Placement report Ms F Alezuyo - Butabika
advertisement

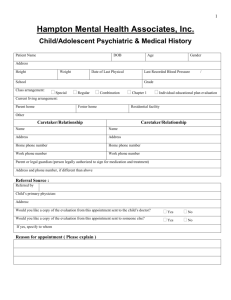
INTRODUCTION Although mental health services in Uganda have rapidly improved in the recent 5-6 years, child and adolescent mental health remained a very big challenge due to lack of special attention to this branch of psychiatry. The country with a population of about 31 million people, had one child and adolescent psychiatrist (now retired) who was based in Kampala and unable to reach out to the whole population. And this was also worsened by children and adolescents with mental health problems been admitted and nursed among adults in the only National Psychiatric Hospital Butabika in the country. Though mental health serves are been offered in regional hospitals, no special attention had been paid to child and adolescent mental health services However, a day children’s unit was opened in Butabika (The National referral Mental Hospital) in 2006 by mental health professionals from East London and in 2010 an inpatient ward was opened. The East London trust in conjunction with Commonwealth developed a strategy to develop specialised child and adolescent mental services to Uganda by training two doctors, one psychiatric clinical officer and two nurses from UK who will be trainers of other health professional in child and adolescent psychiatry. Objectives To gain knowledge and skills in: 1. Individualised patient care 2. Psychiatric diagnosis and/ or psychological problem identification 3. Use of medication, as and when required In order to achieve the above objectives, I had a two months placement at Coborn Centre for Adolescents which is an in-patient unit with a bed capacity of 12 in Acute ward and 3 in the Intensive Care unit and it also has day care services. During my placement at Coborn, I learnt how patients are assessed, either on admission to hospital or at review meetings in the hospital and how it differs from how assessments and care-plans are implemented in Uganda. How care-plans are designed and implemented for each patient according to their individual psychiatric, psychological, emotional and behavioural needs, at each stage of their care. How wards are managed, day services are programmed, school routines are therapeutically programmed to promote the patients recovery. This was done through different therapeutic approaches to care management by a good multi-disciplinary team, care-programme approach to care plans, assessment and treatment models according to each multi-disciplinary team, psychiatric emergencies, nursing care plan, evaluation and documentary To achieve these objectives, I had to review, reflect on how some of these skills, techniques or structures might be applicable or adapted to the children’s unit and outpatient clinics at Butabika. And also review and reflect on how to do this in practice, at Butabika, in relation to the challenges, constraints and possible limitations, who to talk to, or to work alongside with in order to implement the knowledge and skills that I have acquired. Lessons learnt From the above objectives, I have gained a reflective understanding of the journey young people make through the acute phase of the illness, psychiatric intensive care and day-patient services. This is done through individualised care, care plan assessments meetings, involvement of the families/ care takers in every step of care the young person goes through and with the full consent of the parents/caretakers unlike in Uganda where we have no care plan meetings and no structured care plan for the young people. In Butabika, involvement of the parents/ caretakers depends on their availability as a result we at times treat and discharge the young person without interacting with the parents/caretakers. This is due to the poor referral system we have in Uganda making it difficult to trace the young person’s family until after recovery as the young person could have been abandoned near the hospital compound as child protection services are also poor in Uganda unlike in UK where child protection is a very sensitive matter and in case of any suspicion of child abuse, social services does thorough investigations. I observed how psychiatric assessments are done by psychiatrists and SHOs on admission, it aims at getting a psychiatric diagnosis and possibly use of medication. The assessment doesn’t differ so much from what we do in Uganda, but with medication in UK, there’s minimal use of medication and very low doses which is discussed during ward rounds and hand over meetings. I also noticed the use of atypical anti-psychotics in very low doses unlike in Uganda we use typical antipsychotics, very high doses and young people end up with extrapyramidal sides. I gained a good understanding of how the multi-disciplinary team works together and how each professional has a specific part to play, which contributes to the whole functioning of the service and individual young person’s care management. This was done through the different approaches to care and therapeutic management which include Care programme approach (CPA) Assessment and treatment models according to each multi-disciplinary team Psychiatric emergencies Nursing care plans, evaluation and documentation Care-plan and implementation from other disciplines including psychiatrists, psychologists, occupational therapists, teachers, and family, therapists work and differ from each other. Experience at Child and Family Consultation Services at York House At York house, community Child and Adolescent Mental Health Services (CAMHS) are been offered by a well and specialised multi-disciplinary team. They do mental health assessment and identify emotional and behavioural problems affecting children and their families, and how the families, schools and communities have contributed either positively or negatively to the development of this behaviour and how the different stakeholders can be supported to help the young person either deal with or cope with it. They work hand in hand with the different schools, families, social service, GPs and the young persons. They support the family through taking therapy unlike in Uganda where taking therapy is not much practised leading to use of medication when at times is not necessary. In my placement at York House, I never witnessed use of medication and the service users seem to be happy with it. The different multi-disciplinary team have sub-groups, depending on their speciality where they sit for filter and feedback meetings in order to allocate new cases, give feedback on the young persons they have been following and close cases Conference and workshops I attended four major conferences and two workshops organised by Association of child and Adolescent Mental Health (ACAMH) on: Child and adolescent learning disabilities Mental Health problems affecting asylum seeking children Preventing mental health problems through very early intervention Cognitive behavioural therapy (CBT) across cultures During the conferences, I learnt that when mental health problems are prevented or identified early in children, problems like learning disabilities, emotional and behavioural problems would be minimised and the number of adults with psychosis or mental health problems would be very low. I also learnt children present with emotional and behavioural problems after having physical, psychological and sexual which is inflicted on them by adults, however, when they can no longer take it, then it’s seen in their behaviour. They sometimes witness things that they find very scary or stressful, they react by either fight or flight (fight by becoming child soldiers or flight by seeking asylum) during which they go through many stressful events like sleeping in the wilderness, feeling hungry, being physically and sexually abused and they later present with different mental health problems which need intervention by mental health workers. Uganda, having been in war for 20 years has children who were born during the war and have never known what peace is like, they present with traumatic memories. They may present with anger, sadness, guilt, horror, confusion and at times they may present with psychosis and lack of trust for adults. As a result l feel taking therapy would be the best for such depending on how they present. Children who grow were there’s domestic violence, parents abuse drugs, unstable relationships may end up with learning difficulties, emotional and behavioural problems. It may seem reasonable to expect early identification of problems in childhood to be straight forward process but in practice, quite not been the case. While some cases are not easily identified especially emotional abuse but physical abuse can easily be identified as a result, there’s need to provide conducive environment for children. This can be done through health education to parents and care takers on causes of mental health problems, need for early intervention good child protection services, and integration of mental health into Primary Health Care Services, which we have started doing in our daily mental health care delivery in Uganda. Implementation A good child and adolescent mental health service can be delivered in Uganda, this can be done through: Specialists in child and adolescent mental health to train mental health workers and other health professionals in how to identify, assess, and prevent mental health problems. Butabika, Mbarara and Mulago being teaching hospitals, NHS has trained two doctors, two nurses and one psychiatric clinical officer strategically from this hospitals in child and adolescent mental health services, and we plan to work as a team to implement it. Planning structured programme for young people right from the time of admission to time of discharge in order to promote their recovery, and need to use more talking therapy than high doses of drugs There’s need for individualised care as young people present differently with different problems as a result there is need for care plan assessment for each young person I also realised it is very important to involve parents/caretakers in the care of the young people as they go through their journey from the acute phase to day care service Prevention of mental health problems through very early intervention is a very good measure. As a preventive measure, it will be necessary to make the public aware of factors that can cause mental illness and mental health issues and aware of possible ways of preventing them. In Uganda, we have been trying to do this through health education to the communities but at times it is complicated by cultural issues, as a result, Ministry of Health has encourage health workers to work with traditional healers to reach to the communities. Challenges The ratios of patients to health care-providers is too high leading to healthcare providers not having enough time with the young persons individually The numbers of patients with epilepsy and learning disability outnumber the number of people with mental health problems Lack of specialists in Child and Adolescent mental health with inadequate multi-disciplinary team leading to professionals being exhausted Poor referral system leading to waste of time assessing patients who don’t need mental health services, and this leads to overwhelming number of patients. Also due to the poor referral system young people are at times abandoned on the hospital compound by relative/ caretakers or brought in after been found by police loitering in towns and such patients at times fail to trace their homes leading to congestion on the ward Mental health services delivery in Uganda are at times affected by cultural issues which makes people seek mental health services late, hence, delaying. Due to poor resources, reaching out to the people who need services becomes difficult Way forward There’s need to open a school for nurse, psychiatric clinical officers, occupational therapists to specialist in child and adolescent psychiatry. This is already in progress and we have just finished the draft syllabus with the support from NHS Butabika link Training all health professionals with knowledge, skills in identification, assessment, prevention and management of mental health problems Need to actively involve parents/caretakers in the care of the young persons with mental health problems To work with the hospital administration in order to implement good child and adolescent mental health service delivery by designing a good referral system especially for children and adolescents There is need to start Uganda Association of Child and Adolescent Mental Health in order to share with other professionals and improve services in Butabika in particular and Uganda in general. Summary Mental health problems can be prevented or minimised if there is early intervention. And identifying mental health problems in children and adolescents can reduce the prevalence in adults. In Uganda, child and adolescent mental health remained a challenge due to no special attention was paid to it. With the training of specialists in this field of psychiatry by NHS East London, child and adolescent services in Uganda will improve.