Document 7270099
advertisement

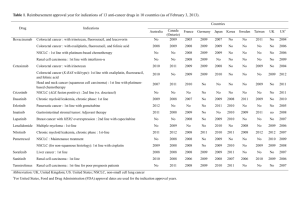
DRUG DEVELOPMENT FOR THE TREATMENT OF SOLID TUMORS Commentary to Habilitation Work by MUDr. Igor Puzanov, CSc. TABLE OF CONTENTS INTRODUCTION..............................................................................................................2 CHAPTER 1: Drug Development for Advanced Colorectal Cancer ............................2 1.1 Development of 5-Fluorouracil and 5-FU/LV as First-line Chemotherapy ..................2 1.2 Development of Capecitabine as an Oral Alternative to 5-FU ......................................3 1.3 Development of Irinotecan as Second-Line Therapy and its Integration Into FrontLine Chemotherapy........................................................................................................4 1.4 Oxaliplatin: Initial Data on Front-Line Therapy and Demonstration of its Second-Line Efficacy ..........................................................................................................................5 1.5 Comparison of Front-Line Combination Regimens ......................................................6 1.6 Bevacizumab ..................................................................................................................7 1.7 Cetuximab ......................................................................................................................8 CHAPTER 2: Drug Development for Advanced Renal Cell Carcinoma .....................8 2.1 VEGF-Targeted Therapy in metastatic RCC .................................................................9 2.1.1 Sorafenib .....................................................................................................................9 2.1.2 Sunitinib ....................................................................................................................10 2.1.3 Bevacizumab ............................................................................................................10 2.2 mTOR Targeted Therapy .............................................................................................11 2.2.1 Temsirolimus and Everolimus ..................................................................................11 2.3 Novel Agents Evaluated in mRCC ..............................................................................12 2.4 High-Dose Interleukin-2 Following VEGF-Targeted Therapy in mRCC ...................12 CHAPTER 3: Drug Development for the Treatment of Melanoma ...........................13 3.1 Targeting Cell Surface Receptors in Melanoma ..........................................................13 3.2 NF-κB Inactivation in the Treatment of Melanoma ....................................................14 3.3 Anti-angiogenic Agents in Metastatic Melanoma .......................................................14 3.4 Inhibition of Multiple Signaling Pathways in Melanoma ............................................15 3.5 Multitargeted Agents with Activity Against VEGFR and Other Cell Surface Receptors............................................................................................................................15 CONCLUSIONS ..............................................................................................................15 REFERENCES .................................................................................................................17 INTRODUCTION In the past decade, the treatment of solid tumors has seen major advances thanks to the development of new targeted therapies based on the enhanced understanding of the cancer signaling pathways on the molecular level. Effective treatment options are now available for patients with progressive refractory disease who 10 years ago would be left with best supportive care and a very poor prognosis. Although still major contributors to cancer fatalities across the world, the management of malignancies like advanced colorectal cancer, metastatic renal cell carcinoma and metastatic melanoma, has made significant gains for the patients, particularly with the development of effective antiangiogenic therapies and immunotherapies. CHAPTER 1: Drug Development for Advanced Colorectal Cancer The treatment options for colorectal cancer have seen exciting advances in the last decade. For over 30 years the treatment consisted of one marginally effective drug, 5fluorouracil (5-FU), whose activity was enhanced slightly by the addition of the biochemical modulator leucovorin (LV) (1). The number of agents approved for use in the treatment of advanced colorectal cancer in the United States has now significantly increased to include irinotecan, capecitabine, oxaliplatin, bevacizumab, and cetuximab. The emergence of multiple new agents for the treatment of advanced colorectal cancer was associated with a substantial improvement in therapeutic outcome. Analyses of clinical trials that incorporate irinotecan, oxaliplatin, bevacizumab, and/or cetuximab in combination with 5-FU/LV show that patients diagnosed with advanced disease today can expect median survival times of 22 months or beyond (2–4) compared with only 11– 13 months reported in the era when 5-FU was the only drug available to treat colorectal cancer (5). This improvement is not limited to patients treated in clinical trials. From 1974 to 1999, the five-year survival rates for Americans diagnosed with colorectal cancer rose from 50% to 63% (6), and it is reasonable to expect that data from subsequent years, when available, will show further improvements. Despite these additions to the treatment armamentarium, the statistics for colorectal cancer remain sobering. More than 146,000 new cases of colorectal cancer were diagnosed in the United States in 2004, and more than 56,000 men and women in the United States died from the disease, making it the third most common cause of cancer death (after lung cancer and prostate or breast cancer) (6). Importantly, slightly more than one-third of these people had their cancer diagnosed in an advanced stage and another 19% had distant metastases present at the time of diagnosis. 1.1. Development of 5-Fluorouracil and 5-FU/LV as First-line Chemotherapy 5-FU was first described by Heidelberger in 1957 (7). The impetus for synthesis of fluorinated pyrimidines came from the observation that rat hepatomas use radiolabeled uracil more avidly than nonmalignant tissues (8). The first clinical trials of single-agent 5-FU in the United States in early sixties were limited by the tools available to assess therapeutic impact - tumor assessment by chest X ray, radionuclide scan, or physical examination; the responses often did not have to be confirmed; and wide range of drug 2 dosages and schedules of administration. Therefore, it is not surprising that response rates reported for single-agent 5-FU in advanced colorectal cancer ranged from 3% to 45%. In phase III trials the response rates rarely exceeded 25%. Regardless of the exact response rate, single-agent 5-FU treatment clearly produced tumor shrinkage, and the responding patients experienced reduction in tumor-related symptoms. This was sufficient evidence to earn new drug approval for 5-FU by the U.S. Food and Drug Administration (FDA) on April 25, 1962. With multiple new cytotoxic agents failing to demonstrate significant clinical activity in this disease, clinical trials performed over the ensuing two decades focused on optimization of 5-FU drug administration and biochemical modulation. The most extensively studied biochemical modulators were LV, methotrexate, and interferon. In 1992, the Advanced Colorectal Cancer Meta-Analysis Project (1) summarized the results of nine controlled clinical trials that compared single-agent 5-FU to LV-modulated 5-FU in patients with previously untreated advanced colorectal cancer. The 5-FU/LV combination was associated with a significantly higher response rate than single-agent 5FU (23% versus 11%, p < 107), but only a non-significant trend towards improved median survival (11.5 versus 11.0 months, p = 0.57). This analysis was updated in 2004 to include 19 trials and more than 3300 patients with a median follow-up of 45 months (9). In addition to a doubling of the objective response rate, this meta-analysis identified a significant improvement in median survival (11.7 versus 10.5 months, p = 0.004) for patients treated with 5-FU/LV. The question of optimal schedule of 5-FU/LV administration – infusion versus bolus - was solved by a meta-analysis combining the results of seven phase III trials, in which a significant advantage for the infusional approach was found with response rate 22% vs. 14%, and median survival 12.1 vs. 11 months (p 0.04), respectively (5). A difference in toxicity was also confirmed between the two administration schedules: 31% of patients treated with 5-FU bolus by the daily 5 schedule reported 3/4 grade toxicities compared with 4% treated with 5-FU CI (p < 0.0001). A greater percentage of patients treated with 5-FU bolus experienced hematologic toxicity, while more patients receiving 5-FU infusions reported hand-foot syndrome. 1.2. Development of Capecitabine as an Oral Alternative to 5-FU 5-FU must be administered intravenously due to its unpredictable oral bioavailability. Capecitabine is an oral prodrug that is enzymatically cleaved to release 5FU preferentially in cancer cells. The developmental strategy for capecitabine was to demonstrate therapeutic non-inferiority compared to intravenous 5-FU and LV. The term ‘‘non-inferiority’’ was used rather than ‘‘equivalence’’ due to the fact that it is virtually impossible to determine that two therapies are equivalent. Two identical phase III trials were performed that randomized patients to oral capecitabine 2500 mg/m2/day 2 weeks, every 3 weeks, or to 5-FU/LV on the daily 5 (Mayo Clinic schedule), every four weeks (10,11). Capecitabine was associated with a higher objective response rate than 5-FU/LV (22.4% versus 13.2% by independent review criteria, p < 0.0001) (12,13). Time to disease progression and overall survival were virtually identical between the two treatments. Time to tumor progression (TTP) was 4.6 months for capecitabine-treated patients and 4.7 months for 5-FU/LV-treated 3 patients (p = 0.95, progression hazard ratio = 1.0) and median survival was 12.9 months for both (p = 0.91, death hazard ration = 1.0). Patients treated with daily bolus 5-FU/LV were more likely to experience diarrhea, neutropenia, stomatitis, nausea, and alopecia, while patients treated with capecitabine were more likely to experience hand–foot syndrome and hyperbilirubinemia. Based on its similar therapeutic efficacy to 5-FU/LV, its convenience, and its acceptable tolerability profile, capecitabine was granted full approval by the FDA on September 7, 2001. 1.3. Development of Irinotecan as Second-Line Therapy and its Integration Into Front-Line Chemotherapy Irinotecan binds the enzyme topoisomerase I, which prevents the uncoiling of DNA during DNA synthesis and repair, leading to apoptosis (14). Irinotecan first entered clinical trial in Japan in 1986. The results from phase I and early phase II studies began to appear in the literature in 1990. By the time the first clinical trials were initiated in France in 1990 and the United States in 1991, objective responses had been reported from Japan and there was emerging recognition of the clinical potential of irinotecan (15). There was clearly a need for another cytotoxic drug effective against advanced colorectal cancer. Patients with progressive CRC following 5-FU had limited therapeutic options beyond investigational agents. In the first phase II trial of irinotecan in Japan, Shimada and colleagues reported a 27% objective response rate in a group of previously treated and untreated patients. This prompted rapid movement of single-agent irinotecan into phase II trials in patients with advanced colorectal cancer that had progressed following 5-FU. Although objective response rates ranged from 11% to 27% in three phase II trials performed in the United States, the combined data demonstrated a 15% objective response rate, an additional 40% to 50% of patients with stable disease for at least four months, a median survival of nine months, and a reduction in tumor-related symptoms (14). Following these studies, no consensus could be reached between several potential designs for registration-directed phase III trials, which included comparison of irinotecan to single-agent mitomycin C or BCNU or to best supportive care. Fortunately, an alternative in the form of accelerated approval had become available, which allowed drugs that demonstrated beneficial effects on surrogate endpoints associated with clinical benefit to gain provisional approval based on the results of phase II trials. This provision reflected acceptance of the fact that individuals with life-threatening illnesses such as cancer and AIDS would be more willing to accept a greater degree of uncertainty, risk, or side effects from a new therapy than individuals with less severe illness or for whom effective therapies existed. The approval could be withdrawn if the confirmatory studies failed to demonstrate clear benefit. Using this mechanism in early 1996, irinotecan became the first new drug to be approved for colorectal cancer in the United States in more than 30 years. Two years later, the data from two phase III trials conducted in Europe demonstrated that irinotecan improved survival in this setting when compared to either best supportive care or infusional 5-FU. This enabled the FDA to convert irinotecan to full-approval status in 1999 (16,17). 4 Once a drug has been approved as a single agent in the refractory disease setting, the next step in its development is to combine the drug with existing front-line therapy to determine whether it improves therapeutic outcomes in that setting. Two phase III trials evaluated the combination of irinotecan and 5-FU/LV in comparison with 5-FU/LV alone as first-line chemotherapy for patients with advanced colorectal cancer. One, conducted primarily in the United States, Israel, and Australia, used irinotecan (125 mg/m2 infused over 90 minutes) added to bolus 5-FU (500 mg/m2) plus LV (20 mg/m2) given weekly for four weeks every six weeks. This became known as the IFL regimen (18). The other study, conducted primarily in Europe, compared irinotecan added to infusional 5-FU administered once every two weeks (LV5FU2 or de Gramont schedule) with the infusional 5-FU administered weekly (AIO schedule) (19). In both studies, overall survival was prolonged when irinotecan was added to 5-FU/LV and there were significant improvements in response rate, progression-free survival (PFS), a two-to three-month improvement in median survival, and a 25% reduction in the death hazard ratio. Although these improvements were associated with an increase in the frequency and severity of adverse effects, including diarrhea, vomiting, and neutropenia, overall quality of life was not impaired. As a result, in March of 2000, the FDA granted expanded indication to irinotecan to include its use in the first-line treatment of advanced colorectal cancer. 1.4. Oxaliplatin: Initial Data on Front-Line Therapy and Demonstration of its Second-Line Efficacy Oxaliplatin is a diaminocyclohexane platinum that is structurally and functionally distinct from cisplatin and carboplatin. The platinum-DNA adducts formed by oxaliplatin are bulkier and more hydrophobic and, therefore, more difficult to repair than those formed by other platinums. Oxaliplatin entered clinical testing in 1986, but it was not until 1990 that the single-agent maximum-tolerated dose was identified (20). In advanced colorectal cancer, a combination of oxaliplatin with chronomodulated 5-FU and LV resulted in a 58% response rate, a median PFS of 10 months, and a median overall survival of 15 months in a group of 93 patients, 49% of whom had received prior chemotherapy and/or radiotherapy (21). Over the ensuing years, similar phase II efficacy data were reported using nonchronomodulated drug administration schedules for this three-drug regimen. In order to better delineate the contribution of oxaliplatin to front-line chemotherapy, two phase III trials were undertaken in Europe in the mid-1990s using the oxaliplatin, 5-FU, and LV combination. One compared chronomodulated 5-FU/LV to the same regimen with oxaliplatin added (22). The other evaluated 5-FU given as a bolus and infusion combined with LV (the so-called LV5FU2 regimen) versus that same regimen with oxaliplatin added (23). While the addition of oxaliplatin to 5-FU/LV resulted in more than a doubling of objective response rates and a 40% improvement in PFS, overall survival was not significantly improved. Possible reasons offered for this therapeutic inconsistency included the small sample size and high proportion of post study cross of control patients to an oxaliplatin-containing second-line regimen. The improvement in PFS, the primary endpoint for both studies, was sufficient to garner drug approval in France in 1996 and in the European Regulatory Agency in 1999. 5 These data were brought before the U.S. Oncologic Drugs Advisory Committee in March of 2000. At that time in the United States, overall survival was considered to be the most important measure of efficacy, especially when the new agent was a cytotoxic compound associated with clinically significant toxicity. No such survival advantage was seen in the trials involving oxaliplatin. Not surprisingly, ODAC did not recommend the new drug application for oxaliplatin for approval. Addition of Irinotecan to the front-line therapy resulted in the lack of effective therapeutic options for patients with progressed disease. This opened the door for the evaluation of oxaliplatin as second-line chemotherapy. Four hundred and sixty-three patients were randomized to 5-FU/LV administered as the LV5FU2 regimen, single-agent oxaliplatin (85 mg/m2 every two weeks), or the FOLFOX4 regimen (LV5FU2 plus oxaliplatin) (24). The objective response rate (RR) was 9.9% for the FOLFOX4 group, 0% for the LV5FU2 group, and 1.3% for the oxaliplatin monotherapy group with highly significant difference between the FOLFOX4 and LV5FU2 groups (p < 0.0001). Patients treated with FOLFOX4 also experienced a longer time to tumor progression (TTP) than those treated with LV5FU2 (4.6 vs. 2.7 months; p < 0.0001). Based on a significant improvement in RR and TTP, the FDA granted accelerated approval to oxaliplatin for use in combination with 5-FU/LV for the treatment of patients with progressed advanced colorectal cancer following front-line therapy (irinotecan, 5-FU/LV) on August 9, 2002 1.5. Comparison of Front-Line Combination Regimens By the late 1990s, the challenges associated with multiple treatment options began to emerge in the field of colorectal cancer. There were little comparative data available for the various combinations involving irinotecan, oxaliplatin, and 5-FU/LV. N9741 was originally designed to explore six combination chemotherapy regimens and compare them to a reference standard of 5-FU/LV on a Mayo Clinic daily 5 schedule (26). Based on emerging data on efficacy and safety, the trial was eventually truncated to just three arms: IFL, FOLFOX4, and IROX (a combination of irinotecan and oxaliplatin). This trial was particularly important, because IFL was the most popular first-line chemotherapy regimen for advanced colorectal cancer in the United States, while FOLFOX4 was the most popular regimen in Europe. IFL and FOLFOX do not differ only in terms of the drugs contained in the regimen, but also in the way 5-FU is administered: as a weekly bolus in IFL, and as a bolus followed by infusion in FOLFOX. The trial demonstrated significant advantages for FOLFOX over IFL in terms of RR (45% vs. 31%; p = 0.002), TTP (8.7 vs. 6.9 months; p = 0.0014), and median survival (19.5 vs. 15.0 months; p = 0.0001) (26). There were no significant differences among the groups in time to treatment discontinuation, although more patients treated with FOLFOX discontinued therapy due to reasons other than disease progression compared to patients on IFL. Based on the results of this trial, the approval of oxaliplatin was expanded to include first-line treatment of advanced colorectal cancer on January 12, 2004. 6 1.6. Bevacizumab Controlling tumor growth by inhibiting tumor angiogenesis is an attractive concept, because the new blood vessels supplying the tumor are relatively small, leaky, and more reliant upon angiogenic growth factors than larger, normal blood vessels. In addition, endothelial cells were believed to lack the genetic instability of cancer cells and considered less likely to mutate into a drug-resistant phenotype. Bevacizumab (Avastin1) is a recombinant humanized monoclonal antibody directed against the vascular endothelial growth factor, one of the most potent endothelial growth factors involved in tumor-associated angiogenesis. Bevacizumab binds to vascular endothelial growth factor before it can engage its receptor, thereby depriving the tumor of new blood vessel formation required for further growth. The development of bevacizumab began with a small, first-line, randomized phase II trial in patients with metastatic colorectal cancer, comparing 5-FU/LV administered on a weekly basis for six out of eight weeks (Roswell Park schedule) with either bevacizumab (5 or 10 mg/kg every two weeks) or placebo (27). The results of this trial suggested that the 5 mg/kg dose of bevacizumab could be safely combined with bolus weekly 5-FU/LV and was associated with a very encouraging objective response rate of 40% (95% CI = 24–58%), median TTP of nine months (95% CI = 5.8–10.9 months), and median survival of 21.5 months (range: 1.2–28.2 months). More patients in the bevacizumab arms experienced a grade 3–4 adverse event including thrombotic events (5%), abdominal pain (3%), and hypertension (3%). These results prompted a large, registration-directed phase III study, designed with three arms: IFL/bevacizumab, IFL/placebo, and 5-FU/LV (Roswell Park schedule)/bevacizumab (4). Once IFL/bevacizumab combination was found to be acceptably safe, the 5-FU/LV/bevacizumab arm was closed and the trial proceeded as a two-arm study. The addition of bevacizumab to IFL significantly improved all measures of therapeutic efficacy, including objective response rate, 44.8% versus 34.8% (p = 0.004); PFS 10.6 versus 6.2 months median (p < 0.001, HR for progression: 0.54); and overall survival, 20.3 versus 15.6 months (p < 0.001, HR for death: 0.66). As observed in earlier trials, the addition of bevacizumab to chemotherapy increased the rates of grade 3 hypertension, proteinuria, arterial thrombotic events, and gastrointestinal perforations. In a smaller phase III trial with patients considered medically unfit for treatment with IFL, the addition of bevacizumab to 5-FU/LV improved objective response rates from 15% to 26% ( p = 0.055), PFS from 5.5 to 9.2 months ( p = 0.0002, progression HR = 0.50), and median survival from 12.9 to 16.6 ( p = 0.16, death HR = 0.79). Similar trends of increased toxicity were observed in this study. A pooled analysis of three studies comparing 5-FU/LV to 5-FU/LV/bevacizumab demonstrated significant improvements in all measures of efficacy (29). Based on these studies, the FDA granted full approval to bevacizumab on February 26, 2004 for use with a 5-FU-based chemotherapy regimen in the first-line treatment of patients with metastatic colorectal cancer. 7 1.7. Cetuximab Cetuximab is also a mouse–human chimeric IgG1 monoclonal antibody with high affinity for EGF receptor. Unlike bevacizumab, cetuximab binds directly to the EGFR, thereby blocking the signaling that occurs when a natural ligand binds to this receptor. Following two small phase II trials that failed to clearly demonstrate the efficacy of cetuximab to the FDA, a larger, randomized Phase II trial was designed to generate definitive data required for drug registration (32). The trial was designed with a 2:1 randomization to the Irinotecan/cetuximab arm and required all patients with irinotecanrefractory disease to have EGFR-expressing tumors. A 23% objective response rate was observed in the group treated with the Irinotecan/cetuximab combination, whereas an 11% response rate was reported in group treated with cetuximab alone (p = 0.007). Similar trend was observed in other measures (PFS, 4.1 vs. 1.5 months; median survival, 8.6 vs. 6.9 months). A consistent correlation has been observed between intensity of skin rash and increased likelihood of response and prolonged survival. Cetuximab-related toxicities included acne-like skin rash and hypersensitivity reactions. The rash is generally of cosmetic concern, but for some patients can be clinically significant. When used in combination, cetuximab did not appear to lessen or exacerbate toxicities associated with irinotecan. The FDA granted an accelerated approval for cetuximab on February 12, 2004 based on this phase II data due to the beneficial outcome observed in terms of PFS and response rate, in conjunction with tumor-related symptoms, in patients refractory on 5-FU, Irinotecan and oxaliplatin. CHAPTER 2: Drug Development for Advanced Renal Cell Carcinoma Recent developments in the treatment of renal cell cancer (RCC) have generated renewed excitement in an area of oncology where up to three years ago therapeutic options were consistently limited and, at best, minimally effective. RCC, particularly the clear cell subtype, represents an important example of how better understanding of molecular pathogenesis can be successfully translated into more effective therapies. The completion of several clinical trials with targeted agents has resulted in a shift in the treatment paradigm of advanced RCC (34-37). However, considerable challenges remain with both clear cell and non-clear cell subtypes of the disease, and metastatic RCC remains a fatal disease for the majority of patients. Over 54,000 new cases of RCC and 13,000 deaths will occur in the U.S. in 2008 and the incidence of these cancers has increased by approximately 2% per year. RCC represents the third leading cause of death among genitourinary malignancies and the twelfth leading cause of cancer death overall in the United States. Worldwide, the annual mortality from RCC is over 100,000 patients (38). In the Czech Republic, 1,200 people die annually, and the Czech Republic has one of the highest incidences of RCC in Europe (2,800 cases). The management of metastatic RCC has undergone a revolution in the last decade. We came a long way from the use of debulking radical nephrectomy followed by 39, 40). More recently 8 systemic therapy targeted toward VEGF produced robust clinical effects for metastatic RCC, leading to regulatory approval of two multikinase inhibitors - sorafenib (Nexavar®) and sunitinib (Sutent®). In addition, a ligand-binding antibody, bevacizumab (Avastin®) was approved in combination with IFN in Europe and is under consideration by FDA in the US. The latest addition to our armamentarium includes temsirolimus (Torisel®), an mTOR inhibitor with promising activity in patients with non-clear cell RCC histologies and poor prognosis by MSKCC criteria. These advances have collectively refined the management of metastatic RCC. 2.1. VEGF-Targeted Therapy in metastatic RCC Inactivating mutations or methylation in the von Hippel-Lindau (VHL) gene were observed in the majority of sporadic clear cell RCC tumors (41). Resulting constitutive activation of the hypoxia response pathway leads to up-regulated expression of multiple genes important for tumor angiogenesis, including VEGF and PDGF. Various strategies have been developed to block these pathways, including antibodies that sequester VEGF, such as bevacizumab (Avastin®), tyrosine kinase inhibitors that block the receptors for VEGF and PDGF, such as sorafenib (Nexavar®) and sunitinib (Sutent®). 2.1.1. Sorafenib Sorafenib is an orally bioavailable, bi-aryl urea originally identified as an inhibitor of raf kinase, an enzyme involved in cellular proliferation that inhibits the VEGF and PDGF receptor families (42). Sorafenib was investigated in a phase II, randomized discontinuation trial, in which 202 patients with metastatic RCC were evaluated. The overall tumor shrinkage rate was 71%, with a PFS advantage in the patients receiving sorafenib (24 vs. 6 weeks, p = 0.0087) (43). A subsequent Phase III randomized trial of sorafenib versus placebo in previously treated (cytokine-refractory) metastatic RCC was conducted (34). Seven (2%) patients receiving the drug had an objective response, defined by RECIST criteria. Significant advantages of sorafenib were observed in other end points (stable disease, 78% vs. 55%; tumor shrinkage 74%; median PFS, 24 vs. 12 weeks, P = 0.000001). PFS across all subgroups of patients receiving sorafenib appeared to be superior to placebo, including a subset of patients who had not received prior cytokine therapy. The study was later modified to allow cross-over from placebo to sorafenib, and after 6 months from cross-over the median overall survival was 19.3 months for sorafenib-treated patients versus 15.9 months for placebo (44). A statistically significant survival benefit was obscured by patient cross-over. Overall, sorafenib was well tolerated, and side effects were manageable. The FDA granted approval of this agent in December 2005 for the treatment of patients with advanced RCC. The subsequent randomized Phase II trial evaluating sorafenib versus IFN- in untreated metastatic RCC patients did not show sorafenib superiority to IFN in improvement of PFS (5.6 vs. 5.7 months), although patient on sorafenib had a better quality of life and symptom improvement. This surprising result might have been caused by insufficient sorafenib dose (45). The original trials with sorafenib indicated that a dose of 400 mg twice a day was well-tolerated and associated with antitumor activity. 9 Subsequent clinical trials have indicated that dose escalation up to 1600 mg/day is feasible, and may be associated with increased antitumor activity (46). In a trial evaluating the addition of sorafenib to IFN- therapy in untreated mRCC patients, the treatment consisted of 8-week cycles of sorafenib 400 mg twice daily plus 10 MU of IFN- SC 3 times a week. The ORR by RECIST criteria was 42% (38% partial response, 4% complete response). An additional 46% had stable disease for at least 1 cycle, including 8% with over 20% tumor shrinkage. Toxicities were mostly Grade ½. Further investigation is required to demonstrate clinical benefit of this combination over monotherapy. 2.1.2. Sunitinib Sunitinib is an orally bioavailable inhibitor of VEGFR-2 and PDGFR-β. In two sequentially conducted single-arm multicenter Phase II trials the activity of sunitinib was investigated in total 169 cytokine-refractory metastatic RCC patients (48). The majority of patients (87%) had clear cell histology and 93% of patients had undergone cytoreductive nephrectomy. All patients had received prior cytokine-based therapy. Patients were treated with 50 mg of sunitinib orally daily on a 4-week-on/2-week-off cycle. The ORR was 34% and a median PFS was 8.3 months. These data led to the FDA approval of this drug in January 2006 for the management of advanced RCC. To evaluate the activity of sunitinib in previously untreated metastatic RCC patients, a randomized Phase III study was undertaken (35). Previously untreated metastatic RCC patients (n = 750) with clear cell histology were randomized 1:1 to receive sunitinib (6-week cycles: 50 mg orally once daily for 4 weeks, followed by 2 weeks off [4/2 schedule]) or IFN- (6-week cycles: SC injection 9 MU given 3 times weekly). The ORR was 31% versus 6% (P = 0.000001) and the median PFS was 11 versus 5 months in favor of sunitinib-treated patients (P = 0.00001). The most common toxicities included fatigue/asthenia, diarrhea, stomatitis, dermatitis, and hypertension. Finally, sunitinib also prolonged the OS (median 26.4 vs. 21.8 months, p=0.051) (16). This trial has demonstrated that sunitinib is superior to IFN- in untreated advanced RCC patients, making it one of several frontline treatment options for advanced RCC patients. 2.1.3. Bevacizumab The clinical utility of bevacizumab in metastatic RCC was investigated in a randomized Phase II trial, in which 116 patients with metastatic, cytokine-refractory clear-cell RCC were randomized to receive placebo, low-dose (3 mg/kg) bevacizumab, or high-dose (10 mg/kg) bevacizumab given intravenously every 2 weeks (51). The study was designed to detect a two-fold TTP increase with either dose of bevacizumab versus placebo (4.8 versus 2.5 months; P = 0.001 by log-rank test) with 10% ORR. Common toxicity included hypertension and proteinuria, more commonly seen in the high-dose bevacizumab arm. The addition of an antiangiogenic agent to standard cytokines has also been explored. Recently reported Phase III trial has evaluated bevacizumab plus IFN- versus IFN- alone in untreated advanced RCC patients (37). The results revealed a high 30% 10 ORR and median PFS of 10.2 months for a combination arm vs. 5.6 months for IFN (p<0.0001). Another rational approach currently being evaluated is a simultaneous targeting of two steps within the VEGF pathway (i.e., using a ligand binding agent with a small tyrosine kinase inhibitor [TKI]). A Phase I/II trial evaluating the combination of sorafenib with bevacizumab reported 53% ORR and 15.3 months PFS (52). The Eastern Cooperative Oncology Group (ECOG) has started a randomized Phase II trial with bevacizumab, bevacizumab/sorafenib, bevacizumab/temsirolimus or temsirolimus/sorafenib combinations. 2.2. mTOR Targeted Therapy Another emerging target in RCC is the enzyme mammalian target of rapamycin (mTOR). This protein modulates a number of cellular processes, including proliferation, nutrient uptake and metabolism, and HIF expression. Given its central role in cell biology, the newer strategies for treating RCC now include agents that not only disrupt VEGF or its receptor, but also mTOR. 2.2.1. Temsirolimus and Everolimus Temsirolimus is an inhibitor of mammalian target of rapamycin (mTOR) - a molecule implicated in multiple tumor-promoting intracellular signaling pathways, including hypoxia-inducible factor (HIF) transcription (53). A randomized Phase III trial was conducted in patients with poor-risk metastatic RCC as defined by existing prognostic schema (36). Patients were equally randomized to receive IFN- up to 18 MU SC 3 times a week, temsirolimus 25 mg IV once a week, or temsirolimus 15 mg IV once a week plus IFN- 6 MU SC 3 times a week. Patients treated with temsirolimus had a statistically longer survival than those treated with IFN- alone (10.9 vs. 7.3 months, P = 0.0069). There was no difference in the combination arm possibly as a result of a lower dose of temsirolimus coupled with an increased number of patients unable to receive temsirolimus secondary to IFN- -related toxicities. Further investigation of this agent is planned in patients with fewer adverse risk features and in combination with VEGFtargeting therapies. A recently reported Phase III randomized, placebo-controlled study evaluated the activity of RAD-001 (Everolimus), an oral serine-threonine kinase inhibitor of mTOR, as second-line therapy in advanced RCC (54). In this trial, 410 patients with metastatic clear cell RCC were randomly assigned in a 2:1 ratio to everolimus (10 mg per day) or placebo. The PFS was 4.0 months vs. 1.9 months on placebo (HR 0.3, 95%CI 0.22-0.40). The PFS at 6 months was 26% on everolimus vs. 6% on placebo. Treatment-related adverse events included mucositis, skin rash, pneumonitis, hypophosphatemia, hyperglycemia, thrombocytopenia, anemia, and elevated liver function tests. These studies demonstrate the importance of mTOR as a therapeutic target in RCC and suggest a potential benefit of these agents in a broader RCC population. 11 2.3. Novel Agents Evaluated in mRCC Several other novel agents that have shown activity in advanced RCC include GW786034 (Pazopanib), a multitarget TKI that inhibits VEGFR-1, -2, -3, PDGFR- , PDGFR-β, and c-kit (55), AG013736 (Axitinib), an orally bioavailable small-molecule TKI of VEGFR-2 and PDGFR-β (56). A Phase II single-arm, multicenter trial of AG013736 in cytokine-refractory RCC patients (n = 52) demonstrated an ORR of 40%. Stable disease was observed in 21 (40%) of patients with 20 of the patients experiencing tumor shrinkage over 30%. Median TTP has not been reached with a median of 12 to 18 months of follow up for most patients. Similar to other small-molecule TKIs, most toxicity was Grade 1 or 2, and included gastrointestinal, dermatologic, fatigue, hypertension, and proteinuria. An additional study evaluating the activity of this agent in sorafenib-refractory metastatic RCC patients is underway. 2.4. High-Dose Interleukin-2 Following VEGF-Targeted Therapy in mRCC High-dose (HD) bolus interleukin-2 (IL-2) has been FDA approved for therapy of metastatic RCC since 1992 based on its ability to induce durable responses in a small percentage of patients (57, 58). The efficacy of HD IL-2 has subsequently been confirmed in two separate large randomized trials (59, 60). However, due to substantial toxicity, only specialized centers continue to offer this therapy with focus on developing patient selection strategies to limit IL-2 therapy only to patients most likely to experience clinical benefit (61, 62). Since the responses to VEGF-targeted therapies are typically not complete or durable, second line of treatment is necessary. The safety and efficacy of HD IL-2 following prior therapy with VEGF-targeted agents was explored in a retrospective analysis of clinical outcomes of patients with mRCC and compared to the results of the phase III Cytokine Working Group (CWG) trial that compared HD IL-2 alone to subcutaneous IL-2 plus IFN (60). The analysis suggests that the toxicity of IL-2 therapy may be higher in patients who have received prior VEGF-targeted therapy, compared with the patients in the CWG trial who were untreated prior to that trial. This increase in severe cardiovascular toxicity was limited only to patients who had received prior TKI treatment and not to patients previously treated with bevacizumab alone. Sunitinib has been demonstrated to reduce cardiac ejection fraction by at least 10% in 28% of patients treated at the approved dose (63). In animal models, the mechanism of this decline in left ventricular function appears to be direct cardiomyocyte toxicity through mitochondrial injury. No patient treated with IL-2 following VEGF-targeted therapy experienced a partial or complete response, which was significantly lower than the 23.2% response rate reported for the HD IL-2 arm of the Phase III CWG trial (P=0.001). However, the clinical significance of this result is unclear since 98% of patients in CWG trial were treatmentnaïve. 12 CHAPTER 3. Drug Development for the Treatment of Melanoma Angiogenesis is a hallmark of melanoma progression. Antiangiogenic agents have been infrequently tested in patients with advanced melanoma. Experience with most other cancers suggests that combinations of antiangiogenic agents with either chemotherapy or other targeted therapy will be needed for significant clinical benefit. In melanoma, numerous cellular pathways important to cell proliferation, apoptosis, or metastases have recently been shown to be activated. Activation occurs through specific mutations (B-RAF, N-RAS, and PTEN) or changes in expression levels of various proteins (PTEN, BCL-2, NF-κB, CDK2, and cyclin D1). Agents that block these pathways are rapidly entering the clinical setting, including RAF inhibitors (sorafenib), mitogen-activated protein kinase inhibitors (PD0325901), mTOR inhibitors (CCI-779), and farnesylate transferase inhibitors (S115777) that inhibit N-RAS, and proteosome inhibitors (PS-341) that block activation of nuclear factor-κB (NF-κB). The evaluation of these agents alone, in combination with each other, or with chemotherapy in patients with melanoma will be challenging. To rationally and optimally develop these targeted agents, it will be critical to adequately test for the presence of the presumed cellular target in tumor specimens and the effect of therapy on the proposed target (biological response). 3.1. Targeting Cell Surface Receptors in Melanoma Melanoma expresses a number of growth factor receptors, including EGFR, PDGFR, and c-kit, and their expression levels changes with the disease progression (6466). Some preclinical studies suggested potential anti-melanoma effect of the inhibition of these growth factors, which lead to cautious investigation of these inhibitors in melanoma. In a phase II study, patients experienced significant Grade 3 and 4 toxicity, and no objective clinical responses were seen (67). The median TTP was 54 days and the median OS was 200 days, with no patients being disease free at 6 months (43). Immunohistochemical examination of the tumors revealed very low expression of c-kit, as well as PDGFR- and PDGFR-, which did not appear to influence the clinical outcome and it was concluded that imanitib is inactive as a single-agent therapy for metastatic melanoma. In a small phase II trial targeting EGFR, erlotinib was administered at its maximum tolerated dose (150 mg/day). The treatment was well tolerated, but no objective responses were attained, and only one patient had stable disease over 6 months. These disappointing results maybe partially explained by the observation that in the nonsmall cell lung cancer the responses to EGFR inhibitors are not related to the surface levels of the receptor, but rather to the activating mutations in the receptor, which are yet to be identified in melanoma (68). 13 3.2. NF-κB Inactivation in the Treatment of Melanoma The NF-κB-mediated gene transcription can be efficiently inactivated by using proteasome 26S inhibitor PS-341 in vitro in melanoma, as well as in a murine xenograft melanoma model, either alone or in combination with temozolomide (69-71). The inhibition of the proteasome averts the breakdown of IκB, a cytosolic protein that binds NF-κB and prevents its translocation to the nucleus. Although a single arm phase II trial of PS-341 showed no activity in melanoma, a small phase I trial of PS-341 in combination with temozolomide was started, in which half of the patients had a decline in NF-κB activation in peripheral blood, 20S proteasome inhibition in blood was 60-80 %, and 4 of 19 patients showed some tumor regression. Immunohistochemistry of tumor biopsies obtained prior and post treatment showed decrease in nuclear-translocated p65 NF-κB expression in two out of three samples. A larger phase II trial of this combination in chemotherapy-naïve and pre-treated patients is being currently initiated. 3.3. Anti-angiogenic Agents in Metastatic Melanoma Angiogenesis is a critical step in the melanoma transformation. Serum levels of VEGF increase with clinical stage in melanoma patients and can be predictive of worse prognosis. In a trial evaluating the activitiy of bevacizumab alone and a combination of bevacizumab and low-dose INF- in patients with melanoma, the combination arm showed some promising activity and the trial was redesign to incorporate high-dose INF. Studies of bevacizumab and erlotinib have been proposed, since in vitro and in xenograft melanoma models this combination results in a cooperative antitumor effect by blocking VEGFR and EGFR1 pathways simultaneously (72, 73). Another potentially worthwhile combination is chemotherapy (carboplatin + paclitaxel) plus sorafenib as an example of antiangiogenic agent enhancing the effects of chemotherapy. In a phase II study that evaluated the efficacy and safety of sorafenib plus dacarbazine in patients with advanced melanoma, the median PFS was considerably higher in the combination arm, and improvement of other clinical measures was observed as well (PFS, TTP). While the treatment had an acceptable toxicity profile, there was no significant difference in OS between the arms. However, these results are encouraging and warrant further studies of this combination. Thalimid/revlimid combination has shown important clinical effects in patients with advanced melanoma, and although previously thought to be antiangiogenic agents, the exact mechanism of their function remains unclear. v3 is an integrin expressed in many cancers, including melanoma, but not in normal melanocytes. Its expression in melanoma primary lesions increases as they progress from the horizontal to vertical growth phase. The MEDI-522 antibody is a humanized form of a murine antibody called LM609 that binds v3, triggering antibody-dependent cellular cytotoxicity and potentially blocking tumor growth in mice by directly causing tumor cell apoptosis and impairment of tumor angiogenesis (74). Preliminary results of a phase II study of MEDI-522 alone or its combination with dacarbazine chemotherapy were disappointing, showing some tumor response and slightly better, but still short, PFS only in the combination arm. 14 3.4. Inhibition of Multiple Signaling Pathways in Melanoma Many pathways are likely to contribute to melanoma resistance to cytotoxic chemotherapy, including the PI3K/Akt pathway (75–79), MAPK pathway, and NF-κBmediated events. It has been shown that inhibition of both the MAPK pathway and NFκB in combination may produce enhanced antitumor effects (80). For example, PS-341 induces expression of an anti-apoptotic protein, Mcl-1, as a cell survival mechanism, so a simultaneous inhibition of the MAPK pathway could depress expression of Mcl-1. Apoptosis resistance is a hallmark of melanoma, and there are a number of new agents in development attempting to overcome this property (71, 78, 81). IκB kinase- inhibitor, such as BMS-345541, will block NF-κB activation more specifically and effectively than a proteosome inhibitor (82). Inhibition of mTOR, a critical component of the PI3K/Akt pathway, with agents such as CCI-779 (phase 2/3) and RAD001 (phase 1/2) affords great promise (83–85). PTEN expression is either lost or the gene is mutated in a number of melanomas, leading to activation of the PI3K/Akt pathway (77–79). Inhibition of both RAS and RAF with the combination of R115777 (farnesylate transferase inhibitor) and sorafenib may more effectively block the MAPK pathway than either agent alone. Downstream from RAS are several signaling pathways, including the PI3K/Akt pathway, that could be inhibited simultaneously with an agent such as R115777. 3.5. Multitargeted Agents with Activity Against VEGFR and Other Cell Surface Receptors SU011248, AG013736, and ZD6474 are all oral tyrosine kinase inhibitors that already show promise in other cancers, including clear cell renal carcinoma (84). They are effective inhibitors for the VEGFR2 receptor signaling but also block one or more other receptors. Targets for both SU011248 and AG13736 include VEGFR2, PDGF, and c-kit, whereas ZD6474 blocks both VEGFR2 and EGFR1. The ability of these agents to inhibit multiple targets makes them of interest to investigate in patients with melanoma alone, with chemotherapy, or with other targeted agents. CONCLUSIONS The emergence of five new drugs for the treatment of advanced colorectal cancer over the past 10 years has doubled the median survival in this disease from 11 to 22 months. Effective therapies exist not only for first-line treatment, but for second-and third-line treatment, as well. But our perspective must be tempered by the fact that very few patients with metastatic colorectal cancer are cured, and five-year survival rates are still less than 10%. While it is clear that further improvements are needed, it is not clear how these new drugs for advanced colorectal cancer will be developed. It is likely that the combination approach for the new drug development will be the most effective one in this setting as well. With multiple therapeutic options now available to patients with metastatic RCC, the most appropriate sequencing of these therapies must be investigated. Sorafenib, 15 sunitinib and temsirolimus have already assumed a substantial role in the management of advanced RCC, but their optimal usefulness is not well defined. Redundancy within molecular pathways implicated in tumor cell growth, coupled with the ability for crosstalk between the components of these pathways, suggests that single-target inhibition of VEGF and its pathway may be insufficient to induce durable antitumor effects in all patients. The next five to ten years will offer physicians treating patients with metastatic melanoma and the patients themselves an entirely new and different set of treatment options to fight this disease. Deepening the understanding of melanoma genetics and advances in anti-tumor immunity will provide new relevant targets for drug development. Another promising treatment route for melanoma that requires further studies is using antiangiogenic agents. 16 References 1. Jemal A, Tiwari RC, Murray T, et al. Cancer statistics, 2004. Cancer J Clin 2004; 54:8–29. 2. Heidelberger C, Chaudhuri NK, Danneberg P, et al. Fluorinated pyrimidines, a new class of tumour-inhibitory compounds. Nature 1957; 179:663–666. 3. Rutman RJ, Cantarow A, Paschkis KE. Studies on 2-acetylaminofluorene carcinogenesis: III. The utilization of uracil-2-C14 by pre-neoplastic rat liver. Cancer Res 1954; 14:119–126. 4. Meta-Analysis Group in Cancer. Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: an updated meta-analysis. J Clin Oncol 2004; 22:2766– 3775. 5. Van Cutsem E, Twelves C, Cassidy J, et al. Oral capecitabine compared with intravenous fluorouracil plus leucovorin in patients with metastatic colorectal cancer: results of a large Phase III study. J Clin Oncol 2001; 19:4097–4106. 6. Hoff PM, Ansari R, Batist G, et al. Comparison of oral capecitabine versus intravenous fluorouracil plus leucovorin as first-line treatment in 605 patients with metastatic colorectal cancer: results of a randomized Phase III study. J Clin Oncol 2001; 19:2282– 2292. 7. Twelves C on behalf of the Xeloda Colorectal Cancer Group. Capecitabine as first-line treatment in colorectal cancer: pooled data from two large, phase III trials. Eur J Cancer 2002; 38:S15–S20. 8. Cassidy J, Twelves C, Van Cutsem, et al. First-line oral capecitabine therapy in metastatic colorectal cancer: a favourable safety profile compared with intravenous 5fluorouracil/leucovorin. Ann Oncol 2002; 13:566–575. 9. Rothenberg ML. CPT-11 (irinotecan): an original spectrum of clinical activity. Semin Oncol 1996; 23(suppl 3):21–26. 10. Shimada Y, Yoshino M, Wakui A, et al. Phase II study of CPT-11, a new camptothecin derivative, in metastatic colorectal cancer. CPT-11 Gastrointestinal Cancer Study Group. J Clin Oncol 1993; 11:909–913. 11. Cunningham D, Pyrhonen S, James RD, et al. Randomised trial of irinotecan plus supportive care versus supportive care alone after fluorouracil failure for patients with metastatic colorectal cancer. Lancet 1998; 352:1413–1418. 12. Rougier P, Van Cutsem E, Bajetta E, et al. Randomised trial of irinotecan versus fluorouracil by continuous infusion after fluorouracil failure in patients with metastatic colorectal cancer. Lancet 1998; 352:1407–1412. 13. Saltz L, Cox JV, Blanke C, et al. Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. N Engl J Med 2000; 343:905–914. 14. Douillard JY, Cunningham D, Roth AD, et al. Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multi-centre randomised trial. Lancet 2000; 355:1041–1047. 15. Extra J-M, Marty M, Brienza, S, Misset J-L. Pharmacokinetics and safety profile of oxaliplatin. Semin Oncol 1998; 25(suppl 5):13–22. 16. Le´vi F, Misset J-L, Brienza S, et al. Chronopharmacologic phase II clinical trial with 5-fluorouracil, folinic acid, and oxaliplatin using an ambulatory multichannel programmable pump. Cancer 1992; 69:893–900. 17 17. Giacchetti S, Perpoint B, Zidani R, et al. Phase III multicenter randomized trial of oxaliplatin added to chronomodulated fluorouracil–leucovorin as first-line treatment of metastatic colorectal cancer. J Clin Oncol 2000; 18:136–147. de Gramont A, Figer A, Seymour M, et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 2000; 18:2938–2947. 18. Rothenberg ML, Oza AM, Bigelow RH, et al. Superiority of oxaliplatin and fluorouracil–leucovorin compared with either therapy alone in patients with progressive colorectal cancer after irinotecan and fluorouracil–leucovorin: interim results of a phase III trial. J Clin Oncol 2003; 21:2059–2069. 19. Rothenberg ML, Oza AM, Burger B, et al. Final results of a Phase III trial of 5FU/leucovorin versus oxaliplatin versus the combination in patients with metastatic colorectal cancer following irinotecan, 5-FU, and leucovorin. Proc Am Soc Clin Oncol 2003; 22:252 (abstr 1011). 20. Goldberg RM, Sargent DJ, Morton RF, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol 2004; 22:23–30. 21. Kabbinavar F, Hurwitz HI, Fehrenbacher L, et al. Phase II, randomized trial comparing bevacizumab plus fluorouracil/leucovorin with fluorouracil/leucovorin alone in patients with metastatic colorectal cancer. J Clin Oncol 2003; 21:60–65. 22. Kabbinavar FF, Schulz J, McCleod M, et al. Addition of bevacizumab to bolus fluorouracil and leucovorin in first-line metastatic colorectal cancer: results of a randomized phase II trial. J Clin Oncol 2005; 23:3697–3705. 23. Kabbinavar FF, Hambleton J, Mass RD, et al. Combined analysis of efficacy: the addition of bevacizumab to fluorouracil/leucovorin improves survival for patients with metastatic colorectal cancer. J Clin Oncol 2005; 223:3706–3712. 25. Saltz L, Rubin MS, Hochster HS, et al. Cetuximab plus irinotecan is active in irinotecan-refractory colorectal cancer that expresses epidermal growth factor receptor. Proc Am Soc Clin Oncol 2001; 20 (abstract 3a). AQ5 26. Saltz LB, Meropol NJ, Loehrer PJ Sr, et al. Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol 2004; 22:1201–1208. 27. Cunningham D, Humblet Y, Siena S, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med 2004; 251:337–345. 28. Johnson JR, Williams G, Pazdur R. End points and United States Food and Drug Administration approval of oncology drugs. J Clin Oncol 2003; 21: 1404–1411. 29. Advanced Colorectal Cancer Meta-Analysis Project. Modulation of fluorouracil by leucovorin in patients with advanced colorectal cancer: evidence in terms of response rates. J Clin Oncol 1992; 10:896–903. 30. Tournigand C, Andre T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol 2004; 22:229–237. 31. Grothey A, Sargent D, Goldberg RM, Schmoll H-J. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil– leucovorin, irinotecan, and oxaliplatin in the course of treatment. J Clin Oncol 18 2004; 22:1209–1214. 32. Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 2004; 350:2335–2342. 33. Meta-Analysis Group in Cancer. Efficacy of intravenous continuous infusion of fluorouracil compared with bolus administration in advanced colorectal cancer. J Clin Oncol 1998; 16:301–308. 34. Escudier B; Eisen T; Stadler WM; Szczylik C; et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007 Jan 11;356(2):125-34. 35. Robert J. Motzer, M.D., Thomas E. Hutson, D.O., Pharm.D., Robert A. Figlin, M.D et al. Sunitinib versus Interferon Alfa in Metastatic Renal-Cell Carcinoma, N Engl J Med. 2007, Jan 11, 356:115-124. 36. Hudes G; Carducci M; Tomczak P; Dutcher J; Figlin R et al. Temsirolimus, interferon alfa, or both for advanced renal-cell carcinoma. N Engl J Med. 2007 May 31;356(22):2271-81 37. Escudier B; Pluzanska A; Koralewski P; Ravaud A; Bracarda S; Szczylik C et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet. 2008 Dec 22;370(9605):2103-11 38. Jemal A, Siegel R, Ward E, et al. Cancer Statistics 2007. CA Cancer J Clin 2007;57:43–66. 39. Flanigan RC, Salmon SE, Blumenstein BA, et al. Nephrectomy followed by interferon alfa-2b compared with interferon alfa-2b alone for metastatic renal-cell cancer. N Engl J Med 2001;345:1655–1659. 40. Mickisch GH, Garin A, van Poppel H, et al. Radical nephrectomy plus interferonalfa-based immunotherapy compared with interferon alfa alone in metastatic renal-cell carcinoma: a randomized trial. Lancet 2001;358:966–970 41. Rini BI, Small EJ. Biology and clinical development of vascular endothelial growth factor-targeted therapy in renal cell carcinoma. J Clin Oncol 2005;23:1028–1043. 42. Wilhelm S, Carter C, Tang L, et al. BAY 43–9006 exhibits broad spectrum antitumor activity and targets raf/MEK/ERK pathway and receptor tyrosine kinases involved in tumor progression and angiogenesis. Proc Am Assoc Cancer Res 2003;44:A78. 43. Ratain MG, Eisen T, Stadler WM, et al. Phase II placebo-controlled randomized discontinuation trial of sorafenib in patients with metastatic renal cell carcinoma. J Clin Oncol 2006;24:2505–2512. 44. Eisen T, Bukowski RM, Staehler M, et al. Randomized phase III trial of sorafenib in advanced renal cell carcinoma (RCC): Impact of crossover on survival [abstract]. J Clin Oncol 2006;24 (suppl):4524. Abstract 4524. 45. Szczylik, C, Demkow, T, Staehler, M, et al. Randomized phase II trial of first-line treatment with sorafenib versus interferon in patients with advanced renal cell carcinoma: Final results. (Abstract). J Clin Oncol 2007; 25:241s. 46. Amato, RJ, Harris, P, Dalton, M, et al. A phase II trial of intra-patient dose-escalated sorafenib in patients (pts) with metastatic renal cell cancer (MRCC). (Abstract). J Clin Oncol 2007; 25:241s 47. Gollob J, Rathmell, K, Richmond T, et al. Phase II Trial of Sorafenib plus Interferon Alfa-2b as First- or Second-Line Therapy in Patients with Metastatic Renal Cell Cancer. Journal of Clinical Oncology, Vol 25, No 22 (August 1), 2007: pp. 3288-3295 19 48. Motzer RJ, Rini BI, Bukowski RM, et al. Sunitinib in patients with metastatic renal cell carcinoma. JAMA 2006;295:2516–2524. 49. Figlin, RA, Hutson, TE, Tomczak, P, et al. Overall survival with sunitinib versus interferon (IFN)-alpha as first-line treatment of metastatic renal cell carcinoma (mRCC) (Abstract). J Clin Oncol 2008; 26:256s. 50. Presta LG, Chen H, O'Connor SJ, et al. Humanization of an anti-vascular endothelial growth factor monoclonal antibody for the therapy of solid tumors and other disorders. Cancer Res 1997;57:4593–4599. 51. Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an antivascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med 2003;349:427–434. 52. J. A. Sosman, K. T. Flaherty, M. B. Atkins, D. F. McDermott, M. L. Rothenberg, W. L. Vermeulen, K. Harlacker, A. Hsu, J. J. Wright, I. Puzanov Updated results of phase I trial of sorafenib and bevacizumab in patients with metastatic renal cell cancer. J Clin Oncol 26: 2008 (May 20 suppl; abstr 5011) 53. Hudson CC, Liu M, Chiang GG, et al. Regulation of hypoxia-inducible factor 1alpha expression and function by the mammalian target of rapamycin. Mol Cell Biol 2002;22:7004–7014. 54. Motzer, RJ, Escudier, BJ, Oudard, S, et al. RAD001 plus best supportive care (BSC) vs BSC plus placebo in patients with metastatic renal cell carcinoma (RCC), that has progressed on VEGFr-TKI therapy: Results from a randomized, double-blind, multicenter phase III study (Abstract). J Clin Oncol 2008; 26:256s. 55. Hutson TE, Bukowski RM. A phase II study of GW786034 using a randomized discontinuation design in patients with locally recurrent or metastatic clear-cell renal cell carcinoma. Clin Genitourin Cancer 2006;4:296–298. 56. Rixe O; Bukowski RM; Michaelson MD; Wilding G; Hudes GR et al. Axitinib treatment in patients with cytokine-refractory metastatic renal-cell cancer: a phase II study Lancet Oncol. 2007 Nov;8(11):975-84. 57. Fyfe GA, Fisher RI, Rosenberg SA, Sznol M, Parkinson DR, Louie AC. Long-term response data for 255 patients with metastatic renal cell carcinoma treated with high-dose recombinant interleukin-2 therapy. J Clin Oncol. 1996; 14(8): 2410-1. 58. Fisher RI, Rosenberg SA, Fyfe G. Long-term survival update for high-dose recombinant interleukin-2 in patients with renal cell carcinoma. Cancer J Sci Am. 2000; 6: S55-S57. 59. Yang JC, Sherry RM, Steinberg SM, et al. Randomized study of high-dose and lowdose interleukin-2 in patients with metastatic renal cancer. J Clin Oncol. 2003; 21(16):3127-32. 60. McDermott DF, Regan MM, Clark JL, et al. Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol. 2005; 23(1): 133-141. 61. Upton MP, Parker R, Youmans AY, McDermott DF, Aktins MB. Histologic predictors of renal cell carcinoma response to interleukin-2 based therapy. J Immunother. 2005; 28(5): 488-95. 62. Atkins M, Regan M, McDermott D, et al. Carbonic anhydrase IX expression predicts outcome of interleukin 2 therapy for renal cancer. Clin Cancer Res. 2005; 11(10): 37143721. 20 63. Chu TF, Rupnick MA, Kerkela R, et al. Cardiotoxicity associated with tyrosine kinase inhibitor sunitinib. Lancet. 2007; 370(9604): 2011-9. 64. Luan J, Shattuck-Brandt R, Haghnegahdar H, et al. Mechanism and biological significance of constitutive expression of MGSA/GRO chemokines in malignant melanoma tumor progression. J Leukoc Biol 1997;62:588-97. 65. Ellis DL, King LE, Nanney LB. Increased epidermal growth factor receptors in melanocytic lesions. J Am Acad Dermatol1992;27:539-46. 66. Sparrow LE, Heenan PJ. Differential expression of epidermal growth factor receptor in melanocytic tumours demonstrated by immunohistochemistry and mRNA in situ hybridization. Australas J Dermatol 1999;40:19-24. 67. Wyman K, Atkins MB, Prieto V, et al. A multi-center Phase II trial of high-dose imatinib mesylate in metastatic melanoma: significant toxicity with no clinical efficacy cancer. Cancer, 2006; 106 (9): 2005-11 68. Tsao MS, Sakurada A, Cutz JC, et al. Erlotinib in lung cancer: molecular and clinical predictors of outcome. N Engl J Med 2005;353:133-44. 69. Boccadoro M, Morgan G, Cavenagh J. Preclinical evaluation of the proteasome inhibitor bortezomib in cancer therapy. Cancer Cell Int 2005;5:18. 70. Fernandez Y, Verhaegen M, Miller TP, et al. Differential regulation of noxa in normal melanocytes and melanoma cells by proteasome inhibition: therapeutic implications. Cancer Res 2005;65:6294-304. 71. Amiri KI, Horton LW, LaFleur BJ, Sosman JA, Richmond A. Augmenting chemosensitivity of malignant melanoma tumors via proteasome inhibition: implication for bortezomib (VELCADE, PS-341) as a therapeutic agent for malignant melanoma. Cancer Res 2004;64:4912-8. 72. Viloria-Petit A, Crombet T, Jothy S, et al. Acquired resistance to the antitumor effect of epidermal growth factor receptor-blocking antibodies in vivo: a role for altered tumor angiogenesis. Cancer Res 2001;61: 5090-101. 73. Sini P, Wyder L, Schnell C, et al. The Antitumor and antiangiogenic activity of vascular endothelial growth factor receptor inhibition is potentiated by ErbB1 blockade. Clin Cancer Res 2005;11:4521-32. 74. Gutheil JC, Campbell TN, Pierce PR, et al. Targeted antiangiogenic therapy for cancer using Vitaxin: a humanized monoclonal antibody to the integrin alphavbeta3. Clin Cancer Res 2000;6:3056-61. 75. Hingorani SR, Jacobetz MA, Robertson GP, Herlyn M, Tuveson DA. Suppression of BRAF(V599E) in human melanoma abrogates transformation. Cancer Res 2003;63:5198202. 76. Alsina J, Gorsk DH, Germino FJ, et al. Detection of mutations in the mitogenactivated protein kinase pathway in human melanoma. Clin Cancer Res 2003;9:6419-25. 77. Neshat MS, Mellinghoff IK, Tran C, et al. Enhanced sensitivity of PTEN-deficient tumors to inhibition of FRAP/mTOR. Proc Natl Acad Sci U S A 2001;98:10314-9. 78. Hidalgo HM, Rowinsky EK. The rapamycin-sensitive signal transduction pathway as a target for cancer therapy. Oncogene 2000;19:6680-6. 79. Tsao H, Zhang X, Benoit E, Haluska FG. Identification of PTEN/MMAC1alterations in uncultured melanomas and melanoma cell lines. Oncogene 1998;16:3397-402. 80. Nencioni A, Hua F, Dillon CP, et al. Evidence for a protective role of Mcl-1 in proteasome inhibitorinduced apoptosis. Blood 2004;105:3255-62. 21 81. Thompson N, Lyons J. Recent progress in targeting the Raf/MEK/ERK pathway with inhibitors in cancer drug discovery. Curr Opin Pharmacol 2005;5:350-6. 82. Burke JR, Pattoli MA, Gregor KR, et al. BMS-345541is a highly selective inhibitor of I kappa B kinase that binds at an allosteric site of the enzyme and blocks NF-kappa Bdependent transcription in mice. J Biol Chem 2003;278:1450-6. 83. Atkins MB, Hidalgo M, Stadler WM, et al. Randomized phase II studyofmultiple dose levels ofCCI-779, a novel mammalian target of rapamycin kinase inhibitor, in patients with advanced refractory renal cell carcinoma. J Clin Oncol 2004;22:909-18. 84. Margolin K, Longmate J, Baratta T, et al. CCI-779 in metastatic melanoma. Cancer 2005;104:1045-8. 85. Boulay A, Zumstein-Mecker S, Stephan C, et al. Antitumor efficacy of intermittent treatment schedules with the rapamycin derivative RAD001correlates with prolonged inactivation of ribosomal protein S6 kinase 1in peripheral blood mononuclear cells. Cancer Res 2004;64:252-61. 86. Rini BI, Sosman JA,Motzer RJ.Therapy targeted at vascular endothelial growth factor in metastatic renal cell carcinoma: biology, clinical results and future development. BJUInt 2005;96:286 -90. 22