COMORBIDITY 2009 - addictioneducation.co.uk
advertisement

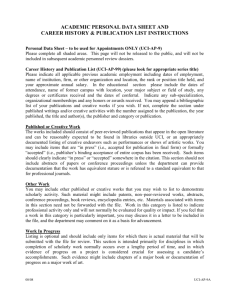
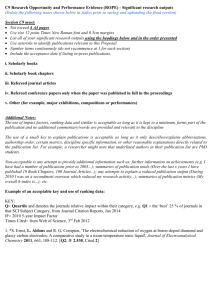
COMORBIDITY 2009 <777> Database EMBASE Accession Number 0019828034 Authors Dausey D.J. Pincus H.A. Herrell J.M. Institution (Dausey) Carnegie Mellon University, Pittsburgh PA 15213, United States. (Dausey, Pincus) RAND Corporation, Pittsburgh PA 15213, United States. (Pincus) College of Physicians and Surgeons, Columbia University, New York Presbyterian Hospital and Irving Center for Clinical and Translational Research, New York NY 10032, United States. (Herrell) Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Substance Abuse Treatment (CSAT), Rockville, MD 20850, United States. Country of Publication United Kingdom Title Performance measurement for co-occurring mental health and substance use disorders. Source Substance Abuse: Treatment, Prevention, and Policy. 4(pp 18), 2009. Article Number: 1747. Date of Publication: 14 Oct 2009. Publisher BioMed Central Ltd. Abstract Background: Co-occurring mental health and substance use disorders (COD) are the norm rather than the exception. It is therefore critical that performance measures are developed to assess the quality of care for individuals with COD irrespective of whether they seek care in mental health systems or substance abuse systems or both. Methods: We convened an expert panel and asked them to rate a series of structure, process, and outcomes measures for COD using a structured evaluation tool with domains for importance, usefulness, validity, and practicality. Results: We chose twelve measures that demonstrated promise for future pilot testing and refinement. The criteria that we applied to select these measures included: balance across structure, process, and outcome measures, quantitative ratings from the panelists, narrative comments from the panelists, and evidence the measure had been tested in a similar form elsewhere. Conclusion: To be successful performance measures need to be developed in such a way that they align with needs of administrators and providers. Policymakers need to work with all stakeholders to establish a concrete agenda for developing, piloting and implementing performance measures that include COD. Future research could begin to consider strategies that increase our ability to use administrative coding in mental health and substance use disorder systems to efficiently capture quality relevant clinical data. copyright 2009 Dausey et al; licensee BioMed Central Ltd. Publication Type Journal: Article Journal Name Substance Abuse: Treatment, Prevention, and Policy Volume 4 Page 18 Year of Publication 2009 Date of Publication 14 Oct 2009 COMORBIDITY 2009 <801> Database EMBASE Accession Number 0019813108 Authors Schneider B. Institution (Schneider) Center of Psychiatry, Department for Psychiatry, Psychosomatics, and Psychotherapy, GoetheUniversity, Heinrich-Hoffmann-Str. 10, 60528 Frankfurt, Germany. Country of Publication United Kingdom Title Substance use disorders and risk for completed suicide. Source Archives of Suicide Research. 13(4)(pp 303-316), 2009. Date of Publication: October 2009. Publisher Routledge Abstract Substance use disorders are among the most frequent psychiatric disorders found in suicides. In psychological autopsy studies between 19% and 63% of all suicides suffered from substance use disorders, mostly from alcohol use disorders. Suicide risk is highly increased in substance use disorders, particularly in alcohol use disorders, and in co-morbid alcoholism and depression. So far, some risk factors for suicide have been identified in alcoholism. Nevertheless, various questions about the relationship between substance use disorders and suicide remain open, which indicate directions for future research. copyright International Academy for Suicide Research. ISSN 1381-1118 Publication Type Journal: Article Journal Name Archives of Suicide Research Volume 13 Issue Part 4 Page 303-316 Year of Publication 2009 Date of Publication October 2009 COMORBIDITY 2009 <802> Database EMBASE Accession Number 0019813114 Authors van Tuan N. Dalman C. Thiem N.V. Nghi T.V. Allebeck P. Institution (van Tuan, Dalman, Allebeck) Department of Public Health Sciences, Karolinska Institute, Stockholm, Sweden. (van Tuan, Thiem, Nghi) Department of Psychiatry, Hanoi Medical University, Hanoi, Vietnam. (van Tuan, Thiem, Nghi) National Institute of Mental Health, Hanoi, Vietnam. Country of Publication United Kingdom Title Suicide attempts by poisoning in Hanoi, Vietnam: Methods used, mental problems, and history of mental health care. Source Archives of Suicide Research. 13(4)(pp 368-377), 2009. Date of Publication: October 2009. Publisher Routledge Abstract The objective of this paper was to investigate methods of poisoning, presence of mental problems, and the rate of psychiatric care among suicide attempters in Vietnam. Three hundred and nine suicide attempters by poisoning admitted to Bach Mai Hospital's Poison Control Center were investigated by trained nurses and qualified psychiatrists. Standardized questionnaires were used to assess methods of suicide, presence of mental problems, and psychiatric care. The most common methods were poisoning by psychotropic drugs in urban, and pesticides in rural areas. ICD-10 confirmed disorders were present in 68% of the cases and 73% rated positive on SRQ-20. Most patients were not in contact with psychiatric care. Restrictions on availability and handling of drugs and pesticides should be reinforced. Better infrastructures are needed for identification and treatment of persons with mental disorders. copyright International Academy for Suicide Research. ISSN 1381-1118 Publication Type Journal: Article Journal Name Archives of Suicide Research Volume 13 Issue Part 4 Page 368-377 Year of Publication 2009 Date of Publication October 2009 COMORBIDITY 2009 <925> Database EMBASE Accession Number 0019401946 Authors Nery-Fernandes F. Quarantini L.C. Galvao-De-Almeida A. Rocha M.V. Kapczinski F. Miranda-Scippa A. Institution (Nery-Fernandes, Quarantini, Galvao-De-Almeida, Rocha, Kapczinski, Miranda-Scippa) Center for Study and Treatment of Affective Disorders (CETTA), Universidade Federal da Bahia, Salvador-Ba, Brazil. Country of Publication United Kingdom Title Lower rates of comorbidities in euthymic bipolar patients.. Source The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry. 10(4 Pt 2)(pp 474-479), 2009. Date of Publication: 2009. Abstract OBJECTIVE: This study assessed the frequency of axis I psychiatric comorbidities in euthymic bipolar patients and the clinical differences between patients with and without comorbidities. METHOD: In this study, 62 euthymic bipolar outpatients assessed using a clinical questionnaire underwent a structured diagnostic interview (SCID/CV-DSM-IV) as well as a symptoms evaluation (YMRS and HAM-D-17). RESULTS: The lifetime frequency of patients with comorbidities was 27.4%. The most frequent comorbidities were anxiety disorders (33.7%), and the positive associated variables were more advanced age, the presence of a steady partner, a first episode of the depressive type and lifetime attempted suicide. CONCLUSIONS: The lower frequency of comorbidities found in our study in comparison with those described in the literature may be due to the evaluation restricted only to euthymic patients. This suggests the importance of assessing psychiatric comorbidity in bipolar individuals while not in acute phases of the disorder. Publication Type Journal: Article Journal Name The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry Volume 10 Issue Part 4 Pt 2 Page 474-479 Year of Publication 2009 Date of Publication 2009 COMORBIDITY 2009 <926> Database EMBASE Accession Number 0017853283 Authors Sorensen H.J. Mortensen E.L. Reinisch J.M. Mednick S.A. Institution (Sorensen, Mortensen, Reinisch, Mednick) Danish Epidemiology Science Center, Institute of Preventive Medicine, Copenhagen University Hospital, Copenhagen, Denmark. Country of Publication United Kingdom Title Parental psychiatric hospitalisation and offspring schizophrenia.. Source The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry. 10(4 Pt 2)(pp 571-575), 2009. Date of Publication: 2009. Abstract The risk of schizophrenia has been linked with a family history of schizophrenia and less strongly with other psychiatric disorders in family members. Using data from the Copenhagen Perinatal Cohort and from the Danish Psychiatric Case Register, we studied the relationship between offspring risk of schizophrenia and a range of psychotic and non-psychotic psychiatric diagnoses in parents. Psychiatric admission data after 1969 were available for 7047 cohort members born between 1959 and 1961, and for 7006 mothers and 6993 fathers. Univariate analysis showed that neurosis, alcohol and substance dependence in both parents were associated with elevated risk of offspring schizophrenia; in addition, maternal schizophrenia, affective disorder and personality disorder were associated with elevated risk. Controlling for parental age, parental social status, and parental psychiatric co-diagnosis, offspring risk of schizophrenia was associated with maternal schizophrenia (OR = 15.41 with 95% CI 5.96-39.81) and, independently, with paternal hospitalisation with neurosis (OR = 5.90 with 95% CI 2.23-15.62). The risk of schizophrenia associated with paternal neurosis remained significant after excluding offspring of parents with non-affective psychosis from the sample. These findings suggest that genetic and family studies should not only focus on parental history of schizophrenia since the simple distinction between positive and negative family history could not accurately describe offspring risk in this sample. Publication Type Journal: Article Journal Name The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry Volume 10 Issue Part 4 Pt 2 Page 571-575 Year of Publication 2009 Date of Publication 2009 COMORBIDITY 2009 <949> Database EMBASE Accession Number 0019658047 Authors Novak G. Boukhadra J. Shaikh S.A. Kennedy J.L. Le Foll B. Institution (Novak, Boukhadra, Shaikh, Kennedy, Le Foll) Translational Addiction Research Laboratory, Centre for Addiction and Mental Health and The University of Toronto, Toronto, Ontario, Canada. Country of Publication United Kingdom Title Association of a polymorphism in the NRXN3 gene with the degree of smoking in schizophrenia: a preliminary study. Source The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry. 10(4 Pt 3)(pp 929-935), 2009. Date of Publication: 2009. Abstract Whole genome scan studies have recently identified the NRXN1 and NRXN3 genes as potential contributing factors in the risk for nicotine addiction. We have genotyped 15 single nucleotide polymorphisms (SNPs) spanning the NRXN1 and NRXN3 genes in 195 unrelated patients with schizophrenia for whom information about their smoking status and number of cigarettes smoked per day (CPD) was obtained. The NRXN3 marker rs1004212 was significantly associated with quantity of tobacco smoked. Individuals homozygous for the C allele of rs1004212 smoked more cigarettes per day than heterozygous individuals. We found no significant association of markers within the NRXN1 gene with the risk of smoking or the quantity of tobacco smoked. Because of the relatively small sample size, this is a preliminary study. However, this candidate gene study supports the observations of molecular studies implicating the NRXN genes in drug addiction and suggests that variants in the NRXN3 gene could contribute to the degree of nicotine dependence in patients with schizophrenia. Publication Type Journal: Article Journal Name The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry Volume 10 Issue Part 4 Pt 3 Page 929-935 Year of Publication 2009 Date of Publication 2009 COMORBIDITY 2009 <950> Database EMBASE Accession Number 0018609413 Authors Fontenelle L.F. Mendlowicz M.V. Versiani M. Institution (Fontenelle, Mendlowicz, Versiani) Anxiety and Depression Research Program, Institute of Psychiatry, Universidade Federal do Rio de Janeiro (IPUB/UFRJ), Rio de Janeiro, RJ, Brazil. Country of Publication United Kingdom Title Volitional disorders: a proposal for DSM-V.. Source The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry. 10(4 Pt 3)(pp 1016-1029), 2009. Date of Publication: 2009. Abstract In the DSM-IV-TR, specific impulse control disorders not elsewhere classified (ICD) have been designated following four principles: (1) through the addition of an adjective that emphasizes the aberrant character of an otherwise normal behaviour (e.g., pathological gambling); (2) by means of metaphors (such as in intermittent explosive disorder); (3) according to the presumably quintessential nature of their main signs and symptoms, such as impulsive (e.g., impulse control disorders not elsewhere classified), compulsive (e.g., compulsive shopping), or addictive (e.g., internet addiction); or (4) using Greek suffix mania (e.g., kleptomania, pyromania, and trichotillomania). Given this flagrant inconsistency, we argue that time has come to adopt a less arbitrary way of describing these disorders, at least until it becomes clearer whether they are really impulsive, compulsive or addictive or if the preoccupation with this distinction is valid. In keeping with DSM's emphasis on descriptive phenomenology rather than on unsupported theory, a less biased terminology is in order. Therefore, we would like to suggest: (1) the substitution of the term ICD by the more neutral expression 'volitional disorders not elsewhere classified'; (2) the use of the classical Greek suffix mania, already present in some DSM-IV-TR ICDs, as the main naming principle to be adopted in the DSM-V; and (3) the creation of compulsive, impulsive, and mixed subtypes of the 'volitional disorders not elsewhere classified', since they are beginning to be validated by treatment trials. Publication Type Journal: Review Journal Name The world journal of biological psychiatry : the official journal of the World Federation of Societies of Biological Psychiatry Volume 10 Issue Part 4 Pt 3 Page 1016-1029 Year of Publication 2009 Date of Publication 2009 COMORBIDITY 2009 <970> Database EMBASE Accession Number 0020021664 Authors Shi L. Ascher-Svanum H. Chiang Y.J. Zhao Y. Fonseca V. Winstead D. Institution (Shi, Ascher-Svanum, Chiang, Zhao, Fonseca, Winstead) School of Public Health and Tropical Medicine, Tulane University, 1440 Canal Street, New Orleans, LA 70112, USA. Country of Publication United Kingdom Title Predictors of metabolic monitoring among schizophrenia patients with a new episode of second-generation antipsychotic use in the Veterans Health Administration.. Source BMC psychiatry. 9(pp 80), 2009. Date of Publication: 2009. Abstract BACKGROUND: To examine the baseline metabolic monitoring (MetMon) for second generation antipsychotics (SGA) among patients with schizophrenia in the Veterans Integrated Service Network (VISN) 16 of the Veterans Health Administration (VHA). METHODS: VISN16 electronic medical records for 10/2002-08/2005 were used to identify patients with schizophrenia who received a new episode of SGA treatment after 10/2003, in which the VISN 16 baseline MetMon program was implemented. Patients who underwent MetMon (MetMon+: either blood glucose or lipid testing records) were compared with patients who did not (MetMon-), on patient characteristics and resource utilization in the year prior to index treatment episode. A parsimonious logistic regression was used to identify predictors for MetMon+ with adjusted odds ratios (OR) and 95% confidence intervals (CI). RESULTS: Out of 4,709 patients, 3,568 (75.8%) underwent the baseline MetMon. Compared with the MetMon- group, the MetMon+ patients were found more likely to have baseline diagnoses or mediations for diabetes (OR [CI]: 2.336 [1.846-2.955]), dyslipidemia (2.439 [2.029-2.932]), and hypertension (1.497 [1.287-1.743]), substance use disorders (1.460 [1.257-1.696]), or to be recorded as obesity (2.052 [1.724-2.443]). Increased likelihood for monitoring were positively associated with number of antipsychotics during the previous year (FGA: 1.434 [1.129-1.821]; SGA: 1.503 [1.290-1.751]). Other significant predictors for monitoring were more augmentation episodes (1.580 [1.145-2.179]), more outpatient visits (1.007 [1.0021.013])), hospitalization days (1.011 [1.007-1.015]), and longer duration of antipsychotic use (1.001 [1.001-1.001]). Among the MetMon+ group, approximately 38.9% patient had metabolic syndrome. DISCUSSION: This wide time window of 180 days, although congruent with the VHA guidelines for the baseline MetMon process, needs to be re-evaluated and narrowed down, so that optimally the monitoring event occurs at the time of receiving a new episode of SGA treatment. Future research will examine whether or not patients prescribed an SGA are assessed for metabolic syndrome following the index episode of antipsychotic therapy, and whether or not such baseline and follow-up monitoring programs in routine care are cost-effective. CONCLUSION: The baseline MetMon has been performed for a majority of the VISN 16 patients with schizophrenia prior to index SGA over the study period. Compared with MetMon- group, MetMon+ patients were more likely to be obese and manifest a more severe illness profile. Publication Type Journal: Article Journal Name BMC psychiatry Volume 9 Page 80 Year of Publication 2009 Date of Publication 2009