Chapter No
advertisement

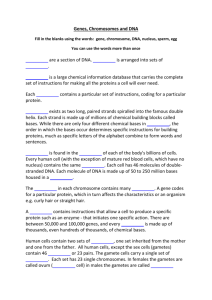
105 EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES CONTAINING DISINTEGRATION ACCELERATORS FOR THE FORMULATION OF METOCLOPRAMIDE ORALLY DISINTEGRATING TABLETS Fars K. Alanazi اكتسبت األقراص الفموية رةري التفتةت جةباً لهتتمةًأ ثك ةر اةق األقةراص التة خاية اًنة اًلمسةب ل مر ة الةبيق لايهم اشك في الب ع ا ل األطفًل وكبةً السةق والمر ة الممةواخق واخةر الةةً يق تةبص األقةراص تفتةت فةي الفةم ااون اضغ ثو إ ًف اخًص لهً في الفم إل اآلن تمًك ال ايا اق اةرااا اخاتةرال لهةبص األقةراص ولكةق تمةًك الة خةل فةة اةق األاثةًل الممشةو د تةةاث البثةي الثةًلي تةو ثضةخر ثقةةراص اختوك وارااخةا رةري التفتةت اةًلفم ا قةةود اخكًنخكخ كًفخ و فتت رريع اق قواعا اثضرد اًرةتدااأ ةمخةً التيمخةا اةًلرل والتيمخةا التيفخفةي ولةةا ارةتداات نةةو يوأ، ك و يةةون،رةةول- اي- اسةرعً ادت فة ل تفتةةت لتثضةةخر األقةةراص الفموية رةري التفتةةت فمويةةً ا ةةل ث اةةبيا يةةًيري تةةو الكثةةول األضخ ةةي والثمةةن األاخمةةي ج خسةةخق ولةةةا ارةةتداأ عةةةً اختوك وارااخةةا، نشةةًج خكوخ المضً ل ةخئ كةمم وايةي فةي األقةراص رةري التفتةت فمويةً المثضةرد ولةةا لةو أ ثن رةرع التفتةت الفمةوي فةي األقراص المثضرد ي تما ع اخرتفً د اق اسرعً التفتت فةي كةل اةق ةمخةً التيمخةا اةًلرل والتيمخةا التيفخفةي نةول،لتثضخر قواعا قرنخ لألقراص الفموي رري التفتت وكبلك ال واال المت ةا د األاةرم ا ةل عم خة التيفخةع اسرعً التفتت وإ ًف اسرعً التفتت قبل ثو ا ا عم خ التيفخع ولةا عزيت ررع التفتت لألقراص المثضةرد إل الترطخا الممتًز لمكونً الةرص ا ا ثن م ريضهً ل م خً التيفخع وقا بةخق ثنةب اا ةًف اسةرعً التفتةت إل قواعا األقراص قبل عم خ التيفخع يمتج عمب إطًل لوقت التفتت اةً ن اا ًفتهً إل قواعا األقراص ا ا عم خة التيفخع ويمكق يبخق تبص الا ار ع ث وي ثارم فةي نةخًاً رةري التفتةت تفتةت فةي التيويةع الفمةي و لةك لتهخئ ااتصًص ثررل اق يويع الفم وا ا لةك يكتمةل اخاتصةًص فةي اةخة اليهةًز الهضةمي وثيضةً ل ت ةا ع ة ن وا الب ع Orally disintegrating tablets (ODT) are gaining attractiveness over conventional tablets specially for patients having difficulty in swallowing such as pediatric, geriatric, bedridden and disable patients. ODT technologies render the tablets disintegrate in the mouth without chewing or additional water intake. So far there have been many patents for ODT, but only few publications are dealing with this dosage form. The aim of the present study was to formulate metoclopramide in ODT with sufficient mechanical strength and fast disintegration from bases prepared by both spray (SD) and freeze drying (FD) techniques. Different disintegration accelerators (DA) were utilized to prepare the proper ODT using various super-disintegrants (Ac-Di-Sol, Kollidon and sodium starch glycolate), a volatilizing solvent (ethanol) and an amino acid (glycine). Metoclopramide, an antiemetic medication, was used as a model drug in the formulated ODT. It was noted that the disintegration of ODT depends on utilization of DA in both SD and FD techniques to prepare tablet bases for ODT and so many other factors such as drying process, type of DA, and the addition of DA before or after the drying processes. The good disintegration property of the prepared tablets was related to the excellent wettability of the ingredients after being subjected to the drying processes. Results also showed that the addition of DA to the tablet bases before drying process results in lengthening of the disintegration time in comparison to their addition to the tablet bases after the drying process. These findings could be utilized for many Department of Pharmaceutics, College of Pharmacy, King Saud University, P.O. BOX 2457, Riyadh 11451, Saudi Arabia. Email: afars@ksu.edu.sa Saudi Pharmaceutical Journal, Vol. 15, No.2, April 2007 106 ALANAZI drugs and they may be considered versatile in the applications. Also, the disintegration of the ODT in the buccal cavity may favor fast absorption via the mucus membrane in the oral cavity. Key words: Spray drying, Freeze drying, Orally disintegration tablet, Metoclopramide, Disintegration accelerators, Dissolution rate, Super-disintegrants. Introduction Recent advances in drug delivery systems seek enhancing the safety and efficacy of drug molecules by formulating them in conveniently administrated dosage forms (1). Dysphagia, difficult in swallowwing, is common among all age groups and it is experienced by patients such as pediatric, geriatric, bedridden and disabled patients (2). The most common complaint about the difficulty in swallowwing of tablets is their large sizes (3). Therefore, improving the compliance and quality of life of such patients by using orally-fast disintegrating tablet is a promising alternative to conventional tablets (4). During the last decade, great deal of attention has been drawn to orally disintegrating tablet (ODT) technologies that make such tablets disintegrate in the mouth without chewing or additional water intake (5). These tablets disintegrate into smaller granules or melt in the mouth from a hard rigid solid to a gel like structure, allowing easy swallowing by patients. The saliva of patients (1-2 ml) is the dissolving medium and it would be enough to disintegrate these tablets (4). Orally disintegrating tablets (ODT) have been reported to be prepared by different technologies including molding, sublimation, direct compression, wet granulation, freeze drying and spray drying (6). So far there have been many patents for ODT, but only few publications are dealing with this dosage form (7). Spray drying (SD) and freeze drying (FD) are considered novel techniques to prepare excipients for ODT. SD technique provides a fast and economic way of evaporating solvents, subsequent drying and producing highly amorphous spherical, fine powders suitable for ODT (8). On the other hand, FD; lyophilization, is a process in which the solvent is sublimed from a frozen drug solution or suspension containing structure-forming excipients. Glassy amorphous porous structure of excipients as well as the drug substance produced with FD leading to the enhancing of dissolution (9). In the literature, there is no study comparing between SD and FD as techniques in the efficiency of preparation of ODT bases. In addition, there is lack of information about the effect of SD and FD Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 techniques on the efficiency of disintegration accelerators (DA). The aim of the present study was to formulate ODT with sufficient mechanical strength and fast disintegration from bases prepared by both SD and FD techniques. Different disintegration accelerators (DA) were also utilized to prepare the proper ODT using various super-disintegrants (Ac-Di-Sol, Kollidon and sodium starch glycolate), a volatile solvent (ethanol) and an amino acid (glycine). Metoclopramide, an antiemetic medication, was used in the present study as a model drug. It is administrated by group of patients who have motion sickness (10) and may not have an access to water at the time of administration. Examples of these patients are aeroplane passengers and pregnant women during walking. In the light of that, metoclopramide is a good candidate for ODT and formulating it in ODT is beneficial for certain patients. Materials and Methods Materials: Metoclopramide and glycine were purchased from Sigma (USA). Crosslinked sodium carboxymethyl cellulose (Ac-Di-Sol), sodium starch glycollate (SSG), and Kollidon CL (crosslinked polyvinyl pyrrolidone) were kindly donated from Al-Jazerah Pharm. Ind. (Riyadh, Saudi Arabia). All other chemicals and solvents used were of pharmaceutical grades. Methods A. Preparation of spray-dried tablet bases: Tablet bases, composed of microcrystalline cellulose, mannitol, saccharine and DA (Table 1), were suspended in deionized water and then heated to 40 oC bending to SD process. All batches of suspension bases were spray-dried using Buchi 190 mini spray drier (Büchi Labortechnik AG, Germany) with 0.5mm nozzle. The suspension bases were fed to the nozzle via peristaltic pump (spray flow rate of 12 ml/min.). The suspension was sprayed as atomized droplets by the force of the compressed air EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES (air flow rate of 4 pound per square inch). The solvent in the droplets was evaporated in the drying chamber by the blown hot air (inlet air temperature of 135 oC and outlet air temperature of 70 oC). The dried tablet bases were collected in collection vessel and stored at room temperature for further manipulation. B. Preparation of freeze-dried tablet bases: The tablet bases, composed of microcrystalline cellulose (MCC), mannitol, saccharine and DA (Table 1), were suspended in deionized water and the suspensions were heated to 40 o C. Suspension bases were pre-cooled (-5 o C) prior to FD. The frozen bases were lyophilized using freeze dryer (ALPHA 1-4LD-2, Martin Christ, Osterode, Germany) under the following conditions (temperature = -59, vacuum = 0.001 mp) for 48 hrs. The dried bases were collected and transferred to well-closed containers and stored at room temperature (25 o C) bending to evaluation and formulation experiments. C. Particle size analysis of the prepared tablet bases: The samples were dispersed in liquid paraffin (1 mg/ 1 ml) and mounted on microscopic slides. Particle diameters of the bases were measured using Reichert Microscope (Depew, NY, USA) and using eyepiece of magnification of 40X. The microscope is equipped with a special projection system connected to the eyepiece which allows the measurement on the surface of the projection screen. The readings were measured in millimeter and converted to micrometer using the microscope provided equation [diameter (m) = measurement in mm X (1000/ magnification power)]. The diameters measured are number parameters (i.e. numbers distribution) (11). The mean particle diameters were the average of at least 100 particles. D. Measurement of Angle of repose of the prepared tablet bases: The angle of repose was measured for the SD and FD bases, so as to observe the flow properties of such bases. The method employed a funnel secured with its tip at a given height (H), above the graph paper placed on horizontal surface. Treated base powders were poured through the funnel until the apex of conical pile touched the tip of the funnel. The angle of repose was calculated using the following formula, tan = H/R where is the angle Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 107 of repose and R is the radius of conical pile (12). The angle of repose was calculated as the mean of three determinations. E. Determination of moisture content of the prepared tablet bases: Weight loss on drying was determined using a Mettler moisture balance (Meltter PM 480 Delta Range, Switzerland). Five gms of each prepared base powder was put in the pan of the balance. Heating temperature was set at 100 oC and the time mode was set at 30 seconds which means continuous heating of the sample after removal of the free water content for the 30 seconds (13). The percentage moisture content was directly recorded. The test was carried out on triplicate for each base and the mean values were considered. F. Determination of bulk density and compressibility of the prepared tablet bases: The bulk density was determined by filling the processed base powders into a tarred graduated cylinder to the 100 ml mark. The graduated cylinder was weighed and the bulk density (VB) was calculated as the ratio of the sample weight to the sample volume (14). The graduated cylinders were then tapped (for 3 mins which was found practically to be enough time) from a height of about 2 inches till constant volume was obtained. The tap density (VT) was calculated as the ratio of the sample weight to the final sample volume. The trial was carried out on triplicate and the mean values were calculated. Carr’s Index and Hausner factor were calculated for the prepared ODT bases as evaluation parameters for compressibility (15). The changes occurring in packing arrangement during the tapping procedure were expressed as Carr’s Index (I) as shown by the following equation , I = [( 1- VB)/ VT] X 100. Hausner factor (HF) was calculated from the following equation, HF = VT/ VB. G. Scanning electron microscopic (SEM) examination for the prepared bases: SD and FD tablet base morphologies were examined under the scanning electron microscope (Jeol, JSM-6360LV scanning microscope, Tokyo, Japan). Before microscopy, the base powders were mounted at carbon tape and were sputter-coated using gold (Jeol, JFC-1100 fine coat ion sputter, Tokyo, Japan). The photomicrographs were taken at an acceleration voltage of 20 kV (16). 108 ALANAZI H. Preparation of ODT by direct compression technique: The ODT were prepared using the SD and FD processed bases after the addition of metoclopramide and sodium stearyl fumarate (SSF), (Table 1). The tablet constituents were weighed and mixed first in the mortar (triturating) and mixed furtherly in tubula mixer (Erweka S27, Frankfort, Germany) for 2 mins which was found practically as the efficient mixing time. The tablet ingredients after mixing were compressed by EKO single punch tablet machine (Korsch, Berlin, Germany) using punch 0.6 cm in diameter and weighing 110 mg. I. Determination of the prepared ODT hardness: The hardness of the ODT was measured using Erweka TBH-28 hardness tester (Frankfort, Germany). Hardness is the breaking strength value of the tablet reported in kilograms (12). Minimum of six tablets were used and the mean value was considered. J. Determination of the prepared ODT friability: Friability (f) of the tablets was determined using Erweka TA3R friabilitor (Frankfort, Germany) at 25 rpm/min for 4 min. The tablets were weighed and loss in weight (%) was calculated (17). Twenty tablets were used in such determination. K. Determination of wetting time for the prepared ODT: Wetting time was determined by the method described previously (18). In brief, a piece of tissue paper folded twice was placed in small culture dish (internal diameter = 6.5 cm) containing 6 ml of water. Then, the tablet was placed on the wetted paper and the time for complete wetting was calculated. The test was carried out on triplicate and the mean value was considered. L. Measurement of disintegration time for the prepared ODT: Disintegration time was determined using USP disintegration test apparatus (Erweka ZT4, Frankfort, Germany) without disk for six tablets. The disintegration medium was 900 ml of distilled water kept at 37 ± 0.5 oC and stirred at a rate of 30 ± 2 cycles/ min (13). M. Measurement of in vitro drug dissolution from the prepared ODT: The dissolution measurements were performed Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 using USP dissolution apparatus II (Caleva Ltd., Model 85T, Philips, UK) adopting a continuous automated monitoring system which consists of an IBM computer PS 830 series and PU 860/60 dissolution test software, Philips VIS/UV single beam, six cells, spectrophotometer model PU 8620, Epson FX 850 printer, and Waston-Marlow peristaltic pump. In each flask, 1 L of distilled water was used as the dissolution medium (USP 23). The temperature was maintained at 37 ± 0.5 oC and paddles speed was kept at 50 rpm. Percent drug dissolution was determined at specified time intervals by assaying the collected samples spectrophotometerically for drug content at 308 nm (19). It was found that all additives included in the tablet formulation didn’t interfere with the spectrophotometric assay of the drug. The dissolution studies were carried out in triplicate. The time required for 50% of the drug to be dissolved (T50 %) was calculated graphically (16) which was used as a comparison parameter in drug dissolution evaluation. Relative dissolution rate (RDR) was obtained by dividing the dissolution percent of the drug in the specific formula at the determined time by the dissolution percent of the pure drug which processed under the same condition (SD and FD) at the same time. Dissolution efficiency (DE) is defined as the area under dissolution curve up to the time (t) which was expressed as a percentage of the area of the rectangular described by 100 % dissolution in the same time (10). N. Statistical analysis of the obtained results: One-way analysis of variance (ANOVA) and ttest were performed using Statgraphics plus 2 software to compare the mean values for all formulations. Multiple Range Test (Fisher’s least significant difference procedure, LSD) was also used to determine which means are significantly different from the others. The level of confidence was set to be 95% (20). Results and Discussions SD technique yielded spherical particles as shown in Fig 1. However, in case of FD technique the products were in the form of spongy matrices with very porous structures. Exception to these findings is in case of glycine, SD powder is not spherical but tubular like structure (Fig 2: SD-F). It was also observed that SD powder containing SSG is EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES spherical in shape (Fig 2: SD-B2), yet their base surface is not smooth like the rest of superdisintegrants (Fig 1: SD-B1 and SD-B3). This surface is composed of small tubular particles joined together to form bigger spherical particles. This could be because SSG may adsorb water during its presence in the sprayed suspension which results in resistance in water removal by SD due to SSG high water affinity. This finding can be also supported by the data obtained from the moisture content (Table 2) in which SSG has the highest moisture content 109 (1.8 %) compared to other SD bases. It worth mentioning that the particle morphology, structure and shape of these bases affect their compressibility into tablets and consequently tablet properties. Photomicrographs taken by scanning electron microscopy for the prepared ODT base particles show differences in morphologies of SD and FD particles compared to that of controls. This difference may lead to variation in the interaction with water as well as differences in water solubility and disintegration. Table 1: Formulation of orally disintegrating tablets of metoclopramide. Formulations Tablet Drug (mg) A1 A2 A3 B1 B2 B3 C D E F 10 10 10 10 10 10 10 10 10 10 MCC Mannitol Ac-Di-Sol (mg) (mg) (mg) 10 10 10 10 10 10 10 10 10 10 84.9 84.9 84.9 84.9 84.9 84.9 89.9 89.9 89.9 84.9 5 — — 5 — — — — — — SSG (mg) Kollidon CL (mg) Volatilizing agent % * Amino acid (mg) SC (mg) SSF (mg) Total tablet Formula weight (mg) — 5 — — 5 — — — — — — — 5 — — 5 — — — — — — — — — — 10 % — — — — — — — — — — — — 5 0.1 0.1 0.1 0.1 0.1 0.1 0.1 0.1 0.1 0.1 0.2 0.2 0.2 0.2 0.2 0.2 0.2 0.2 0.2 0.2 110.2 110.2 110.2 110.2 110.2 110.2 110.2 110.2 110.2 110.2 MCC= microcrystalline cellulose, Ac-Di-Sol = crosslinked sodium carboxymethyl cellulose, SSG = sodium starch glycolate, SSF = sodium stearyl fumarate, Amino acid = glycine, Volatilizing agent = ethanol. SC= saccharine * ethanol added to suspending medium (water) in v/v %. A = disintegrants added after drying process. B = disintegrants added before drying process. C = ethanol composed of 10 % suspending medium before drying. D = bases alone (negative control). E = bases alone dried by freezing and spraying techniques (positive control). F =amino acid added to the bases before drying. Figure 1. Photomicrographs taken by scanning electron microscope for the prepared excipient bases. B1 and B3: formulations containing ODT bases and superdisintegrants Ac-Di-Sol and Kollidon CL. FD: freeze-dried base. SD: spray-dried base Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 Figure 2. Photomicrographs taken by scanning electron microscope for the prepared excipient bases. C, B, and F: formulations containing ODT bases and with alcohol treatment (C) , the super-disintegrant SSG (B2) , glycine (F). FD: freeze-dried base. SD: spray-dried base. 110 ALANAZI Table 2: Physical characterization of the SD and FD prepared tablet bases Base symbols B1 SD-B1 FD-B1 B2 SD-B2 FD-B2 B3 SD-B3 FD-B3 SD-C FD-C D SD-E FD-E SD-F FD-F Particle size ( 77.9 ±37.1 119 ±9.5 128 ±11.5 71.1 ±36.4 207 ±18.3 169 ±15.2 70.8 ±36.2 212.8 ±19.1 191.7 ±17.2 52.67 ±4.7 144.1 ±12.8 104 ±9.6 127.9 ±10.2 117 ±9.3 86.5 ±7.7 179.4 ±16.2 Ø 44.57 ±1.13 44.83 ± 0.45 45.32 ± 0.78 45.76 ± 0.44 36.6 ± 0.43 49.02 ± 1.44 44.62 ± 0.15 37.3 ± 1.28 50.2 ± 0.58 49.9 ± 0.43 47.6 ± 0.57 46.2 ± 0.92 45.8 ± 0.57 49.7 ± 0.75 44.6 ± 0.16 46.6 ± 1.2 Carr’s index % 37.08 ± 1.0 38.37 ± 0.38 39.89 ± 0.16 37.08 ± 2.18 33.3 ± 0.9 46.1 ± 1.06 41.3 ± 1.81 37.42 ± 1.48 44.37 ±0.52 27.3 ± 0.08 53.58 ± 1.09 35.13 ± 0.5 43.01 ± 0.45 44.5 ± 0.44 22.6 ± 1.1 23.6 ± 1.01 Hausner factor 1.58 ± 0.02 1.61 ± 0.02 1.66 ± 0.01 1.58 ± 0.04 1.50 ± 0.01 1.85 ± 0.03 1.70 ± 0.03 1.59 ± 0.04 1.82 ± 0.03 1.38 ± 0.01 2. 15 ± 0.05 1.54 ± 0.01 1.75 ± 0.01 1.8 ± 0.02 1.29 ± 0.02 1.31 ± 0.02 Moisture content % 1.1 ± 0.1 1.1 ± 0.2 1.2 ± 0.3 1.1 ± 0.1 1.8 ± 0.1 2.1 ± 0.3 1.1 ± 0.1 1.00 ± 0.1 0.99 ± 0.1 1.1 ± 0.1 1.1 ± 0.2 1.00 ± 0.1 1.1 ± 0.1 1.1 ± 0.3 1.1 ± 0.1 1.1 ± 0.1 Technique Spray drying Tablet Formula symbol Disintegration time (s) SD-A1 15 ± 4.0 SD-B1 53.33 ± 20.6 SD-E 50 ± 5.0 FD-A1 13 ± 2.0 FD-B1 45.83 ± 21.5 FD-E 60 ± 7.0 Freeze drying B 80 60 40 20 0 20 25 30 35 40 Wetting time (s) Disintegration time (s) A Disintegration time (s) FD = freeze dried base. SD = spray dried base, Ø= angle of repose. B1, B2 and B3= formulations containing metoclopramide and super-disintegrants Ac-Di-Sol, SSG, and kollidon, respectively. B = disintegrants added before drying process. C= ethanol composed 10 % of suspending medium before drying. D= bases alone (negative control). E= bases alone dried by freezing and spraying techniques (positive control). F= amino acid added to the bases before drying. 80 C 60 40 20 0 3.2 3.4 3.6 3.8 4 0.36 0.48 Hardness (kg) B1 60.83 ± 9.1 D 70 ± 8.0 D 80 Disintegration time (s) Controls 60 40 20 0 0 0.12 0.24 Friability % Figure 3. disintegration time of ODT containing metoclopramide and the super-disintegrant Ac-Di-Sol (A), disintegration time of the tablets as a function of wetting time (B), disintegration time of the tablets as a function of hardness (C), disintegration time of the tablets as a function of friability (D). Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 A Technique Tablet Formula symbol Disintegration time (s) SD-A2 Disintegration time (s) EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES 111 B 150 100 50 0 19.2 ± 3.7 15 30 45 60 75 SD-B2 63.33 ± 12.1 SD-E 50 ± 5.0 FD-A2 22.8 ± 3.1 FD-B2 135 ± 13.7 FD-E 60 ± 7.0 B2 42.5 ± 9.8 D 70 ± 8.0 Freeze drying Controls C 150 100 50 0 3.2 3.4 3.6 3.8 4 4.2 Hardness (kg) Disintegration time (s) Spray drying Disintegration time (s) Wetting time (s) D 150 100 50 0 0 0.1 0.2 0.3 0.4 0.5 Friability % A Technique Tablet Formula symbol Disintegration time (s) SD-A3 18 ± 2.1 SD-B3 51.67 ± 21.1 Disintegration time (s) Figure 4. disintegration time of ODT containing metoclopramide and the super-disintegrant sodium starch glycolate (SSG) (A), disintegration time of tablets as a function of wetting time (B), disintegration time of tablets as a function of hardness (C), disintegration time of tablets as a function of friability (D). B 100 75 50 25 0 0 SD-E 50 ± 5.0 FD-A3 18.1 ± 3.1 Freeze drying FD-B3 16.67 ± 2.5 FD-E 60 ± 7.0 B3 70.83 ±16.8 D 70 ± 8.0 30 45 60 C 100 75 50 25 0 3.3 3.4 3.5 3.6 3.7 3.8 3.9 4 Hardness (kg) Disintegration time (s) Controls 15 Wetting time (s) Disintegration time (s) Spray drying D 80 60 40 20 0 0 0.2 0.4 0.6 Friability % Figure 5. disintegration time of ODT containing metoclopramide and the super-disintegrant kollidon (A), disintegration time of tablets as a function of wetting time (B), disintegration time of tablets as a function of hardness (C), disintegration time of tablets as a function of friability (D). Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 112 ALANAZI B Disintegration time (s) 150 A 90 60 30 0 Disintegration time (s) SD-C 120 ± 2.0 SD-E 50 ± 5.0 FD-C 25 ± 6 FD-E 60 ± 7.0 D 70 ± 8.0 Spray drying Freeze drying 0 50 100 150 200 250 Wetting time (s) C 150 Disintegration time (s) Technique Tablet Formula symbol 120 120 90 60 30 0 3.5 Control 3.6 3.7 3.8 3.9 4 Hardness (kg) D Disintegration time (s) 150 120 90 60 30 0 0 0.15 0.3 0.45 0.6 Friability % Disintegration time (s) Figure 6. disintegration time of ODT containing metoclopramide and ethanol as a volatile agent (A), disintegration time of tablets as a function of wetting time (B), disintegration time of tablets as a function of hardness (C), disintegration time of tablets as a function of friability (D). A Disintegration time (s) SD-F 205 ± 10 SD-E 50 ± 5.0 FD-F 170 ± 8 FD-E 60 ± 7.0 200 150 100 50 0 0 Spray drying Freeze drying 30 60 90 120 150 Wetting time (s) Disintegration time (s) Technique Tablet Formula symbol B 250 250 C 200 150 100 50 0 3.5 3.6 3.7 3.8 3.9 Hardness (kg) 18 ± 2.0 D 70 ± 8.0 Disintegration time (s) G Controls 250 D 200 150 100 50 0 0.15 0.3 0.45 0.6 Friability % Figure 7. disintegration time of ODT containing metoclopramide and glycine as disintegration adjuvant (A), disintegration time of tablets as a function of wetting time (B), disintegration time of tablets as a function of hardness (C), disintegration time of tablets as a function of friability (D). G= glycine was added to the tablet base after drying (positive control). Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES 113 A T 50 % (min) 4 3.5 3 2.5 2 1.5 1 0.5 0 SD-A1 B Tablet Formulation FD-A1 SD-B1 PD 5 min RDR 5 min FD-B1 C 100 DE 10 min B1 SD-A1 85.2 91.6 26.8 SD-B1 76.1 81.7 23.9 FD-A1 74 79.5 24.3 FD-B1 81.8 87.9 24.9 B1 69.1 74.2 22.6 % Released 80 60 SD-A1 SD-B1 40 FD-A1 FD-B1 20 B1 0 0 5 Time (min) 10 Figure 8. In vitro dissolution parameters of ODT formed from spray dried and freeze dried excipient bases and super-disintegrant Ac-Di-Sol. (A) T50 % data which is the time in which 50% of the drug was released., (B) PD is the percent drug dissolution at 5 min, RDR is the relative dissolution rate in 5 min in comparison to pure drug, DE is the dissolution efficiency, (C) dissolution profiles. SD-A1 = disintegrants added after spray drying process, SD-B1= disintegrants added before spray drying process, FD-A1= disintegrants added after freeze drying process, FD-B1= disintegrants added before freeze drying process, B1= control consist of base plus AC-Di-Sol without drying. A T 50 % (min) 3 2.5 2 1.5 1 0.5 0 SD-A2 Tablet Formulation SD-B2 FD-A2 FD-B2 RDR 5 min DE 10 min SD-A2 97.6 100 26.9 SD-B2 96.7 100 26.8 FD-A2 97.5 100 26.8 FD-B2 89.5 96.2 25.9 B2 87.8 94.4 25.6 B2 C 100 PD 5 min % Released B 80 60 SD-A2 SD-B2 40 FD-A2 FD-B2 20 B2 0 0 5 Time (min) 10 Figure 9. In vitro dissolution parameters of ODT formed from spray and freeze dried excipient bases and super-disintegrant SSG. (A) T50 % data which is the time in which 50% of the drug was released, (B) PD is the percent drug dissolution at 5 min, RDR is the relative dissolution rate in 5 min in comparison to pure drug, DE is the dissolution efficiency, (C) dissolution profiles. SD-A1 = disintegrants added after spray drying process, SD-B1= disintegrants added before spray drying process, FD-A1= disintegrants added after freeze drying process, FD-B1= disintegrants added before freeze drying process, B1= control consists of base plus SSG without drying. Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 ALANAZI T 50 % (min) 114 A 3.5 3 2.5 2 1.5 1 0.5 0 SD-A3 SD-B3 FD-A3 FD-B3 B3 B C 100 PD 5 min RDR 5 min DE 10 min SD-A3 98.1 100 29.8 SD-B3 87.3 93.8 25.5 FD-A3 98.9 100 29.9 FD-B3 98.8 100 27.1 B3 77.5 83.3 24.1 % Released Tablet Formulation 80 SD-A3 60 SD-B3 40 FD-A3 FD-B3 20 B3 0 0 5 10 Time (min) Figure 10. In vitro dissolution parameters of ODT formed from spray dried and freeze dried excipient bases and super-disintegrant Kollidon. (A) T 50 % data which is the time in which 50% of the drug was released, (B) PD is the percent drug dissolution at 5 min, RDR is the relative dissolution rate in 5 min in comparison to pure drug, DE is the dissolution efficiency, (C) dissolution profiles. SD-A1 = disintegrants added after spray drying process, SD-B1= disintegrants added before spray drying process, FD-A1= disintegrants added after freeze drying process, FD-B1= disintegrants added before freeze drying process, B1= control consists of base plus Kollidon without drying. A T 50 % (min) 5 4 3 2 1 0 SD-C Tablet Formulation FD-C SD-E FD-E 100 PD 5 min RDR 5 min SD-C 62.2 66.8 20.9 FD-C 95.2 100 28.4 SD-E 78.2 84.1 22.8 FD-E 84.7 91.1 25.4 D 89.5 96.2 24.5 D C DE 10 min % Released B 80 SD-C 60 FD-C 40 SD-E FD-E 20 D 0 0 5 10 Time (min) Figure 11. In vitro dissolution parameters of ODT formed from spray dried and freeze dried excipient bases and alcohol as a volatile agent. (A) T 50 % data which is the time in which 50% of the drug was released, (B) PD is the percent drug dissolution at 5 min, RDR is the relative dissolution rate in 5 min in comparison to pure drug, DE is the dissolution efficiency, (C) dissolution profiles. SD-A1 = disintegrants added after spray drying process, SD-B1= disintegrants added before spray drying process, FD-A1= disintegrants added after freeze drying process, FD-B1= disintegrants added before freeze drying process, B1= control consists of base alone without drying. Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES 115 T50 % (min) A 6 5 4 3 2 1 0 SD-F FD-F G B % Released 100 C 80 Tablet Formulation PD 5 min RDR 5 min DE 10 min SD-F 54.5 58.6 20.7 FD-F 55.6 59.7 21.6 20 G 86 92.5 27.1 0 60 SD-F 40 FD-F G 0 5 10 Time (min) Figure 12. In vitro dissolution parameters of ODT formed from spray dried and freeze dried excipient bases and glycine as a disintegrant. (A) T 50 % data which is the time in which 50% of the drug was released, (B) PD is the percent drug dissolution at 5 min, RDR is the relative dissolution rate in 5 min in comparison to pure drug, DE is the dissolution efficiency, (C) dissolution profiles. SD-A1 = disintegrants added after spray drying process, SD-B1= disintegrants added before spray drying process, FD-A1= disintegrants added after freeze drying process, FD-B1= disintegrants added before freeze drying process, B1= control consists of base and glycine without drying. The prepared ODT bases were evaluated for their physical characteristics (Table 2). The mean particle diameters of the prepared ODT bases were in the range of 70. 8 to 212 m (Table 2). The results revealed size enlargement after SD or FD as indicated by larger particle size of both SD and FD products compared with the corresponding control (unprocessed mixture). Flow properties of the powder, resistance to particle movement, can be judged from the angle of repose. This measurement gives qualitative and quantitative assessment of the internal cohesive and frictional force under low levels of external loading, as might be applied in mixing and tableting. Values of angle of repose < 40 o indicate good flow potential and values > 50 o indicate poor flow properties (17). Values for angle of repose for SD and FD treated bases were found in the range of 36.6 to 50.2 o, showing that the prepared bases have reasonable flow properties. Thus, these bases can be used for tablet manufacture. The SD excipient bases show lower angle of repose (better flow properties) than the FD excipient bases (Table 2), which is probably due to the spherical structure of the SD prepared bases (21). Controversy of this was observed in case of bases Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 containing volatilizing agent (SD-C and FD-C) in which the angle of repose was lower in the FD excipient bases. No distinct pattern could be obtained between presence of disintegratingadjuvant (i.e. super-disintegrants, a volatilizing agent, and an amino acid) and the flow properties. Compressibility index (Carr’s index) of the ODT prepared bases falls in the range of 33.3 and 53.58 % indicating some kind of complexity in compressibility of the prepared bases. This was also supported by Hausner factor values which were in the range of 1.5 and 2.15. Moisture content values of the different bases were very minute and readings were around 1 %. Exception to that was observed in formulation containing SSG which showed values around 2 % indicating a relatively high moisture content which could adversely affect the flowability. Direct compression technique was adopted for the preparation of ODT because it is the cheapest, easiest and the fastest tableting technique. Also, it is considered the best method to prepare ODT since the prepared tablets might be of higher disintegration due to absence of binder and low moisture content. The prepared tablets were evaluated for their hardness and friability. Mechanical integrity is of paramount importance in successful formulation of 116 ODT. Thus the hardness of the tablets was determined and was found to be in the range of 3.4 to 4 kg. Friability of the tablets was observed between 0.11–0.48 %, which was below 1% indicating sufficient mechanical integrity and strength of the prepared tablets. Wetting time is used as an indicator for the ease of the tablet disintegration in the buccal cavity (10). It was observed that the wetting time of the prepared tablets is in the range of 15.1 to 220 seconds. It has been noted in all cases that the addition of DA to the tablet bases before drying process results in elongation of the wetting time in comparison to their addition to the tablet bases after passing the drying process which causes the reverse (p < 0.05). That is because addition of DA through drying processing of these tablet bases minimizes their wetting efficiency as they become hydrated through processing. Additionally, results show that on comparing super-disintegrants the bases containing sodium starch glycolate (SSG) prepared by SD and FD processes take more wetting time (23.7 % and 50.1 %, respectively, calculated as percentage increment) than that of Ac-Di-Sol and Kollidon. Wetting is related to the inner structure of the tablets and the hydrophobicity of the components. This may be due to the fact that SSG is disintegrated by swelling mechanism leading to longer wetting time. Kollidon and Ac-Di-Sol perform their disintegrating action by wicking through capillary action and fibrous structure, respectively, with minimum gelling (22). Also, the effect of passing of the super-disintergrants through drying processing was maximum for SSG bases, in which the adsorbed moisture could decrease its dryness and swelling mechanism and consequently lengthens its wettability (Table 2). Results also show that the addition of superdisintegrants to SD or FD treated bases (after drying) leads to shorten the wetting time of prepared tablets in comparison to their addition to non-dried bases (formula B1, B2 and B3) (p < 0.05). This finding is explained by the results derived from the comparison in wetting time between bases alone dried by SD and FD techniques (positive controls, SD-E and FD-E) and bases alone without drying (negative control, D), which yields shortening in the wetting time of prepared tablets by 7.9 % for SD and 10.5 % for FD due to the drying process alone without addition of DA. Meaning that drying the tablet base by SD and FD also assists in fastening the wetting time. Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 ALANAZI Surprisingly, the addition of the volatilizing agent (ethanol) results in lengthening of the wetting time to 220 ± 16 seconds for SD bases perhaps due to more binding of the base, while it results in shortening of the wetting time to 27.1 ± 1.1 seconds for FD bases in comparison to 35 ± 4 seconds and 34 ± 3 seconds in case of positive spray (SD-E) and freeze dried (FD-E) controls, respectively, which may be explained by the wider spongy holes caused by the volatilization of ethanol by FD technique. Also, results show that the addition of the amino acid (glycine) before drying of the bases results in elongation of wetting time significantly (p< 0.05). For SD bases containing glycine, wetting time was 130 ± 14 seconds and for that of FD was 61 ± 13 seconds. Notably, the wetting time was very short (22 ± 3 seconds) when glycine was added to the base after drying. These results indicate that glycine is a good DA when added to dried bases. However, the addition of glycine before SD or FD process leads to passing it through contacting as well as solublizing in water and thus producing complex-dried particles. The production of these particles could make changes in glycine properties as DA consequently. Glycine was reported to enhance wetting of the tablet due to its polar surface free energy which comprises about 75 % of its component (23). As results of its presence in solution and drying process after that, the packing of glycine molecules in dried base particles may lead to reduction or minimization of the action of polar component and consequently the wetting of the tablet. Disintegration time is very important for ODT which is desired to be less than 60 seconds for ODT (10). That is because rapid disintegration in ODT assists swallowing conveniently. It may also play a role in assistance of drug absorption to take place in the buccal cavity, thus promoting its bioavailability. Disintegration time was found in the range of 15 - 205 seconds (Figs 3 - 7). Results show that the addition of DA to the tablet bases before drying process results in lengthening of the disintegration time in comparison to their addition to the tablet bases after passing the drying process (p < 0.05). That is because of the effect of drying processes on their wetting action and disintegration efficiency as a result. For the super-disintegrants, results show that disintegration time was in order of Kollidon < AcDi-Sol < SSG for both SD and FD bases when EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES super-disintegrants added before drying process (difference is statistically insignificant, p < 0.1). Results of disintegration time for adding superdisintegrants after drying of the tablet bases resulted in a similar rank Ac-Di-Sol < Kollidon < SSG in which tablets made from SSG gave the longest disintegration time (p < 0.05). This finding is in agreement with the results obtained from wetting time since SSG swells with more gelling than AcDi-Sol and Kollidon which extend wetting and disintegration times as a result. Results also show that the addition of the investigated super-disintegrants to the SD or FD bases (after drying) leads to a shortening the disintegration time of prepared tablets in comparison to their addition to non-dried bases (formula B1, B2 and B3) (p < 0.05). This finding is in agreement with wetting time data. This observation can be explained by the results derived from the comparison in disintegration time between bases alone dried by SD and FD techniques (positive controls, SD-E and FDE) and bases alone without drying (negative control, D), which yields shortening of the disintegration time of the prepared tablets by (28.5 % for SD and 14.3 % for FD) due to drying process alone without addition of DA. Meaning that drying the tablet base by SD and FD also assists in fastening of disintegration time. Notably, the presence of a volatilizing agent with FD process decreases disintegration time by 41.6 % (FD-C), while with SD process increases disintegration time by 140 % (SD-C) in comparisons with controls (Fig 6-A). That is because residual ethanol may cause strong binding of the ingredients in case of SD bases which results in delaying disintegration time. Oppositely, in case of FD the complete removal of ethanol causes more porosity in the matrix thus shortening of the disintegration time more than the controls (SD-E and FD-E) (p < 0.05). Also results show that the addition of the amino acid (glycine) before drying of the bases results in elongation of disintegration time significantly (p < 0.05) (Fig 7). For SD treated bases containing glycine, disintegration time was 205 ± 10 s (SD-F) and for that of FD was 170 ± 8 s (FD-F). Notably, the disintegration time was very short (18 ± 2 seconds) when glycine was added to the base after drying (p < 0.05) (Fig 7-A). That is because when glycine is added after the drying process, it didn’t loose its disintegrating properties. These results indicate that glycine is a good DA when added to Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 117 dried bases. However, addition of glycine before spray or freeze drying process leads to its passing through contacting as well as solublizing in water thus producing complex-dried particles. The production of these particles could make changes in glycine properties as DA consequently. Glycine was reported to enhance disintegration of the tablet due to its dispersion surface free energy which is comprises about 25 % of its component (23). As results of its presence in solution and drying process after that, the packing of glycine molecules in dried base particles may lead to reduce or minimize the action of dispersion component. The relationship between tablet wetting time and tablet disintegration time is shown in Figs 3-7, part B. It is observed that the tablets with the shortest wetting time have the minimum disintegration time. Also, the results show a good correlation between disintegration time and wetting time. In addition the strongest correlation was found for glycine bases (r2 = 0.817). Disintegration time as a function of hardness is presented in Figs 3-7, part C. It is observed that the tablets with the least hardness have the minimum disintegration time. Also, results show a good correlation between disintegration time and hardness. In addition, the highest correlation was found for kollidon bases )r2 = 0.834). The relationship between tablet friability and tablet disintegration time is shown in Figs 3-7, part D. It is observed that the tablets with the least friability have the minimum disintegration time. That is because the friability values of the prepared tablets are very near to each other and lie between 0.11 and 0.48. Also, results show a good correlation between disintegration time and friability. In addition, the highest correlation was found for ethanol treated bases )r2 = 0.637). In vitro drug dissolution studies are presented in Figs 8-12. For the super-disintegrants, results show maximum dissolution when they were added after SD or FD for the tablet bases compared to their addition to the bases before the drying process. That is because addition of the super-disintegrants through the processing of these bases (before drying) may lead to minimization of their efficiency as DA by decreasing their affinity to adsorb water and consequently decreasing their swelling behavior. T50 % is used as a comparison parameter for the dissolution in this study (16). It was found in the range of 0.83 – 3.3 min (Figs 8-10, part A). T50 % was the least when super-disintegrants were added 118 ALANAZI after SD or FD of the tablet bases (p < 0.05). Relative dissolution rates (RDR5 min) at 5 min and dissolution efficiencies (DE 10) of the tablets were maximum with the addition of super-disintegrants after SD or FD process (Figs 8-10, part B). This finding is in agreement with the results obtained from wetting and disintegration time evaluations. The more rapidly wetted and the more rapidly disintegrated tablets exhibited faster dissolution. Presence of ethanol in the SD process (i.e. before drying) resulted in delaying of the dissolution rates, while with FD process resulted in expedite the dissolution rate in compassion with the controls (Fig 11) (p < 0.05). T 50 % was the longest when ethanol present with SD process (4.1 min) and the least with freeze drying process (1.4 min) (p < 0.05), (Fig 11, part A). Relative dissolution rates at 5 min (RDR5 min) and dissolution efficiencies (DE 10) of the tablets were maximum (100 and 28.4, respectively) with the presence of ethanol in the freeze drying process (p < 0.05) (Fig 11, part B). These results also are in agreement with the results obtained from wetting and disintegration time evaluations. The effect of the addition of the amino acid (glycine) before drying processes on dissolution rate is presented in Fig 12. The addition of the amino acid before drying of the bases resulted in delaying of dissolution rate significantly (p < 0.05). T 50 % was the longest when glycine was added with SD (4.5 min) and FD (4.2 min) processes, (Fig 12, part A). T50 % was minimum (1.5 min) when glycine was added to the dried base (p < 0.05). Relative dissolution rates at 5 min (RDR5 min) and dissolution efficiencies (DE 10) of the tablets were minimum with addition of the amino acid before drying of the bases. Also, this is in agreement with results obtained from wetting and disintegration time evaluations. The more wetted and the more disintegrated tablets exhibited faster dissolution. Conclusion The methods adopted to prepare ODT bases via SD or FD techniques were successful to dry the excipient bases. Rapidly oral disintegrating tablets containing certain various super-disintegrants, a volatile solvent (ethanol) and an amino acid (glycine) using SD and FD techniques have been prepared successfully using direct compression technique. It was concluded that utilization of DA and both SD and FD techniques to prepare tablet Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 bases for ODT depends on so many factors such as type of DA, drying process and the mode of superdisintegrant addition (before or after drying processes). The good disintegration property of the tablets was closely related to the excellent wetting nature of the ingredients after passing the drying processes. These findings could be applied and utilized for many drugs and they may be considered versatile in the preparation of ODT. Acknowledgment The author would like to thank Dr. Gamal Mahrous for his help in running some experiments in base and tablet evaluations. Also, the gratitude is extended to Al Jazerah Pharmaceutical Industries (Riyadh, Saudi Arabia) for their kind support by gifting the super-disintegrants. References 1. Carpay J, Schoen J., Ahmed F., Kinrade F., Boswell D., Efficacy and tolerability of sumatripian tablets in a fastdisintegrating, rapid-release formulation for acute treatment of migraine: results of a multicenter, randomized, placebocontrolled study. Clin. Therapeut. 2004, 26: 214-223 2. Seager H, Drug-delivery products and the Zydis fastdissolving dosage form. J. Pharm. Pharmacol. 1998, 50:375382 3. Dobetti L. Fast-melting tablet: development and technologies. Pharm. Technol. N. Am. 2001; Suppl:44-50. 4. Fu Y, Yang S, Hoon-Jeong S, Kimura S, Park K, Orally fast disintegrating tablets: development, technologies, taste masking and clinical studies. Critical review therapeutic drug carrier systems 2004, 21: 433-475 5. Shu T, Suzuki H, Hironaka K, Lto K, Studies of rapidly disintegrating tablets in the oral cavity using co-grinding mixtures of mannitol with crospovidone. Chem. Pharm. Bull. 2002, 50:193-198. 6. Habib W, Khankari RK, Hontz J, Fast-dissolving drug delivery systems. Critical review therapeutic drug carrier systems 2000, 17: 61-72 7. Fukami J, Yonemochi E, Yoshihashi Y, Terada K, Evaluation of rapidly disintegration tablets containing glycine and carboxy methylcellulose. Inter. J. Pharm. 2006, 310, 101-109 8. Allen LV, Wang B., Process for making a particulate support matrix for making a rapidly dissolving dosage form. US patent 2001, 6:199-207 9. Chang RK, Gue X, Burnside BA, Couch RA, Fast-dissolving tablets. Pharm. Tecnol. N. Am. 2000, 24: 52-58 10. Mishra DN, Bindal M, Singh SK, Vijaya-Kumar SG, Spray dried excipient bases: a novel technique for the formulation of orally disintegrating tablets. Chem. Pharm. Bull. 2006, 54:99-102 11. Parrott EL. Milling, in the Theory and practice of industrial pharmacy, Leon L et al (Ed.). 1986. Lea and Febiger publisher, PA, USA, p 21-46. 12. Banker GS , Anderson NR, Tablets, ibid, p 293-345. EVALUATION OF SPRAY AND FREEZE DRIED EXCIPIENT BASES 13. Saleh I, Alangary A, Mahrous G, Utilization of honey as a tablet binder. Saudi Pharmaceutical Journal 2001, 9: 26-33 14. Phadke DS, Anderson NR, Effect of crosspovidone on the wet granulation aspects of acetaminophen. Drug Dev. Ind. Pharm. 1990, 16: 983-994 15. Malamatris S. Karidas K, Goidas P, Effect of particle size and adsorbed moisture on the compression behavior of some hydroxypropyl methylcellulose (HPMC) polymers. Int J. Pharm 1994, 103:205-215 16. Alanazi FK , El-Badry M, Alsarra IA, Spray-dried HPMC microparticles of indomethacin: impact of drug-polymer ratio and viscosity of the polymeric solution on dissolution, Saudi Pharmaceutical Journal 2006, 14: 100-107 17. Marshall K, Compression and consolidation of powder solids, in the Theory and practice of industrial pharmacy, Leon L et al (Ed.). 1986. Lea and Febiger publisher, PA, USA, p 66-99. 18. Bi Y, Sunada H, Yonezawa Y, Danjo K, Otsuka A, Lida K, Preparation and evaluation of a compressed tablet rapidly disintegrating in the oral cavity, Chem. Pharm. Bull. 1996, 44:2121-2127. Saudi Pharmaceutical Journal, Vol. 15, No. 2, April 2007 119 19. The United States Pharmacopoeia the National Formulary (USA-NF). US Pharmacopoeial Convention Inc, Rockville, MD,USA,1995,1013 20. Alanazi FK, Li H, Halpern DS, Oie S, Lu DR. Synthesis, preformulation and liposomal formulation of cholesteryl carborane esters with various fatty chains. Int J Pharm. 2003 ,14:189-97 21. Elversson J, Millqvist-Fureby A, Particle size and density in spray drying-effects of carbohydrate properties. J. Pharm. Sci 2005, 94: 2049-2060 22. Yang S, Fu Y, Jeong SH, Prak K, Application of poly(acrylic acid) superporous hydrogel microparticles as a superdisintegrant in fast-disintegrating tablets, J. Pharm. Pharmacol. 2004, 56:429-436 23. Fukami J, Ozawa A, Yoshihashi Y, Yonemochi E, Terada K, Development of fast disintegration compressed tablets using amino acid as disintegration accelerator: evaluation of wetting and disintegration of tablet on the basis of surface energy. Chem. Pharm. Bull. 2005, 53, 1536-1539.