Epithelial Tissue
advertisement
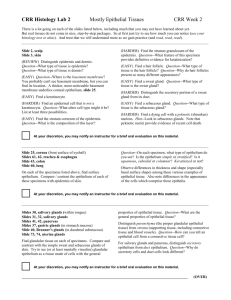
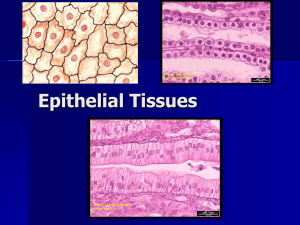
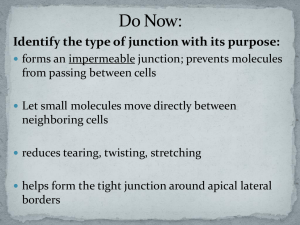
Epithelial Tissue August 26, 2010 Dr. Crissman 1. Identify the two major subdivisions of epithelium (epithelium and glands) and their embryological origins. a. Ectoderm: epidermis b. Mesoderm: lining of internal cavities i. Mesothelium: pericardium, pleura, peritoneum ii. Endothelium: Lining of blood/lymph vessels c. Endoderm: Lining of GI, respiratory tract 2. Be able to define tissue epithelium, list its functions and common structural characteristics a. Epithelium: Layer of cells that cover the body’s surfaces b. Functions of Epithelium: i. Physical barrier ii. Protection from chemical/mechanical damage and dehydration iii. Secretion (glands are epithelial tissue) iv. Absorption (GI) v. Transport (endothelium, lungs) vi. Sensory surfaces vii. Regeneration and repair c. Structural characteristics of epithelium: i. Predominantly cellular ii. Numerous intercellular junctions iii. Polar cell (Apical vs. Basolateral portions) iv. Free surface v. Sits on basement membrane of connective tissue vi. Avascular 3. Be able to describe and classify types of epithelium by cell shape and number of layers a. Two parts to epithelium naming, according to STRUCTURE i. Number of layers 1. Unilaminar = Simple (single layer) 2. Multilaminar = Stratified (more than 1 layer) ii. Shape of cell 1. Squamous – thin and flat 2. Cuboidal – cube-like 3. Columnar – Tall & Narrow b. Types of Epithelial Tissues (based on shape of surface cells!) i. Simple Squamous: Lining of blood/lymph vessels ii. Simple Cuboidal: Ducts of glands, ovary covering iii. Simple Columnar: GI tract, lower respiratory tract iv. Pseudostratifed: Most of respiratory tract, nasal cavity v. Keratinized Stratified Squamous: 1. NO nucleus. Cell dies as it migrates up 2. Epidermis vi. Non-keratinized Stratified Squamous (mucosa): 1. Nucleus present 2. Wet inner surfaces (vagina, mouth, eye, esophagus) vii. Stratified Cuboidal: Ducts of sweat glands, pancreas viii. Transitional (Uroepithelium) Epithelial Tissue August 26, 2010 Dr. Crissman 1. Most of urinary tract 2. Non-distended Uroepithelium: Surface = Cuboidal 3. Distended Uroepithelial: Surface = Squamous ix. Sensory 1. Gustatory: Tongue, taste buds 2. Olfactory: Nasal passage 3. Stato-acustic: ears (proprioception) x. Germinal: seminiferous tubules 4. Be able to describe the polarity of the epithelial membrane and how its specializations contribute to its polarity and function. Be able to relate structure to function a. Epithelial cells are morphologically divided into Apical and Basolateral domains, each with its own structural/functional characteristics b. Apical Domains i. Free surface (luminal) side of cell ii. Contains: Carrier proteins, Glycoproteins, Glycocalyx, Hydrolytic enzymes, Aquaporins iii. Performs Endocytosis, Exocytosis, and Transcytosis 1. Endocytosis: Coated pit with clathrin pinched off, forms coated vesicle which becomes endosome by shedding clathrin 2. Exocytosis: At apical surface (mucous, saliva) or basolateral surface (endocrine glands) 3. Transcytosis: One side to another in any direction iv. Specializations of Apical Surface 1. Microvilli: small, non-motile finger-like projections a. Form striated, brush-border b. Actin filaments joined at top of microvilli (Villin), connected to each other (Fimbrin), embedded at base (into Terminal web), and supported by linkages to membrane at regular intervals (myosin-1, calmodulin) c. GI tract, Proximal tubule of kidney 2. Sterocilia: longer version of microvilli, non-motile, epididymis 3. Cilia a. Motile, used to propel mucous across surface b. Axoneme: core of cilia c. Consist of microtubules attached to basal body at bottom d. 2 singlets surrounded by 9 doublets (made of Subunit A of 13 protofilaments, and Subunit B of 10 protofilaments): 9+2 Arrangement e. Sheath surrounds singlet’s and is connected to Subunit A by radial spoke to prevent buckling f. Nexin connects neighboring doublets g. Dynein is microtuble-associated protein with 2 arms which project from Subunit A to B. Epithelial Tissue August 26, 2010 Dr. Crissman Dynein ATPase causes dynein to transiently attach to Subunit B and slide toward tip and cilium. Nexin translates this to bending. Dynein releases Subunit B, causing cilia to return upright h. Beat of cilia has Effector Stroke and Recovery stroke i. Primary Ciliary Dyskinesia or Immotile Cilia Syndrome or Kartagener’s Syndrome: lacking dynein or radial spokes, leading to malfunction cilia (infertility, lung infections) 4. Flagella a. Structurally similar to cilia, but longer and axoneme is surrounded by mitochondria c. Basolateral Domain i. Lateral and base of epithelial cell ii. Characterized by junctional complex, aka terminal bars, which is where cells come in contact near apical surface and runs all around the cell’s circumference iii. 4 Different Structural/Functional Junctions of Lateral Domain 1. Zonula Occludens aka Tight Junction a. Most superficial to apical surface b. Quilt-like barrier which functions to make epithelial sheet impermeable to substances. Tight vs. Leaky c. Division of apical/basolateral membranes, and keeps membrane proteins from each domain separate d. Fusion of claudin and occludin, arranged as anastomosing strands, and reinforced by Cadherins 2. Zonula Adherens aka Adhesion Belt a. Mechanical adhesion between neighboring cells b. Cadherins are transmembrane linker proteins, and are bound to Actin filaments of cytoskeleton by Talin, Vinculin, and -Actin. 3. Macula Adherens aka Desmosome a. Act as a “spot-weld” mechanical attachment b. Attachment Plaques (made of desmoplakin & plakoglobin) formed on cytoplasmic side of membrane c. Desmoglein & Desmocolin (both Cadherins) span membrane/gap to connect plaques d. Intermediate filaments anchor plaques into membrane e. Phemphigus vulgaris: antibodies attack self cadherins (desmoglein). Causes severe blistering due to high [desmosome] in epidermis Epithelial Tissue August 26, 2010 Dr. Crissman 4. Gap Junctions a. Only in lateral domain, scattered throughout b. Cell-cell communication c. Disc of numerous connexons (total of 6 connexin subunits) form aqueous pores in cell membrane which connect cytoplasm of adjacent cells d. Passable ONLY to ions, small amino-acids, c-AMP, nucleotides and polysaccharides (i.e. no macromolecules) e. Can pass along electrical impulse to create peristaltic wave iv. 3 Specializations of Basal Domain: 1. Basal Lamina: Dense layer which holds cell to connective tissue; located in ECM, subadjacent to basal membrane 2. Plasma Membrane Enfoldings: highly folded basal membrane which increases surface area for fluid passage (tessellated). 3. Hemidesmosomes: Appears as half of a desmosome and has ½ plaque on cytoplamsic side into which Intermediate Filaments embed. Unlike Desmosomes, transmembrane protein is Integrin, which holds cell membrane to basement membrane i.e. connective tissue. 5. Describe/differentiate between exocrine and endocrine glands a. Endocrine Gland: No duct. Secretes directly into connective tissue where it is transferred into blood b. Exocrine Gland: Uses duct to deliver secretion to surface of epithelium 6. Be able to describe common components of an exocrine gland and classify glands by morphology, mode of secretion, and type of secretion a. Morphological/Structural Classification i. Unicellular gland: single cell embedded in epithelial layer (ex. Goblet cell) ii. Multicellular Gland: consists of duct and secretory portions and is named according to 1.) Branching of duct portion and 2.) Shape of secretory portion 1. Duct Portion: branching-based a. Simple exocrine gland: single duct b. Compound exocrine gland: branched duct system 2. Secretory Portion: shape-based a. Tubular: Secretory portion forms long tube b. Acinar/Alveolar: Secretory portion is grape-shaped, may have myoepithelial cells surrounding secretory portion, contractile to help secretion 3. Multicellular glands are surrounded by Connective Tissue Capsule 4. Larger versions may be subdivided by septa Epithelial Tissue August 26, 2010 Dr. Crissman iii. Examples of structural nomenclature: 1. Simple tubular: Gastric glands 2. Simple alveolar: Sebaceous glands 3. Simple branched alveolar: Sebaceous glands 4. Simple coiled tubular: Sweat glands 5. Compound tubuloaveolar: Salivary, pancreas b. Mode of Secretion i. Merocrine secretion 1. Most common 2. Exocytosis of secretory vesicles, no cytoplasm loss 3. Sweat, saliva, pancreas, goblet cells ii. Apocrine secretion 1. Secretion is pinched off of cell with partial cytoplasm and membrane loss 2. Lipid portion of milk of mammary gland iii. Holocrine secretion 1. Cell fills with secretion and dies, degeneration cell forms secretion 2. Sebaceous gland of skin iv. Cytocrine secretion 1. Whole living cell is secreted 2. Ovary, testis c. Type of Secretion i. Mucous 1. Thick, viscous, and rich in mucinogens 2. Appears as light-staining with foamy cytoplasm 3. Ex. Goblet cells, sublingual salivary ii. Serous 1. Watery and rich in enzymes and ions 2. Cells appear acidophilic (darker) 3. Ex. pancreas, parotid, sweat glands iii. Mixed 1. Both mucous and serous secretions 2. Demilunes: crescent shapes on outside of mucous alveolus 3. Ex: salivary gland iv. Sebum 1. Oily, rich in lipid 2. Ex. Sebaceous glands of skin, eyelid v. Ceruminous 1. Thick, waxy, protective secreation 2. Ex. Glands of auditory canal 7. Be able to define and describe the different levels of organization in the body a. Cells: Basic unit of all animals b. Tissues: groups of cells performing a specific function c. Organs: groups of tissues performing specific function d. Organ Systems: Groups of organs performing specific function 8. Be able to list and describe the 4 tissue types in the body. Epithelial Tissue August 26, 2010 Dr. Crissman a. Tissue types are based on function of said tissue b. Epithelium: layer of cells that covers the body’s surfaces c. Muscle: groups of cells that change shape, specialized for contraction and responsible for locomotion, constriction, pumping, and peristalsis d. Nerve: groups of cells characterized by excitability; receive stimuli and transform stimuli into impulse e. Connective Tissue: group of cells that connects other tissues together in the body; relatively few cells, large amounts of ECM
![Histology [Compatibility Mode]](http://s3.studylib.net/store/data/008258852_1-35e3f6f16c05b309b9446a8c29177d53-300x300.png)