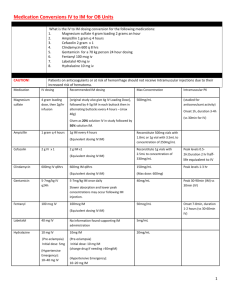
I. Empiric Dosing (this step is for both TD and EID)
advertisement

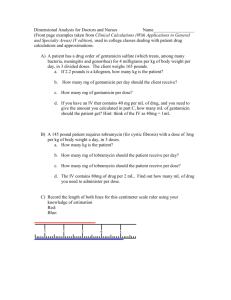
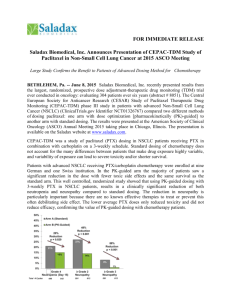
A Apppprroovveedd bbyy PP++TT,, 1111//0044 Therapeutic Drug Monitoring and Pharmacokinetics of Aminoglycosides for Pharmacists and Other Healthcare Professionals Purpose of this document: This document is a Section of Infectious Disease & Pharmacy consensus statement of agreed upon dosing and drug monitoring recommendations. Comprehensive Antimicrobial Program (CAP) Approved Indications: AMIKACIN-Prior approval needed and automatic review within 72 hours A. Prophylactic use: none. B. 1. C. 1. 2. 3. Empiric use: Seriously ill patient in whom an infection with P. aeruginosa (or other resistant GNR) resistant to tobramycin is suspected. Therapeutic use: Patient with infection caused by GNR resistant to all other agents. Patient with severe infection by an agent that requires combination therapy and is resistant to other aminoglycosides. Treatment of infection caused by Mycobacterium avium complex. GENTAMICIN-Unrestricted TOBRAMYCIN-No prior approval needed, review within 72 hours A. B. Prophylactic use: none. Empiric use: 1. In combination with cefepime for neutropenic fevers. 2. In combination with piperacillin for 48 hours when severe P. aeruginosa infection suspected. C. 1. Therapeutic use: With appropriate ß-lactam for GNR infection resistant to gentamicin, when combination therapy is deemed necessary (e.g. P. aeruginosa) Aminoglycoside antibiotics are active against many aerobic gram-negative bacilli (GNB), including Pseudomonas aeruginosa. In reduced doses, gentamicin is also used as an adjunctive synergistic agent in combination with cell wall active agents such as vancomycin or ß-lactams for the treatment of serious infections involving many aerobic gram positive cocci (GPC). 1 A Apppprroovveedd bbyy PP++TT,, 1111//0044 Two dosing strategies are available for patients placed on aminoglycosides. These strategies are extended interval (once daily) dosing (EID) or traditional dosing (TD). Extended interval dosing is appropriate for patients with presumed or documented GNB infections only. While EID is only appropriate for GNB, TD is appropriate for both infections due to susceptible GNB (EID is the preferred method) and for synergy against GPC. A lower dose (generally 1mg/Kg of dosing weight (DW) is preferred for synergy. Data has shown that EID has similar efficacy and may have decreased toxicities over traditional dosing methods. In addition, EID has the convenience of easier dosing and has fewer drug levels to monitor. How to Decide on an Aminoglycoside Dosing Strategy Gentamicin, Tobramycin or Amikacin Indicated Treating GNB Treating GPC (gentamicin only) Use 1mg/Kg dosing (TD only) EID (Preferred) TD I. Empiric Dosing (this step is for both TD and EID) A. Calculate DW-All expressed in kilograms 1. Ideal body weight (IBW): a. Males:50 + 2.3(height in inches-60) b. Females:45.5 + 2.3(height in inches-60) c. If IBW>Actual body weight (ACTBW) then use ACTBW as dosing weight B. Adjusted body weight (ADJBW ): Use if ACTBW >120% of IBW 1. ADJBW = IBW + 0.4(ACTBW - IBW) 2 A Apppprroovveedd bbyy PP++TT,, 1111//0044 C. Calculate creatinine clearence (CrCL): (ml/min) 1. Use urine CrCL if available: Urine volume (ml/24hrs) 1440 x x Urine creatinine (mg/dl) Serum creatinine (mg/dl) 2. Estimated CrCL: Use Crockoft and Gault Method1 (140-age) x IBW or ADJBW x 0.85 (females only)____ 72 x SCr D. Empiric Traditional Dosing 1. Choose a loading dose (LD), maintenance dose (MD) and interval a. LD 1. Tobramycin or gentamicin =2mg/Kg of DW b. MD and dosing interval: Adjust dosing interval PRN based on the Hull-Sarubbi Nomogram c. For synergy with cell wall active agents (gentamicin only) in the treatment of gram positive infections, dosing is 1mg/kg Q8H (NO LOADING DOSE NEEDED) Hull-Sarubbi Nomogram CrCL Percentage of LD to use for Dosing Interval (ml/min) MD >90 84 Q8H 80 80 Q8H 70 76 Q8H 60 84 Q12H 50 79 Q12H 40 72 Q12H 30 86 Q24H 20 75 Q24-36H <20 Give LD x1, then check random level(s) *Ann Intern Med 1978; 89: 612-618 2. When is it appropriate to obtain serum aminoglycoside levels? a. Utilization of serum aminoglycoside concentrations may be used to help ensure adequate levels are achieved at the site of infection, for those patients with altered pharmacokinetics and in populations that are at increased risk to help avoid or identify toxicity. It is important to keep in mind that acute renal failure can occur even if drug levels are closely monitored, although the risk is clearly greater in those patients with levels outside the therapeutic range.2,3 3 A Apppprroovveedd bbyy PP++TT,, 1111//0044 b. Populations who DO NOT require serum aminoglycoside levels: 1. Predicted duration of therapy less than 5 days with the following characteristics a. Stable, normal renal function b. No concurrent nephrotoxins c. Not volume depleted d. Absence of hypotension or impaired renal perfusion 2. For those that require serum levels, a peak and a trough should be obtained after 4-5 half lives (typically the 3rd or 4th maintenance dose) and subsequently every 7 days, with lack of efficacy, signs of toxicity or with a 25% change in serum creatinine or CrCL. 3. Special Populations a. Neonates Postconseptual Age (weeks) Postnatal Age (days) Gent or Tobra Dose (mg/Kg/dose) Amikacin Dose (mg/Kg/dose) Dosing Interval (hours) < 29 0-28 >28 0-14 >14 0-7 0-7 >7 >7 2.5 3 3 2.5 4 4 - 7.5 10 10 7.5 7.5 7.5 24 24 24 12 24 12 24 8 30-36 >37 *All Pediatric dosing based on The Harriet Lane Handbook, Sixth edition a. Infants and Children 1. Gentamicin and Tobramycin i. 2 to 2.5mg/Kg every 8 hours 2. Amikacin i. 5 to 7.5mg/Kg every 8 hours c. Ascites-Patients receiving aminoglycosides who have ascites typically have a larger volume of distribution (VD) than the normal population, due to the hydrophilic nature of the drug class. The VD in patients who have ascites typically is 0.3-0.35 L/Kg versus ~0.25L/Kg in the normal population4. Serum levels should be monitored closely. 4 A Apppprroovveedd bbyy PP++TT,, 1111//0044 d. Elderly patients- More than 85% of the elimination of all aminoglycosides is accounted for by renal clearance. Therefore, it is not unexpected that linear regression models have shown a direct correlation between CrCL and the aminoglycoside elimination rate constant5 Similarly, pharmacokinetic studies have found a direct relationship between age and diminished renal function, although, to date no firm relationship has been established between age and decreased aminoglycoside clearance 6,7. Given this information, dosing should be based on CrCL not age. One must also keep in mind that the elderly have a higher incidence of dehydration and decreased plasma proteins (albumin) that may influence aminoglycoside dosing, so serum levels should be monitored closely. Ultimately, after the clinician reaches a dose they think is appropriate based on the methods provided, they should review the patients clinical situation, weight and renal function and decided if the dose is acceptable. The ID pharmacist may be consulted as needed. e. Burn patients-Patients with burns of greater than 20% of their body should NOT be placed on EID of aminoglycosides8. This is due to the unpredictability of the drug clearance and volume of distribution in this patient population9. It is apparent that large variations in dosages and dosing intervals may be needed to achieve therapeutic levels of aminoglycosides. Many patients may require either increased dosages or more frequent dosing intervals to achieve their target serum levels, or both. However, this should not be interpreted as a steadfast rule. Early research by Zaske and colleagues has shown that patients receiving individualized dosing regimens have a statistically significant reduction in mortality compared to patients who receive a standard dosing regimen10. Patients placed on aminoglycosides with burns greater than 20% of their body should receive a traditional dosing regimen and serum levels with the 3rd maintenance dose. Patients who are started on aminoglycosides within 48 hours of a > 20% burn injury should have levels drawn with the 3rd maintenance dose and with the 6th 9th maintenance dose due to the changing burn pharmacokinetics before and after 48 hours8. Patients placed on aminoglycosides after a > 20% burn injury should be dosed at 3mg/Kg every 8 hours (adjust dosing interval based on CrCl), and serum levels should be monitored closely11. f. Critically ill/surgery patients-Critically ill patients who have undergone surgery may receive EID aminoglycosides based on the Hartford Nomogram guidelines. Frequently, patients in this subpopulation who receive aminoglycosides (EID and TD) will have sub-therapeutic serum levels initially. This is due to the large 5 A Apppprroovveedd bbyy PP++TT,, 1111//0044 VD that is commonly seen in this patient population. Typical VD’s are 0.3-0.4 L/Kg as compared to ~0.25L/Kg seen in patients with normal pharmacokinetics12-14. Some traditional dosing studies suggest a larger initial dose (such as 3mg/Kg) might be necessary in critically ill patients, but no consensus has been reached on this issue as of yet15. To complicate the clinical picture, these patients commonly present with renal insufficiency or even acute renal failure. Serum levels should be drawn with the 3rd or 4th maintenance dose to ensure they are within the therapeutic range. e. Cystic fibrosis (CF)- The renal clearance of aminoglycosides is considerably accelerated in CF patients for unclear reasons, requiring starting doses that are approximately triple (usually 3mg/Kg Q8h) those normally recommended. Volumes of distribution are also increased and are thought to be from a lack of adipose tissue in CF patients (and a resultant increase in the percentage of hydrophilic tissue). It is critically important to measure peak and trough blood levels soon after the initiation of treatment because considerable variation exists in clearance rates. Extrapolation of EID in CF patients is uncertain. Pharmacokinetic studies of once-daily tobramycin in CF patients showed that the time spent with serum levels less than the minimal inhibitory concentration was significantly longer than in non-CF individuals16. Pending the results of ongoing multicenter trials, a general recommendation for once daily dosing of aminoglycosides in these patients cannot yet be made. Some practitioners, who specialize in the treatment of older CF patients here at DHMC routinely, do use tobramycin EID (10mg/Kg). Nevertheless, the current available data show a clear consensus that CF patients exhibit a larger VD and enhanced clearance in comparison to nonCF patients for many antibiotics, including aminoglycosides.17,18 E. Empiric Dosing Using EID (Hartford Nomogram) 1. Should NOT be used in the following populations a. < 13 y/o b. Allergy to aminoglycosides c. Ascites d. CRCL<20 ml/min e. Synergy for gram-positive infections f. Extensive burns (>20% of BSA) g. Pregnancy 6 A Apppprroovveedd bbyy PP++TT,, 1111//0044 2. Dosing a. Tobramycin and gentamicin =7mg/Kg based on DW 3. Initial dosing interval a. Initial dosing interval should be based on CrCL as described in the table below. Obtain a random level 6-14 hours after the start of a 1 hour infusion, except as noted b. Q24H Regimens-If duration of therapy is expected to be > 5 days, a random level should be obtained after the first or second dose and weekly thereafter. A Random level is necessary after the first dose if the regimens expected duration is < 5 days and: i. Receiving concurrent nephrotoxic agent(s) ii. Changing renal function iii. Quadriplegic or amputee iv. Patient is in an ICU c. Q36H Regimens- A random level should be obtained after the first or second dose and then weekly thereafter. d. Q48H Regimens- A random level should be obtained after the first dose and then weekly thereafter. CrCl >60 40-60 20-40 <20 Dosing Interval Q24H Q36H Q48H Use traditional dosing and follow serial levels II. Dosing Modifications based on level(s) obtained (TD) A. Traditional Dosing using the Sawchuk-Zaske method19 1. Find elimination constant (Ke) Ke = lnC1 - lnC2___ t1-t2 2. Find T1/2 (Want dosing interval to be 2-3 x T1/2) T1/2= 0.693 Ke 3. Find real peak (Cmax) and trough (Cmin) Cmax= __C1_____ e-Ke(t”) Cmin= Cmax (e-Ke(T-t’) ) Symbol Meaning (D) (t’) Dose (mg) Infusion duration (hr) (T) Dosing interval (hr) (t) Time since infusion completion (hr) (t”) Time since completion of infusion when C1 drawn (hr) Volume of distribution (L) (Vd) 7 A Apppprroovveedd bbyy PP++TT,, 1111//0044 4. Find volume of distribution (Vd) in liters Vd= ___ Dose (mg) x (1-e-Ke(t’) ) t’*Ke (Cmax – Cmin e-Ke(t’) ) 5. Find new dose (mg) based on peak level (from chart below) Dose= Cmax (desired) * Ke*Vd*(1-e-Ke(T) )*t’ 1-e-Ke(t’) 6. Calculate new peak and trough Cmax(new)= _____Dose(mg)* (1-e-Ke(t’) )_______ t’*Ke*Vd (1-e-ke(T) ) Cmin(new)= Cmax (e-Ke(T-t’) ) Gentamicin and Tobramycin Target Serum Levels for Specific Disease States/Etiologies Infection Type Target Peak Target Trough Gram-positive infections 4 mg/L <2 mg/L Most gram-negative infections 6-8 mg/L <2 mg/L Gram-negative pneumonia 8-10 mg/L <2 mg/L UTI 4-6 mg/L <2 mg/L Cystic Fibrosis 10-12 mg/L <2 mg/L P. aeurgenosa (non-UTI) 9-11 mg/L <2 mg/L Amikacin 15-30 mg/L <8 mg/L *amikacin serum levels are a send out 8 A Apppprroovveedd bbyy PP++TT,, 1111//0044 B. Dosing Modifications based on level(s) obtained (EID) 1. Evaluate using the Hartford Nomogram below a. If the level falls in the area designated q24h, q36h or q48h the dosing interval should be adjusted as needed. b. If the level falls directly on a line choose the longer of the two dosing intervals c. If the 6-14 hour post level is < 2 mg/L then use TD d. For amikacin double the serum concentrations on the Y axis of the nomogram III. Monitoring the patient- In addition to serum levels the following information should be monitored daily. A. Laboratory parameters 1. Serum creatinine (or CrCL) a. Monitor for trends and adjust doses based on Hartford or Hall & Sarubbi Nomogram if not following serum drug levels 2. Blood urea nitrogen a. BUN / Scr ratio of > 20 may indicate a pre-renal state (dehydration) representing a smaller VD and subsequent increased levels 3. White blood cell count (WBC) a. Trends in WBC count help evaluate physiologic response to treatment 4. Microbiology a. Gram stain results i. Aminoglycosides are mainly effective against GNB, but may be used as an adjunctive agents for GPC b. Culture and sensitivity results i. Culture 9 A Apppprroovveedd bbyy PP++TT,, 1111//0044 1. These results should be reviewed to identify the species of the microorganism. ii. Sensitivities 1. Identifies in vitro activity of antibiotics against a specific microorganism B. Monitor for Adverse Drug Reactions (ADR) 1. Nephrotoxicity (Acute tubular necrosis) a. Nephrotoxicity has ranged from 5% to 25% in clinical trials. It is important to note that the criteria used to define nephrotoxicity influences the incidence reported in these trials. b. The risk of nephrotoxicity may be less with EID (Murry et al, 1999) c. Concurrent use of other nephrotoxins, dehydration, pre-existing renal dysfunction, prolonged therapy and increased trough concentrations appear to increase the risk of nephrotoxicity b. Recommended course of action is to withdraw the offending agent(s) and risk/benefit should be discussed with the physician 2. Ototoxicity a. Serious adverse effects on both vestibular and auditory branches of the eighth cranial nerves have been reported in varying ranges (3%-14%) based on the criteria used b. This toxicity is primarily seen in patients with renal impairment (especially if dialysis is required), patients on high doses and/or prolonged therapy, dehydration, and previous/concurrent exposure to other ototoxic agents c. Symptoms include dizziness, vertigo, ataxia, tinnitus, roaring in the ears and hearing loss, which, may be irreversible. d. Hearing loss is usually manifested initially by diminution of high-tone acuity c. Recommended course of action is to withdraw the offending agent(s) and risk/benefit should be discussed with the physician 3. Other Neurotoxicity a. Peripheral neuropathy, numbness, skin tingling, muscle twitching, convulsions, and a myasthenia gravis-like syndrome are all rare occurrences b. Recommended course of action is to withdraw the offending agent(s) and risk/benefit should be discussed with the physician 10 A Apppprroovveedd bbyy PP++TT,, 1111//0044 References 1. Cockroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976:16;31-41. 2. Humes, HD. Aminoglycoside nephrotoxicity. Kidney Int 1988; 33:900. 3. Moore, RD, Smith, CR, Lipsky, JJ, et al. Risk factors for nephrotoxicity in patients treated with aminoglycosides. Ann Intern Med 1984; 100:352 4. Sampliner R, Perrier D, Powell R, Finley P. Influence of acites on tobramycin pharmacokinetics. J Clin Pharmacol 1984; 24:43-6 5. Matzke GR, Jameson JJ, Halstenson CE. Gentamicin disposition in young and elderly patients with various degrees of renal function. J Clin Pharmacol 1987; 27:216-20 6. Bauer LA, Blouin RA. Influence of age on tobramycin pharmacokinetics in patients with normal renal function. Antimicrob Agent Chemother 1981; 20:58789 7. Triggs E, Charles B. Pharmacokinetics and therapeutic drug monitoring of gentamicin in the elderly. Clin Pharmacokinet 1999; 37:331-41 8. Nicolau DP, Freeman CD, Belliveau PP, et al. Experience with a once-daily aminoglycoside program administered to 2,184 adult patients. Antimicrob Agent Chemother 1995; 39:650-5 9. Weinbren MJ. Pharmacokinetics of antibiotics in burn patients. J Antimicrob Agent Chemother 1999; 44:319-27 10. Zaske DE, Bootman JL, Solem LB, Strate RG. Increased burn patient survival with individualized dosages of gentamicin. Surgery 1982; 91:142-9 11. Hollingsed TC, Harper DJ, Jennings JP, et al. Aminoglycoside dosing in burn patients using first-dose pharmacokinetics. J Trauma 1993; 35:394-398 12. Dasta J, Armstrong D. Variability in aminoglycoside pharmacokinetics in critically ill surgical patients. Crit Care Med 1988; 16:327-330 13. Niemec P, Allo M, Miller CF. Effect of altered volume of distribution on aminoglycoside levels in patients in surgical intensive care. Arch Surg 1987; 122:207-212 14. Oparaoji E, Cornwell E, Hekmak E, et al. Aminoglycoside volume of distribution in postoperative patients with septic shock. Clin Pharmacol 1993; 12:131-134 15. Watling SM, Dasta JF. Aminoglycoside dosing considerations in intensive care unit patients. Ann Pharmacother 1993; 27:351-357 16. Beringer, PM, Vinks, AA, Jelliffe, RW, Shapiro, BJ. Pharmacokinetics of tobramycin in adults with cystic fibrosis: implications for once-daily administration. Antimicrob Agents Chemother 2000; 44:809 17. Rey E, Treluyer JM, Pons G. Drug disposition in cystic fibrosis. Clin Pharmacokinet 1998;35:313–329 18. Touw DJ, Vinks AA, Mouton JW, Horrevorts AM. Pharmacokinetic optimisation of antibacterial treatment in patients with cystic fibrosis. Current practice and suggestions for future directions. Clin Pharmacokinet 1998;35:437–459 19. Sawchuk RJ, Zaske DE, et al. Kinetic model for gentamicin dosing. Clin Pharmacol Ther 1977;21;3:362-369 11