Vascular Endothelial Growth Factor Gene Therapy
advertisement

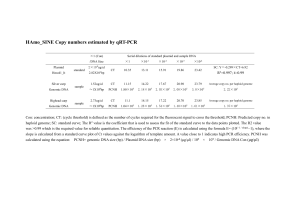
Title: Vascular Endothelial Growth Factor Gene Therapy Enhances Survival of Ischemic Random Skin Flaps in the Rats Authors: Liwen Yang, M.D., Jixiang Zhang, M.D., Ph.D., Li Zeng, M.D., Jiangjing Xu, B.S., Fangten Du, M.D., Wen Luo, M.D., Zhongjin Luo, M.D., and Jianhong Jiang, B.S. Plastic and reconstructive surgery has recently given attention to the focus that the viability of the ischemic tissues can be increased by gene therapy. Ischemic skeletal muscle has been shown to be advantageous for taking up and expressing foreign genes transferred in the form of naked plasmid DNA. We therefore investigated the effects of the naked plasmid DNA encoding vascular endothelial growth factor (VEGF) injected directly into the panniculus carnosis muscle on survival of a full thickness ischemic random skin flap in the rat. Method: A random skin flap measuring 8 cm by 2 cm was elevated onto the back of each of 30 Sprague-Dawley rats. All 30 rats were randomized into three groups with 10 in each group. The rats in experimental group were treated with the naked plasmid DNA encoding 121-amino acid isoform of VEGF that was inserted into pcD2. The rats in other two control groups were administrated with control plasmid DNA alone or physiologic saline. Each solution was injected directly into the panniculus carnosis muscle of the ischemic skin flap. At seven days after injection, RT-PCR, immunohistochemistry, single photon emission computed tomography , and color medical image analytical system were employed to investigate the expression of VEGF, the blood flow, the subdermic vascular density, and the survival rate of the ischemic skin flap. Results: Notably increased expressions of VEGF mRNA and the corresponding protein were found in the flaps treated with the naked VEGF plasmid DNA. The blood supply to the flap and the subdermic vascular density were markedly increased in the VEGF gene-treated group than either of the two control groups (P﹤0.01). Compared with the two control groups, the ischemic skin flap treated with VEGF plasmid DNA showed a significant enhanced tissue viability at the end of 7 days after treatment: 87﹢/﹣5 % versus 47﹢/﹣6 % for the control plasmid pcD2 group (P﹤0.01), or versus 46﹢/﹣5% for the saline group (P﹤0.01). Conclusion: Our results indicated that the VEGF gene therapy is able to enhance survival of ischemic skin flap by inducing angiogenesis and increasing vascular perfusion. We also conformed that the panniculus carnosis muscle is capable of taking up and expressing foreign gene transferred by direct intramuscular injection of naked VEGF plasmid DNA in a rat model of ischemic skin flap. Correspondence to: Dr J X Zhang, Molecular Medicine Institute, The Second Affiliated Hospital, Jiangxi Medical College, 1 Mingde Road Nanchang City, Jiangxi Province, 330006, CHINA. Email: shangrao3@yahoo.com