Review of Anesthesia Team Response: Rescue Effort from the
advertisement

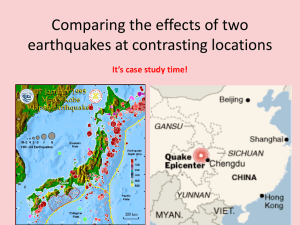
1 Review of Anesthesia Team Response: Rescue Effort from the Largest Hospital near Wenchuan Earthquake Epicenter Authors: Tao Zhu, M.D,1 Rong-Mei Li,2 Wen-Xia Huang,3 Zhen-Hai Yao, PH.D, M.D, 4 Jin Liu, M.D.5 1. Tao Zhu, Professor, Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, China 2. Rong-Mei Li, Administration Assistant, Hospital , West China Hospital, Sichuan University, Chengdu, Sichuan 610041, China 3. Wen-Xia Huang, Chief Nurse of Operating Room, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, China 4. Zhen-Hai Yao, Professor, Department of Anesthesia and Pain Management, Toronto General Hospital, 3 Eaton North 200 Elizabeth Street, Toronto, ON, M5G 2C4, Canada 5. Professor and Chairman of Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, China Corresponding Author Jin Liu, MD Professor and Chairman Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, Sichuan 610041, China, Tel: +86-28-85422520 Fax: +86-28-85423591 E-mail: xwtao_zhu@yahoo.com Short title: Anesthesia team in Wenchuan earthquake 2 Background: On May 12, 2008, an earthquake with a magnitude of 8.0 on the Richter scale occurred in southwest China’s Sichuan Province. We examined the emergency management strategies used by the anesthesia team of West China Hospital. The experience of our anesthesia team may have implications for operating room emergency management in responding to any major disaster. Methods: We reviewed the activities of the anesthesia team of our hospital between May 12 and June 11, 2008 after the Wenchuan earthquake. The analysis was based on the data provided by the hospital’s Department of Information. Results: Within 3 hours of the earthquake, a rescue team comprising 5 anesthesiologists and 5 nurses set out for the disaster area. As of July 11, 1,265 operations for earthquake injuries had been performed, in operating rooms (ORs). Most surgeries during the initial peak of surgery (May 14) were for amputations (43%). Most patients in the second peak (May 23) received second-stage procedures such as open reduction and internal fixations (61%). During this rescue, 61 (7.0%) surgeries for suspected gas gangrene were performed. Five regional surgical teams helped in our hospital for 12 days and participated in 585 procedures. Conclusions: The Wenchuan earthquake was the worst disaster in China in the past century. Quick response and OR efficiency are the keys for delivering quality medical service to a large number of earthquake trauma victims during such a short period of time. Emergency management of the OR can be accomplished effectively and safely with the use of available resources and personnel. 3 On May 12, 2008, an earthquake measuring 8.0 on the Richter scale struck southwest China’s Sichuan Province. The epicenter was in Wenchuan County. The death toll as of September 22, 2008 was 68,712 with 374,643 injuries.* West China Hospital, the largest hospital near the epicenter, has a capacity of 4,300 beds with 62 operating rooms (ORs). There are 55 attending doctors and over 150 residents in the Department of Anesthesiology. For the year of 2007, over 50,000 procedures were performed in ORs and 20,000 general anesthetics were delivered outside the OR. West China Hospital played a crucial role in providing emergency disaster relief between May 12 and June 11, 2008. Over the course of 30 (sleepless!) days, West China Hospital received 2,695 injured patients, of which 1,825 were hospitalized, and performed 1,265 operations. In this article, we describe how our anesthesia team functioned in response to the sudden influx of a large number of trauma victims. Initial Assessment When the earthquake struck there were 55 ongoing operations in our ORs: 45 under general anesthesia and 10 under local anesthesia. During both the initial earthquake and the many strong aftershocks some anesthesia machines and monitors fell to the floor. The first few minutes were chaotic. In this situation, patient safety was paramount in our minds. Immediately, patients in the holding area and postanesthesia care unit were relocated to safer areas. * http://en.wikipedia.org/wiki/2008_Sichuan_earthquake, last accessed October 5, 2009 4 Thirty-seven of the ongoing operations were quickly ended. We decided to continue the remaining 18 operations because there was not a safe way to quickly end the surgery. On the day of the earthquake, we managed to complete 133 elective surgeries by 5:05 pm. Although we applaud our dedicated staff (nursing, anesthesia, surgery, and support personnel), we point out that continuing work in the presence of powerful aftershocks represents a personal risk to staff and patients. In general, all elective cases not already underway should be cancelled after such a disaster. West China Hospital Rescue Team Simultaneously, we organized a rescue team in our hospital. Within 3 hours of the initial quake a rescue team comprising 5 anesthesiologists (1 attending anesthesiologist and 4 residents) and 5 nurses set out for the disaster area. Arriving at the scene, we found local hospitals demolished and thousands of victims crushed to death. Many more were trapped inside collapsed buildings desperately awaiting rescue. The rescue efforts were complicated by numerous aftershocks and bad weather. We brought bandages, simple external fixators, lighting, warming equipment, local anesthetics, analgesics, sedatives, and numerous appliances for debridement, amputation, and neurosurgery to the disaster area. The medical rescue team of our hospital treated 850 injuries, including 410 fractures in the field. On-site rescue efforts were reviewed after the event. Anesthesiologists played a critical role during the first two weeks after the quake. Anesthesiologists in the first wave of rescue teams realized that they had not brought enough emergency equipment for endotracheal intubation and 5 first-aid. After two weeks, when most injuries had been transferred to and treated in nearby undamaged hospitals, the primary task in the disaster area was to focus on primary health care. Preparation for Victims Arriving From the Disaster Area. No anesthesia or nursing personnel at the West China Hospital were injured. All members of the anesthesia team (anesthesiologists and nurses) were urged to (1) remain in Chengdu, (2) make themselves reachable via pager, home phone, or cell phone, (3) arrive in the ORs within 30 minutes of being paged. We divided our members into 5 groups. Each group consisted of 6-7 attending physicians and 18-20 residents working in 12-hour shifts. Nurses were divided into 3 groups of 25, working in 8-hour shifts. Two senior professors (1 surgery and 1 anesthesia) were responsible for triage during the first 24 hours. Operating Rooms Sixty two ORs in our hospital were located on 5 different floors. This distribution of facilitates allowed for isolation and quarantine of patients with potential infections. After the earthquake we selectively isolated each floor for sterilization or for patients with potentially serious infections by equipping each floor with independent entrances and exits. In this way, we maximized the use of all 62 ORs. During the initial 3 days (May 12 to May 14) of rescue, 11 ORs performed 36 procedures each day. To accommodate all victims arriving at our hospital during this emergency, the daily need for ORs varied between 11 and 20. At all times, one or two ORs with separate transport entrances and exits and independent laminar flow and air purifying systems were set up for emergency surgery on infected patients. In our 6 hospital, a maximum of 5 ORs can be available for such surgery. Therefore, this design and distribution of ORs reduced and prevented the cross infection of gas gangrene and drug-resistant bacteria between victims. Rescue of Earthquake Trauma The Chinese government’s rescue response was quick, effective and well organized. Earthquake victims were initially transferred out of the epicenter via helicopters. After 2 days of struggle, the Chinese army restored earthquake-damaged roads to the epicenter, which resulted in the effective transportation of a large number of trauma victims and the initial peak of hospital admissions. Our hospital and Chengdu city’s emergency medical center created a triage center at the army base airport. Victims from the Wenchuan epicenter were quickly disseminated to various hospitals. Our hospital received additional victims from many other quake-shattered areas including Shifang, Deyang, Du Jiangyan and Mianyan. The first victim of the Wenchuan earthquake arrived at our hospital at 15:40 on May 12. Over the following 30 days, 2,695 victims from the disaster area were treated in our hospital (1,825 inpatient; 1,265 procedures). Hospital admissions peaked 2 days after the earthquake on May 14th at 220 cases. Admission diagnoses were fractures (55%), craniocerebral injuries (10.0%), and thoracoabdominal injuries (7.5%) (Table 1). There were 875 procedures performed in our ORs. The most common operation was amputation (Table 2). Admissions and surgery associated with the earthquake between May 12 and June 11 are presented in Figure 1. The second peak of hospitalization occurred on May 20, 8 days after the earthquake (200 cases). Since our hospital is the largest medical center in Western China, from this day a significant 7 number of seriously injured victims were sent to our hospital directly from the airport after receiving urgent treatment in the disaster area. In addition, many critically injured patients were further triaged to us from nearby emergency facilities in Deyang and Du Jiangyan and from other hospitals in Chengdu. The majority of these victims suffered from complicated orthopedic injuries and required second stage open reduction and internal fixation procedures (61%) (Table 2). Management of Gas Gangrene To prevent cross infection of gas gangrene and drug-resistant bacteria among the injured, a standard protocol (wound examination flow chart) was created and strictly enforced (Figure 2). Prior to entering the emergency department, all patients were changed into isolation gowns. Secretion smears, aerobic and anaerobic cultures, as well as tests for drug sensitivity, were performed on all admissions with open wounds. Results of these tests dictated where patients would be sent (isolation ward or infected OR for surgical procedures). Two days after the earthquake, patients with suspected gas gangrene and drug-resistant bacteria infections increased markedly. Up to June 11, 67 cases of suspected gas gangrene among the earthquake victims were identified, 32 (47.8%) of whom were strongly suspected of having gas gangrene infection. The isolated and designated OR was set up and a specialized surgical team prepared to take care of these patients. During this rescue, 61(7.0%) such procedures were performed in our ORs. Effective use of multiple surgical teams from other parts of China In response to a disaster of such magnitude, Chinese and international volunteers poured into our hospital to provide assistance. To avoid chaos and effectively use this volunteer resource, the 8 Chinese central government selected and organized 5 regional surgical teams (25 different hospitals from Beijing, Tianjin, Jilin, Harbin and Hong Kong), which included 50 orthopedic surgeons, 17 anesthesiologists, and 35 OR nurses. The first regional team arrived at our hospital on May 15. Huge numbers of people from various backgrounds, different styles of practice, and varying familiarity with different varieties of equipment posed a difficult challenge for effective cooperation under such stressful circumstances. There is no doubt that these 5 regional surgical teams made a prompt and huge contribution to relief task forces in our ORs. Our staff members were effective in organizing and coordinating these enthusiastic colleagues to maximize the effectiveness of the operation. To cope with the inevitable chaos during the first few days of rescue, we developed a plan for establishing an emergency command, execution, and coordination of systems in an effort to maximize patient safety and provide an orderly rescue. One staff anesthesiologist from each rescue team was responsible for one OR. One nurse from the rescue team was responsible for scrubbing or circulating to assist the in-charge staff nurse. One staff anesthesiologist and one in-charge nurse from our hospital served as the principal coordinators and commanders-in-chief of the system in the OR. Patient safety was paramount in this chaotic environment. A daily procedure list including names of patients and surgeons was posted at each OR’s entrance. We enforced the use of the mandatory time-out by surgeons, anesthesiologists, and nurses to ensure that the planned surgical procedures were performed on the correct patients by qualified surgeons. Regional help teams 9 stayed in our hospital for 12 days and participated in 585 procedures, of which 188 (32.1%) were completed by them independently. Procedures of Earthquake Related Patients and Non-earthquake Related Patients Western China Hospital is the largest and most advanced diagnostic and treatment center in China and a major part of the regional health care network that covers nearly half of all China. Since the Wenchuan earthquake struck on May 12, our outpatient division has remained continuously open and continues to care for its routine patients, some of whom were waiting for admission and elective surgery. However, all elective surgery was put on hold, which produced a backlog of patients over time. On May 12 the day of the earthquake, 57 of 190 elective operations were cancelled. The next day on May 13, 187 scheduled procedures were cancelled to accommodate the patients from the earthquake. Most of these patients were from outside Chengdu, but chose to wait in the hospital. Consequently, the list of elective, non-earthquake related cases was growing and becoming an urgent problem. Although rescue was the number one priority, the whole anesthesia team and hospital staff worked extremely hard to accommodate as many patients as possible. We maximized the use of all 62 ORs in the 30 days after the initial strike of the Wenchuan earthquake. A total of 3,471 cases were treated in our 62 ORs, 2,596 of these (74.8%) were elective procedures not related to the earthquake. Compared to the elective procedures performed in May 2007 (3,377), this is a 2.8% increase. 10 Conclusion The Wenchuan earthquake was the worst natural disaster in China in the past century. This was the first time that our hospital played the key role in the rescue effort after such a massive natural disaster. The prompt and effective response of the anesthesia team at West China Hospital contributed to the saving of countless lives and can serve to guide other hospitals when dealing with large scale natural disasters. 11 Figure legends. Figure 1 Chart for Admission and Performed Procedures (May12 to June 11) Figure 2: Triage Flow Chart 12 Table 1: Admission diagnoses after the Wenchuan earthquake Admission diagnosis Fracture Craniocerebral injury Thoracoabdominal injury Compartment syndrome Crush syndrome Ocular injury Others Number of patients 1018 182 140 20 17 6 442 Percent 55.8% 10.0% 7.7% 1.1% 0.9% 0.3% 24.2% 13 Table 2: Surgical procedures during the two patient peaks after the Wenchuan earthquake Surgical Procedure Amputation Debridement and suturing Open reductin and internal fixation (ORIF) Other Initial Peak Second Peak (%) (%) 43% 4% 22% 21% 15% 20% 61% 15% 14 Figure 1: 15 Figure 2: