906 - جامعة المنيا
advertisement

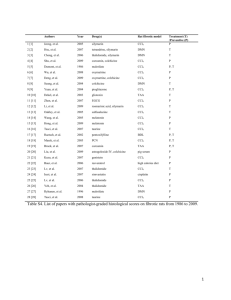
EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ HEPATOPROTECTIVE EFFECT OF NICORANDIL AGAINST CARBON TETRACHLORIDE-INDUCED HEPATOTOXICITY IN RATS By Ashraf Taye*, Mohamed A. El-Moselhy*, Mohamed A. Morsy** and Gamal A. El-Sherbiny*** Departments of Pharmacology and Toxicology, Faculties of Pharmacy, * Minia and ***Beni-Suef Universities; and **Department of Pharmacology, Faculty of Minia Medicine ABSTRACT: Nicorandil (NIC), an anti-anginal drug, was reported to act as an adenosine triphosphate-sensitive potassium (KATP) channel opener, a nitric oxide (NO) donor and also has an antioxidant action. Based on these pharmacological properties, an attempt has been made to evaluate the potential hepatoprotective effect of NIC, and to elucidate its possible mechanism(s) of action in carbon tetrachloride (CCl4)-induced hepatotoxicity in rats. The rats were randomized into 5 groups to receive either vehicle, CCl4, NIC, glibenclamide (GLB, an antagonist of KATP channels), or a combination of NIC and glibenclamide for 5 weeks. NIC administration under CCl4induced intoxication resulted in hepatoprotective effect as evident by significant decrease in serum enzymatic activities of alanine aminotransferase (ALT) and aspartate aminotransferase (AST), hepatic triglycerides, total cholesterol, nitric oxide (NO), and malondialdehyde (MDA) contents, with a concurrent increase in serum albumin level and hepatic catalase activity as compared to CCl4 group. The hepatoprotective effect of NIC was confirmed by histopathological examination of the liver tissues. On the other hand, the protective effect of NIC was maintained in the presence of GLB. In conclusion, NIC has a hepatoprotective effect on CCl4-induced hepatotoxicity in rats may be through, at least in part, its antioxidant activity but not likely to be coupled with activation of KATP channels. KEY WORDS: Nicorandil Glibenclamide Hepatoprotective Carbon tetrachloride et al., 2004), ameliorates lung allograft reperfusion injury through activation of KATP channels (Yamashita, Ogawa, and Akaike, 1996), has anti-apoptotic effects in neurons mediated by KATP channels (Teshima et al., 2003), and protects against gastric ulcer in rats by KATP channel opening and free radical scavenging (Ismail et al., 2007). INTRODUCTION: Nicorandil, an efficacious drug for the treatment of ischemic heart disease, exerts multiple pharmacological actions that involve activation of KATP channels, generation of NO, and scavenging of free radicals (Miura and Miki, 2003). These pharmacological multiactions offer the possibility of interacting with various experimentally-induced pathological conditions usually through one or more of these actions. For examples, NIC improves diabetes and rat islet β cell damage via a radical scavenging effect but not KATP channel opening (Kasono Liver disease is a serious health problem. There is scanty information concerning both the effect of NIC on liver injury and the mechanism(s) involved in this effect. The preventive action of CCl4-induced liver damage 312 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ has been widely used as an indicator of liver protective activity of drugs (Weber et al., 2003). Therefore, the present study was undertaken to evaluate the putative hepatoprotective effect of NIC against CCl4-induced hepatotoxicity as well as to reveal the mechanism(s) implicated in this protective effect. In addition, to determine whether KATP channel opening activity contributes to the likelihood of NIC's hepatoprotection, the effect of NIC alone and in the presence of the KATP channel blocker GLB was studied. treated with the combined administration of CCl4 (1 ml/kg) and GLB (3 mg/kg). The fifth group was treated with combined administration of CCl4 (1 ml/kg) and GLB (3 mg/kg) in addition to NIC (3 mg/kg). After completion of 5 weeks, animals were kept starved overnight before being decapitated, blood was collected from orbital sinuous of the eye and the serum obtained was analyzed. Afterwards, liver tissues were immediately dissected out and weighed, fixed in 10% formalin for histopathology or snap frozen in liquid nitrogen and stored at -80°C. Thereafter, the liver tissue was homogenized in 0.25 M sucrose, 10 mM Tris-HCl, 1 mM EDTA medium, pH 7.4, centrifuged at 10,000g for 10 min and supernatants used for biochemical analysis. MATERIALS: Drugs and chemicals Carbon tertrachloride (BDH Chemicals, England); Nicorandil (Torrent, India); Glibenclamide (a kind gift from Aventis Company, Egypt). Animals Adult male Sprague-Dawley rats (150–180 g) were used throughout the experiments. Rats were fed a standard diet of commercial rat chow and tap water ad libitum and left to acclimatize to the environment for at least one week prior to inclusion in the experiments. Experiments were conducted in accordance with the guidelines for animal care of the United States Naval Medical Research Centre, Unit No. 3, Abbaseya, Cairo, Egypt, accredited by the Association for Assessment and Accreditation of Laboratory Animal Care international (AAALAC international). Experimental animals randomly divided into 5 groups (n = 8–10 per group: the first group constituted hepato-intoxicated rats, was i.p. injected CCl4-olive oil(1:1,1 ml/kg) (Sur-Altiner and Yenice, 2000) twice weekly for five weeks, whereas the second served as vehicle control and was given 1 ml/kg, i.p. olive oil in saline, third group was received NIC daily at doses (3 mg/kg, i.p.) for 5 weeks, the fourth group was METHODS: Assessment of serum aminotransferases and albumin Serum ALT, AST and albumin levels were determined using spectrophotometric assay kits purchased from (Randox, Laboratory. Ltd., UK). Estimation of hepatic triglycerides, total cholesterol, catalase, malondialdehyde and nitrite/nitrate levels Liver triglycerides contents were assayed spectrophotometrically as described by Roeschlau et al. (1974) using a commercially available kit (Spectrum, Egypt). Hepatic total cholesterol level was determined also using a commercially available kit (Spectrum, Egypt). Catalase activity in liver homogenates was determined spectrophotometrically as described by Aebi (1984) using commercially available kit (Biodiagnostic, Egypt). Lipid peroxidation was determined in liver homogenates as thiobarbituric acid reactive species (TBARS; sometimes refereed to as MDA) as a marker of oxidative stress according to 313 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ the previously described method (Buege and Aust, 1978). The total of nitrate/nitrite in the samples was assayed as nitrite after reduction of nitrate into nitrite using the cadmium reduction method as described by Sastry and his colleges (Sastry et al., 2002). All parameters measured in hepatic tissues were normalized to the protein content of the homogenate. KATP potassium channel blocker, GLB. It is observed that administration of GLB does not block the protective effect of NIC. Effect of various treatments on hepatic triglycerides, total cholesterol, catalase, malondialdehyde and nitrite/nitrate levels As shown in Figs. 4 and 5, CCl4 administration exhibited a marked increased hepatic MDA levels (p<0.01) (Fig. 4), whereas the hepatic catalase activity significantly (p<0.01) decreased compared to those of control (Fig. 5). NIC had the opposite effect, where it markedly inhibited MDA level and increased the catalase activity nearly to that of control. Compared to control, CCl4 exerted a significant (p<0.001) elevation in hepatic NO level (reflected by total nitrate and nitrite), whereas NIC administration markedly reduced NO production as shown in (Fig. 6). On the other hand, GLB could not reverse the protective effect of NIC on the antioxidant enzyme activities of CCl4-induced liver injury. CCl4 administration resulted in a dramatic elevation of hepatic triglyceride and total cholesterol contents compared to control group (p<0.01 and p<0.001, respectively). Simultaneous administration of NIC with CCl4 reduced the lipid profile indices near to those of control. However, GLB administration could not inhibit the protective effect of NIC on lipid profile (Figs. 7 and 8). Histopathological examination Excised liver tissues from each rat were fixed in 100 ml/L neutral formalin, embedded in paraffin, and stained with hematoxylin-eosin (HE) and masson's trichrome. The evaluation of hepatic fibrosis was determined by a semi-quantitative method to assess the degree of histological injury in chronic hepatic fibrosis (Constandinou, Henderson, and Iredale, 2005). Statistical analysis Data are presented as means ± S.E.M. Group comparison were performed (ANOVA) for repeated measures followed by Bonferroni's test. Results were considered statistically significant at p<0.05. RESULTS: Effect of various treatments on ALT, AST and albumin serum levels In the CCl4-induced liver injury, the serum levels of ALT and AST were markedly (p<0.01) raised compared to control group, indicating the severity of hepatic injury caused by CCl4. Daily administration of NIC effectively inhibited the elevated hepatic enzymes ALT and AST (Figs. 1 and 2). Moreover, albumin levels of CCl4-treated group were significantly (p<0.01) reduced. Similarly, NIC administration restores the reduced albumin to its normal level (Fig. 3). To gain insight into the mechanism of hepatoprotective effect of NIC, we examined its effect in the presence of Histopathological studies Hematoxylin and eosin histological slides were evaluated by a blinded investigator and analyzed using a semiquantitative score for steatosis and inflammation. In control group, there are no pathological changes in healthy control livers which showed normal lobular 314 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ architecture with central vein and radiating hepatic cords (Fig. 9) The lesions in the liver of CCL4 + NIC-group group were completely disappeared except for congestion of some portal blood vessels (Fig.11A) and mild and focal vacuolations of some hepatocytes with necrosis of individual hepatocytes (Fig. 11B). The aforementioned lesions were only detected in the liver of 2 rats; meanwhile, the livers of the others were normal. To investigate role of KATP channels in the protective of NIC, we treated the CCl4 with GLB prior to NIC administration. Surprisingly, similar lesions were seen to that described in CCL4 + NIC-group. The portal areas showed congestion of the portal veins and lymphocytic infiltration (Fig. 11C). Ballooning degeneration and rarely fatty change were also seen (Fig. 11D). Consistent with serum ALT and AST levels, histological examination of the liver showed distorted architecture with distorted central vein and multifocal areas of coagulative necrosis along the hepatic parenchyma in CCl4-treated group (Fig.10A). Severe and diffuse fatty change, ballooning degeneration of hepatocytes, mononuclear cell infiltration, hemorrhages and Kupffer cell hyperplasia were detected (Fig. 10B and 10C). The portal triad showed fibrous portal expansion with moderate fibrosis, biliary hyperplasia with formation newly formed bile ductules and moderate round cell infiltration in the portal areas (Fig. 10D). There was marked centrilobular congestion and hemosiderosis. ALT Levels (IU/l) 150 p<0.01 a p<0.05 b 100 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0 Fig. 1: Effect of various treatments on serum alanine aminotransferase (ALT) level. Values are mean ± S.E.M.; (a) versus control group at p< 0.01 and (b) versus (a) at p<0.05. 315 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ p<0.01 a p<0.01 p<0.01 a 100 AST levels (IU/l) ALT Levels (IU/l) 75 b 150 p<0.05 b 50 100 25 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0 Fig. 2: Effect of various treatments on serum aspartate aminotransferase (AST) level. Values are mean ± S.E.M.; (a) versus control group at p<0.01 and (b) versus (a) 0 at p<0.01. Albumin levels (g/dl) ALT Levels (IU/l) 4.5 4.0 3.5 3.0 2.5 2.0 1.5 1.0 0.5 0.0 150 p<0.01 p<0.05 b p<0.05 a a p<0.05 b 100 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 Fig. 3: Effect of various treatments on serum albumin level. Values are mean ± S.E.M.; (a) versus control 0 group at p<0.01 and (b) versus (a) p<0.05. p<0.01 a p<0.01 10.0 150 a p<0.05 b 7.5 ALT Levels (IU/l) Malondialdehyde MDA (nmol/g tisuue) (nmol/ml) 12.5 5.0 p<0.05 b 100 2.5 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0.0 Fig. 4: Effect of various treatmentsMDA on hepatic malondialdehyde level. Values are 0 control group at p<0.01 and (b) versus (a) at p<0.05. mean ± S.E.M.; (a) versus 316 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ p< 0.01 p<0.01b a 100 150 75 ALT Levels (IU/l) Catalase activity (U/g tissue) 125 50 25 0 100 p< 0.01 a p<0.05 b Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 Fig. 5: Effect of various treatments on hepatic catalase activity. Values are mean ± S.E.M.; (a) versus control group at p< 0.01 and (b) versus (a) at p<0.01. 0 p<0.001 a p<0.01 2000 ALT Levels (IU/l) NO2/ NO3 ratio (nmol/g tisuue) 150 1000 a p<0.01 b p<0.05 100 b Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0 Fig. 6: Effect of various treatments on hepatic nitric oxide level. Values are mean 0 ± S.E.M.; (a) versus control group at p< 0.001 and (b) versus (a) at p<0.01. 200 150 p<0.001p<0.01 a a p<0.01 b 150 100 50 ALT Levels (IU/l) Triglyceride contents (mg /g tissue) 250 p<0.05 b 100 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0 Fig. 7: Effect of various treatments on hepatic triglyceride level. Values are mean 0 ± S.E.M.; (a) versus control group at p< 0.001 and (b) versus (a) at p<0.01. 317 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ 25 150 a p<0.01 a 20 15 ALT Levels (IU/l) Total cholestrol contents (mg/g tisuue) p<0.01 p<0.05 p<0.01 b b 100 10 5 Control CCl4 CCl4+GLB CCl4+NIC CCl4+NIC+GLB 50 0 Fig. 8: Effect of various treatments on hepatic total cholesterol level. Values are 0 mean ± S.E.M.; (a) versus control group at p< 0.01 and (b) versus (a) at p<0.01. Fig. 9: Liver of healthy control group showing normal lobular architecture with central vein and radiating hepatic cords, H&E.x300. 318 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ A C B D Fig. 10: A) Liver of CCl4 showing an area of coagulative necrosis (arrow), H&E.x500; B) Liver of CCl4 showing diffuse fatty change (arrowheads) and mononuclear cell infiltration (arrow), H&E.x300; C) Liver of CCl4 showing diffuse fatty change (arrowheads) and hemorrhage (arrow), H&E.x500; and D) Liver of CCl4 showing portal fibrosis (arrows), biliary hyperplasia (arrow-heads) and moderate round cell infiltration in the portal areas, H&E.x100. A B D C Fig. 11: A) Liver of CCl4 + NIC showing congestion of the portal blood vessels (arrows), H&E.x300; B) Liver of CCl4 + NIC showing focal vacuolations of some hepatocytes (arrows) and necrosis of individual hepatocytes (arrowheads), H&E.x500; C) Liver of CCl4 + GLB + NIC showing congestion of the portal veins (arrows) and lymphocytic infiltration (arrowheads), H&E.x500; and D) Liver of CCl4+ GLB + NIC showing congestion of the portal veins (arrows) and ballooning degeneration in the hepatocytes (arrowheads), H&E.x500. 319 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ DISCUSSION: CCl4 has been widely used to induce experimental hepatic damage as it induces liver cell necrosis and apoptosis, and can be used to induce hepatic fibrosis or cirrhosis by its repetitive administration (Constandinou et al., 2005). The changes induced by CCl4 are quite similar to that of acute viral hepatitis. We verified the hepatotoxicity of CCl4 by the increased serum amino-transferases and decreased albumin levels compared to that of the control groups. Raised serum enzyme levels in CCL4injected rats can be attributed to the damaged hepatocellular structural integrity (Xu, et al., 2006). Several reports investigated effects of various agents that protect against liver toxicity induced by CCl4 (Abraldes and Bosch, 2007; Guven, et al., 2003; Tan et al., 2000). Here, we try to emphasize the putative hepatoprotective effect of NIC and the underlying mechanism of this protection. Noteworthy, NIC administration not only normalize the serum aminotransferases to their normal levels but also serum albumin level as well. accelerate several metabolic pathways (Stoyanovsky and Cederbaum, 1999). These radicals appear to affect the adjacent lipids in the tissues and induce lipid peroxidation. We suggest that increased MDA level in the CCl4treated group is attributed to increased lipid peroxidation-associated tissue damage. Our results showed that NIC appears to play a key role in the attenuation of CCl4-induced liver injury. In accordance, NIC appeared to have a protective effect on the lipid peroxidation, as evident by scavenging free radical and increasing the antioxidant catalase enzyme activity. The reduction of lipid peroxidation by NIC might be important because increased oxidative stress is a feature of the CCl4-induced liver injury and significant protection was obtained with the use of antioxidants (Jaeschke, 1990). Moreover, our results showed that CCl4 administration significantly increased liver triglycerides, and total cholesterol, these observations are in accordance with that of Venukumar and Latha (2002). Herein, decreased liver triglycerides, and total cholesterol contents and reduced lipid peroxidation by NIC introduced a more satisfactory explanation for the protective action of NIC against both fatty degeneration and hepatomegaly induced by CCl4 and elucidated that hepatomegaly possibly is induced by an increase in all lipid forms at the expense of protein content; NIC efficiently prevented deterioration of liver function and this may account for its protection against the deleterious effect of CCl4 on fatty liver. Reactive oxygen species, such as superoxide anions, hydrogen peroxide, and hydroxyl radical, produced by the partial reduction of oxygen, are highly unstable and extremely reactive. The short half-lives of many of these species make them highly toxic to tissues (Noyan et al., 2006). Increased lipid peroxidation is generally believed to be an important underlying cause of the initiation of oxidative stress related to various tissue injuries, cell death, and the progression of many acute and chronic diseases (Halliwell, 1997). During the initial phase of CCl4 toxicity following its administration, a large amount of CCl4 is converted to trichloromethyl radical or other radicals, which in turn Interestingly, the present biochemical findings were reflected on the structural changes of the liver as evident by the hepatic necrosis, diffuse fatty changes, portal fibrosis, biliary and Kupffer cell hyperplasia, haemorrhage and mononuclear cell 320 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ infiltration. Such lesions were induced via the formation of free radicals, especially the reactive oxygen species. The hepatotoxicity of CCl4 results from its metabolism by the cytochrome P450 enzyme system into the reactive intermediates, which leads to oxidative stress and causes hepatic necrosis. In consistent with the present findings, the hepatotoxicity effect of CCl4 was subsided and reversed with complete disappearance of hepatic damage after treatment with NIC. Thus, antioxidant effect of NIC appears to play a key role in the attenuation of inflammation, and then preserve the structural integrity of the hepatocellular membrane resulting in amelioration of liver function. GLB to reverse the protective effect NIC in CCl4-induced hepatotoxicity. In conclusion, NIC have a potential hepatoprotectve effect and the possible mechanism of hepatoprotective action of NIC may be due to its antioxidant activity as indicated by protection against increased lipid peroxidation and maintained catalase contents. The rest of the biochemical and histpathological parameters studied indicate the status of structural and functional integrity of the cells and provide further support to the suggestive mechanism of action. Acknowledgment To Dr. Mohamed Hamed Mohamed. Department of Pathology, Faculty of Veterinary Medicine, Zagazig University for his kind help in the histopathology in this work. On the other hand, it has been reported that liver injury induced by CCl4 is associated by elevated NO level due to increased the proinflammatory cytokines tumor necrosis factors- (TNF-) which induce NO expression (Dang et al., 2007). NIC has been shown in rat myocardial mitochondria to produce NO (Sakai et al., 2000), that plays an important role in ischemic preconditioning of rat livers (Peralta et al., 1997). The present study revealed that concurrent administration of NIC with CCl4 restored NO to its normal level. This can be explained by that the released amount of NO from NIC has been consumed in the scavenging of free radicals. Additionally, NIC may also inhibit the inducible NO synthase via its inhibitory effect on TNF- (Zhan et al., 2003). To verify the hepatoprotective mechanism of NIC, we treated rats with GLB as a KATP sensitive channel blocker. Although NIC acts as a KATP-channel opener (Miura and Miki, 2003; Ohta et al., 1991), it is unlikely that the hepatoprotective effect of NIC is via KATP receptors as evident by failure of REFERENCES: 1. Abraldes, J. G., and Bosch, J. (2007). The treatment of acute variceal bleeding. J Clin Gastroenterol 41(10 Suppl 3), S312-7. 2. Aebi, H. (1984). Catalase in vitro. Methods Enzymol 105, 121-6. 3. Buege, J. A., and Aust, S. D. (1978). Microsomal lipid peroxidation. Methods Enzymol 52, 302-10. 4. Constandinou, C., Henderson, N., and Iredale, J. P. (2005). Modeling liver fibrosis in rodents. Methods Mol Med 117, 237-50. 5. Dang, S. S., Wang, B. F., Cheng, Y. A., Song, P., Liu, Z. G., and Li, Z. F. (2007). Inhibitory effects of saikosaponin-d on CCl4-induced hepatic fibrogenesis in rats. World J Gastroenterol 13(4), 557-63. 6. Guven, A., Guven, A., and Gulmez, M. (2003). The effect of kefir on the activities of GSH-Px, GST, CAT, GSH and LPO levels in carbon tetrachloride-induced mice tissues. J 321 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ Vet Med B Infect Dis Vet Public Health 50(8), 412-6. 7. Halliwell, B. (1997). Antioxidants and human disease: a general introduction. Nutr Rev 55(1 Pt 2), S44-9; discussion S49-52. 8. Ismail, H. A., Khalifa, M. M., Hassan, M. K., and Ashour, O. M. (2007). Insights in the mechanisms underlying the anti-ulcer activity of nicorandil. Pharmazie 62(1), 60-6. 9. Jaeschke, H. (1990). Glutathione disulfide formation and oxidant stress during acetaminopheninduced hepatotoxicity in mice in vivo: the protective effect of allopurinol. J Pharmacol Exp Ther 255(3), 935-41. 10. Kasono, K., Yasu, T., Kakehashi, A., Kinoshita, N., Tamemoto, H., Namai, K., Ohno, R., Ueba, H., Kuroki, M., Ishikawa, S., and Kawakami, M. (2004). Nicorandil improves diabetes and rat islet betacell damage induced by streptozotocin in vivo and in vitro. Eur J Endocrinol 151(2), 277-85. 11. Miura, T., and Miki, T. (2003). ATP-sensitive K+ channel openers: old drugs with new clinical benefits for the heart. Curr Vasc Pharmacol 1(3), 2518. 12. Noyan, T., Komuroglu, U., Bayram, I., and Sekeroglu, M. R. (2006). Comparison of the effects of melatonin and pentoxifylline on carbon tetrachloride-induced liver toxicity in mice. Cell Biol Toxicol 22(6), 381-91. 13. Ohta, H., Jinno, Y., Harada, K., Ogawa, N., Fukushima, H., and Nishikori, K. (1991). Cardioprotective effects of KRN2391 and nicorandil on ischemic dysfunction in perfused rat heart. Eur J Pharmacol 204(2), 171-7. 14. Peralta, C., Hotter, G., Closa, D., Gelpi, E., Bulbena, O., and Rosello-Catafau, J. (1997). Protective effect of preconditioning on the injury associated to hepatic ischemiareperfusion in the rat: role of nitric oxide and adenosine. Hepatology 25(4), 934-7. 15. Roeschlau, P., Bernt, E., and Gruber, W. (1974). Enzymatic determination of total cholesterol in serum. Z Klin Chem Klin Biochem 12(5), 226. 16. Sakai, K., Akima, M., Saito, K., Saitoh, M., and Matsubara, S. (2000). Nicorandil metabolism in rat myocardial mitochondria. J Cardiovasc Pharmacol 35(5), 723-8. 17. Sastry, K. V., Moudgal, R. P., Mohan, J., Tyagi, J. S., and Rao, G. S. (2002). Spectrophotometric determination of serum nitrite and nitrate by copper-cadmium alloy. Anal Biochem 306(1), 79-82. 18. Stoyanovsky, D. A., and Cederbaum, A. I. (1999). Metabolism of carbon tetrachloride to trichloromethyl radical: An ESR and HPLC-EC study. Chem Res Toxicol 12(8), 730-6. 19. Sur-Altiner, D., and Yenice, B. (2000). Effect of black tea on lipid peroxide and glutathione levels in female rats. Drug Metabol Drug Interact 16(4), 299-305. 20. Tan, S. Y., Tan, L. H., Teo, S. M., Thiruventhiran, T., Kamarulzaman, A., and Hoh, H. B. (2000). Disseminated nocardiosis with bilateral intraocular involvement in a renal allograft patient. Transplant Proc 32(7), 1965-6. 21. Teshima, Y., Akao, M., Baumgartner, W. A., and Marban, E. (2003). Nicorandil prevents oxidative stress-induced apoptosis in neurons by activating mitochondrial ATP-sensitive potassium channels. Brain Res 990(12), 45-50. 22. Venukumar, M. R., and Latha, M. S. (2002). Antioxidant effect of Coscinium fenestratum in carbon tetrachloride treated rats. Indian J Physiol Pharmacol 46(2), 223-8. 23. Weber, T., Dalen, H., Andera, L., Negre-Salvayre, A., Auge, N., 322 EL-MINIA MED., BULL., VOL. 19, NO. 1, JAN., 2008 Taye et al ___________________________________________________________________________________ Sticha, M., Lloret, A., Terman, A., Witting, P. K., Higuchi, M., Plasilova, M., Zivny, J., Gellert, N., Weber, C., and Neuzil, J. (2003). Mitochondria play a central role in apoptosis induced by alpha-tocopheryl succinate, an agent with antineoplastic activity: comparison with receptor-mediated pro-apoptotic signaling. Biochemistry 42(14), 4277-91. 24. Xu, Q., Shen, Y. P., and Xu, A. L. (2006). [Cystic degeneration in liver injury induced by CCl4 in SD rats]. Zhongguo Zhong Yao Za Zhi 31(22), 1880-1. 25. Yamashita, Y., Ogawa, H., and Akaike, N. (1996). ATP-induced rise in apamin-sensitive Ca(2+)-dependent K+ conductance in adult rat hepatocytes. Am J Physiol 270(2 Pt 1), G30713. 26. Zhan, Y. T., Wei, L., Chen, H. S., Cong, X., Fei, R., and Wang, Y. (2003). [Differentiation of bone marrow stem cells in rat hepatic fibrogenesis environment]. Zhonghua Gan Zang Bing Za Zhi 11(11), 673-5. التأثير الواقي للنيكورانديل ضد التسمم الكبدي المستحدث بمادة رابع كلوريد الكربون في الجرذان أشرف أبو الوفا طايع* ،محمد أحمد المصيلحي* ،محمد علي مرسي**، جمال أحمد الشربيني*** *قسم األدوية والسموم – كلية الصيدلة – جامعة المنيا * ،قسم األدوية – كلية الطب – جامعة المنيا *** ،قسم األدوية والسموم – كلية الصيدلة – جامعة بني سويف يعتبر عقار النيكورانديل المضاد للذبحة الصدرية واحدًا من محفزات قنوات البوتاسيوم الحساسة تأثيرا مانعًا لألكسدة .واعتمادًا لألدينوسين ثالثي الفوسفات ،ومولدًا ألكسيد النيتريك ،كما أن له ً على هذه الخصائص فقد أجريت محاولة لتقدير تأثير النيكورانديل الواقي للكبد ولتوضيح آليات هذه التأثيرات الوقائية في حاالت التسمم الكبدي المستحدث بمادة رابع كلوريد الكربون في الجرذان .قسمت الجرذان إلى خمس مجموعات :مجموعة أعطيت المذيب ومجموعة أعطيت رابع كلوريد الكربون فقط وأعطيت المجموعات الثالث المتبقية رابع كلوريد الكربون مع إعطاء مجموعة منهم النيكورانديل والثانية أعطيت الجاليبنكالميد والثالثة أعطيت النيكورانديل والجاليبنكالميد معا ً .وقد اتضح تأثير النيكورانديل الواقي على الكبد من خالل النقص الواضح في نشاط إنزيم األالنين أمينوترانسفيريز واألسبارتات أمينوترانسفيريز في مصل الدم ،وكذلك نقص معدل الدهون الثالثية في الكبد والكوليستيرول الكلي وأكسيد النيتريك ومحتوى الكبد من نواتج تأكسد الدهون (المالون ثنائي األلدهيد) ،باإلضافة إلى زيادة تركيز األلبيومين في مصل الدم وزيادة نشاط إنزيم الكتاليز في الكبد مقارنة بالمجموعة التي أعطيت رابع كلوريد الكربون فقط .وقد أ ُ ّكدَت التأثيرات الوقائية للنيكورانديل بتحليل أنسجة الكبد .ومما يسترعي االنتباه أن تأثيرات النيكورانديل الواقية للكبد قد بقيت حتى في وجود الجاليبنكالميد .ونخلص من ذلك كله بأن النيكورانديل له تاثير وقائي على الكبد ضد التسمم الكبدي المستحدث برابع كلوريد الكربون ،وأن هذا التأثير قد يُعزى بشكل جزئي إلى خصائص النيكورانديل المانعة للتأكسد وليس إلى تحفيز قنوات البوتاسيوم الحساسة لألدينوسين ثالثي الفوسفات. 323