annexure-2)
History
A detailed history with specific reference to period of gestation, duration
and onset of labour, time of rupture of membranes in patients in labour
and symptoms of impending eclampsia.
Examination
General physical examination – in particular blood pressure, respiratory
rate, presence of deep tendon reflexes, edema and cyanosis
Systemic examination
Obstetric examination to assess the route of delivery
Recording of BP
Women should be seated or lying at 45° with arm at level of heat
Mercury sphygmomanometer with appropriate sized cuff will be used
Phase-V of Korotkoff sound will be taken as the measure of DBP, when
phase V is absent phase IV (muffling) will be accepted
Investigations
Haemogram with platelet count
Peripheral smear for hemolysis
Urine albumin (by dipstick analysis)
Blood urea, serum creatinine, serum electrolytes
14
Coagulation profile: Prothrombin time (PT), Partial thromboplastin time
(PTTK)
Liver function tests (Serum bilirubin, AST, ALT,LDH)
Ophthalmological examination of fundus
Routine antenatal investigations - blood grouping, Rh typing, voluntary
councelling test for HIV,VDRL etc., if not already done
Randomization of Patients
After the initial workup, randomization will be done using computer generated
random numbers to one of the two treatment groups –
Group A: Labetalol group (study group)
Group B: Magnesium sulfate group (control group)
Intervention
Group A (labetalol group)
According to the mean arterial pressure (MAP), patients will be given either oral
or intravenous (iv) labetalol loading dose
MAP 125 mmHg- 20 mg iv , with repeat dose of 40 mg, 80 mg, 80 mg given
every 20 min till BP < 150/100 mmHg or a maximum of 5 doses after which
Nifedipine will be given as per in group B.
MAP <125 mmHg- Patients will receive 200 mg oral labetalol
Maintenance dose: irrespective of whether loading dose was iv or oral, a dose of
200mg labetalol every 6 hours from the time of inclusion in the study will be
given.
Patients developing eclamptic seizures will be given therapeutic magnesium
sulfate regimen as in group B.
15
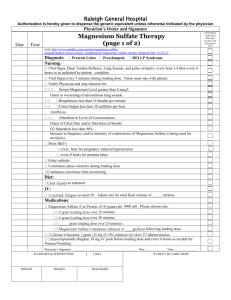
Group B (magnesium sulfate group)
Patients will receive 4 gm of magnesium sulfate as a 20% solution loading dose
slow iv followed by magnesium sulfate 5 gm of 50% solution deep
intramuscular(IM) in upper outer quadrant of both buttocks and maintenance
dose of 5 gm in 50% solution deep IM in alternate buttock every 4 hour after
ensuring:
1) Patellar reflex is present
2) Respiratory rate >14/min
3) Urine output in previous 4 hrs exceeds 100 ml
Patients with MAP ≥125 mmHg will receive Nifedipine 10 mg oral capsule in
incremental doses repeated every 20 min until DBP<100mmHg and SBP<150
mmHg or a maximum of 5 doses. If BP is still not controlled labetalol will be given
as in group A.
In both the groups requirement of postpartum antihypertensive therapy will be
assessed based on the blood pressure levels.
Obstetric Management
Induction of labour where indicated will be done as per standard protocol
based on Bishop score
Maternal and fetal monitoring along with monitoring of progress of labour
will be carried out as per norms of management of any high risk
pregnancy (Annexure-3)
Cesarean section, under appropriate anaesthesia will be performed where
indicated and the anaesthetist will be informed about the medications.
Presence of pediatrician will be ensured for all cases
Cord blood sugar levels will be taken after delivery of placenta
OUTCOME MEASURE
Primary outcome measure
1. Occurrence of eclamptic seizure(s) after enrollment in the study.
16
Secondary outcome measures
Maternal
1. Need for additional antihypertensive medication
2. Subjective assessment of side effects by the patient.
3. Objective assessment of new onset complications and/or side effects by
the treating clinicians
4. Labor and delivery parameters including induction to delivery interval
Fetal and neonatal outcome
1. Intrapartum fetal distress
2. 5 min Apgar score
3. Any neonatal complication
DATA ANALYSIS
Data analysis will be done using SPSS software (version 17).
Chi-square and Fisher’s exact test will be used for categoric variables and
Student’s t-test for continuous variables. p<0.05 will be considered significant.
17
REFERENCES
1.
Hypertension
in
Pregnancy,
ACOG
Technical
Bulletin
No.
219,
Washington DC: The College; 1996: 1-8.
2.
NHBPEP Working Group on High Blood Pressure. Report of NHBPEP
Working Group in Hypertension in Pregnancy. Am J Obstet Gynecol 2000;
183: S1-22.
3.
Diagnosis and management of preeclampsia and eclampsia. Practice
bulletin No.33.Washington DC: Am J Obstet Gynecol, 2002.
4.
Hauth JC, Ewell MG, Levine RJ, et al. Pregnancy outcomes in healthy
nulliparas who developed hypertension. Obstet Gynecol 2000; 95: 24-8.
5.
Sibai BM, Mercer BM, Schiff E, et al. Aggressive versus expectant
management of severe preeclampsia at 28-32 weeks gestation: a
randomized controlled trial. Am J Obstet Gynecol 1994; 171: 818-22.
6.
Belfort MA, Varner MW, Dizon-Townson DS, Grunewald C, Nisell H.
Cerebral perfusion pressure, and not cerebral blood flow, may be the
critical determinant of intracranial injury in preeclampsia: A new
hypothesis. Am J Obstet Gynecol 2002; 187: 626-34.
7.
Altman D, Carroli G, Duley L. Do women with preeclampsia and their
babies benefit from magnesium sulfate? The Magpie Trial: a randomized
placebo controlled trial. Lancet 2002; 359(9321): 1877-90.
8.
Belfort MA, Anthony JA, Saade GR, Allen JC. Magnesium sulfate versus
nimodipine for the prevention of eclampsia. N Engl J Med 2003; 348: 30411.
9.
Belfort MA. Is CPP and cerebral flow predictor of impending seizures in
preeclampsia? A case report. Hypertens Preg 2005: 24(1): 59-63.
10.
Belford MA, Tooke-Miller C, Allen JC Jr, Dizon-Townson D, Warner MA.
Labetalol decreases cerebral perfusion pressure without negatively
affecting cerebral blood flow in hypertensive gravidas. Hypertens Preg
2002; 21(3): 185-97.
11.
Cunningham FG, Lindeimer MD. Hypertension in pregnancy: Current
18
concepts. N Engl J Med 1992; 326: 927-30.
12.
Duley L, Henderson-Smart DJ. Drugs for treatment of very high blood
pressure
during
pregnancy.
Cochrane
Database
Sys
Reb
2002;(4):CD001449.
13.
Eclampsia Trial Collaborative Group. Which anticonvulsant for women
with eclampsia? Evidence from the collaborative eclampsia trial. Lancet
1995; 345: 1455-63.
14.
Lucas MJ, Leveno KJ, Cunningham FG. A comparison of magnesium
sulfate with phenytoin for the prevention of eclampsia. N Engl J Med 1995;
333: 201-8.
15.
Coetzee EJ, Dommisse J, Anthony J. A randomised controlled trial of
intravenous magnesium sulphate versus placebo in the management of
women with severe pre-eclampsia. Br J Obstet Gynaecol 1998; 105: 3003.
16.
Michael A, Belfort MA, Moise KJ. Effect of magnesium sulfate on maternal
brain blood flow in preeclampsia. A randomized placebo controlled study.
Am J Obstet Gynecol 1992; 167: 661-6.
17.
Gambling DR. Hypertensive disorders. In: Chestnut DH, ed. Obstetric
Anaesthesia: Principles and Practice, 3rd ed. Mosby; 2004: 794-837.
18.
Katz VL, Farmer R, Kuller JA. Preeclampsia into eclampsia. Towards a
new paradigm. Am J Obstet Gynecol 2000; 182: 1389-96.
19.
Pruett KM, Krishon B, Cotton DB, et al. The effects of magnesium sulfate
therapy on Apgar scores. Am J Obstet Gynecol 1988; 159: 1047-8.
20.
Mahmoud TZ, Bjornsson S, Calder AA. Labetalol therapy in pregnancy
induced hypertension: the effects on fetoplacental circulation and fetal
outcome. Eur J Obstet Gynecol Reprod Biol 1993; 50(2): 109-13.
21.
Management of Preeclampsia, ACOG Technical Bulletin, No. 219,
February,
1996.
The
American
College
of
Obstetricians
and
Gynecologists. Washington, DC.
22.
Rogers RC, Sibai BM, Whybrew WD. Labetalol pharmacokinetics in
pregnancy-induced hypertension. Am J Obstet Gynacol 1990; 162: 362-6.
19
23.
Rubin PC, Butters L, Kelman AW, Fitzsimons C, Reid JL. Labetalol
disposition and concentration-effect relationships during pregnancy. Br J
Clin Pharmacol 1983; 15: 465-70.
24.
Spinnato TA, Sibai BM, Anderson GD. Fetal distress after hydralazine
therapy for severe PIH. South Med J 1986; 79: 559-62.
25.
Michael CA. Use of labetalol in treatment of severe hypertension during
pregnancy. Br J Clin Pharmacol 1979; 8: S211-5.
26.
Riley AJ. Clinical pharmacology and labetalol in pregnancy. J Cardiovasc
Pharmacol 1981; 3: S53-9.
27.
Greer IA, Walker JJ, McLaren M, Calder AA, Forbes CD. A comparative
study of the effects of adrenoreceptor antagonists on platelet aggregation
and thromboxane generation. Thromb Haemost 1985; 54: 480-4.
28.
Greer IA, Walker JJ, Maclaren M, Calder AA, Forbes CD. Inhibition of
thromboxane and prostacyclin in whole blood by adrenoreceptor
antagonists. Prostaglandins Leukotrienes Med 1985; 19: 209-17.
29.
Michael CA. Early fetal lung maturation associated with labetalol therapy.
Singapore J Obstet Gynaecol 1980; 11: 2-5.
30.
Vermillion ST, Scardo JA, Newman RB, et al. A randomized double blind
trial of oral nifedipine and IV labetalol in hypotensive emergencies of
pregnancy. Am J Obstet Gynecol 1999; 181: 858-61.
31.
Walker JJ. Preeclampia. Lancet 2000; 326: 1260-5.
20
ANNEXURE-1
INFORMED CONSENT FORM
I _______________________ am willing to enroll myself in the study titled
“EVALUATION OF LABETALOL AS AN ALTERNATIVE TO MAGNESIUM
SULFATE IN THE PREVENTION OF ECLAMPSIA”. I give my full free and
voluntary consent for examination, any intervention and publication.
I also give my voluntary consent to be enrolled in either treatment group (drug or
placebo as the case may be) depending upon the randomized allocation.
Signature / thumb impression
of patient
Signature / thumb impression
of witness
Date
Doctor’s signature
®úÉäMÉÒ EòÉ ºÉ½þ¨ÉÊiÉ {ÉjÉ
¨Éé ………………………………………… +{ÉxÉÒ º´ÉäSUôÉ ºÉä
ÊSÉÊEòiºÉEòÒªÉ
+vªÉªÉxÉ
¨Éå
+{ÉxÉä
+É{ÉEòÉää
ºÉΨ¨ÉʱÉiÉ Eò®úxÉä EòÒ ºÉ½þ¨ÉÊiÉ |ÉnùÉxÉ Eò®úiÉÒ
½ÚÄþ*
¨ÉÖZÉä
ºÉä´ÉÉ
|ÉnùÉxÉ
Eò®úxÉä
´ÉɱÉä
ÊSÉÊEòiºÉEò xÉä ¨ÉÖZÉä ºÉÆiÉÖι]õ EòÒ ºÉÒ¨ÉÉ iÉEò
<ºÉ ÊSÉÊEòiºÉEòÒªÉ +vªÉªÉxÉ EòÒ |ÉEÞòÊiÉ ´É =qäù¶ªÉ
ºÉä ¦É±ÉÒ ¦ÉÉÆÊiÉ +´ÉMÉiÉ Eò®úÉ ÊnùªÉÉ ½èþ*
®úÉäMÉÒ Eäò ½þºiÉÉIÉ®ú MÉ´Éɽþ Eäò ½þºiÉÉIÉ®ú
21
+lÉ´ÉÉ +ÄMÉÚ`äö EòÉ ÊxɶÉÉxÉ +lÉ´ÉÉ +ÄMÉÚ`äö EòÉ
ÊxɶÉÉxÉ
ÊSÉÊEòiºÉEò Eäò ½þºiÉÉIÉ®ú
ÊnùxÉÉÆEò
22
ANNEXURE-2
CASE RECORD FORM
Case no.
CR no.
Date:
Date of admission:
Name:
Age:
Address:
Phone no:
Religion:
Booked/unbooked:
SE status:
Dietary history:
Antenatal medications: Haematinics, calcium supplementation
History
Menstrual history
LMP
EDD
POG
Obstetric history
Any specific complaints
Headache
Epigastric or right upper quadrant pain
Visual symptoms
Decreased urinary output
Respiratory distress
Edema
Convulsions
Others
Past history
Hypertension
Preeclampsia or eclampsia in previous pregnancy
Myasthenia gravis
23
Seizure disorder
Hypersensitivity to magnesium
Nature of treatment received
Family history
Examination
General physical examination
Vitals
Pulse rate
Blood pressure
Respiratory rate
Pallor / icterus / cyanosis / edema
Systemic examination
Respiratory
Cardiovascular
Per abdomen
Per vaginum
Bishop score
Investigations
Routine
Hb
BG
VDRL
GCT/GTT9glucose challenge test/ glucose tolerance test)
Urine routine :albumin, sugar,
Special
Hemogram with platelet count
24
Peripheral Smear for hemolysis
Urine albumin (by dipstick analysis)
Serum uric acid
Blood urea, Serum electrolytes, Serum creatinine
Coagulation profile
Liver function tests
Ohphthalmological examination of fundus
Details of neonate
Birth weight
Apgar score
Neonatal resuscitation
NICU stay
Neonatal morbidity / mortality
Condition at discharge
25
ANNEXURE-3
PARTOGRAPH
26