Case Study 5: Patient with proteinuria
advertisement

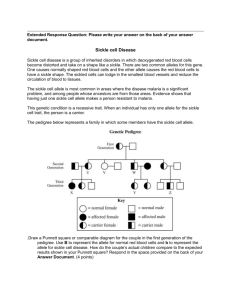
Case Study 5: Patient with proteinuria Other studies 1. 2. 3. 4. 5. 6. Sickle cell patient complains about shortness of breath Patient considering discontinuing Desferol therapy Pain Manangement Sß+ Thalassemia patient with acute infarct Patient with proteinuria Pregnancy and sickle cell care Adult Sickle Cell Care Provider: CASE STUDY #5 (Total repondents=9) Results of Adult Case No.5 28-year-old man with HbSS, baseline Hemoglobin 8.0 gm/dl, Hep C negative, infrequent pain events, working father with wife and 3 children. No history of acute multi-organ failure or chest syndrome. Urinalysis demonstrates 1+-2+ proteinuria blood pressure values 115-125 systolic, 80-85 diastolic creatinine ranges from 1.2-1.5 mg/dl. Other: SCD with tubule dysfunction is common and defects in potassium excretion (hyperalemia) are not clinically apparent until the renal failure is acute. Increased creatinine secretion can result in a pseudo-low level serum creatinine and assumption that GFR is not as impaired as what really is. Renal failure must be evaluated immediately. Actually, what I do is a spot urine for protein and creatinine and if the Pr:cr> 0.3, I would start an ACE inh. I use an ARB if cough or angiodema is a problem with the ACEI. I would also exclude HIVm and check an ANCA, C3, C4 and Hep C as general screen before referring to nephrologist. I would order 24 hour urine for creatinine clearance and protein quantitation along with careful follow-up. If the results show hyper filtration with increased clearance - with or without protein, I would start him on Cozaar (Losartan) 25mg and recheck the 24 hour collection in 6 months. If no significant decrease in his clearance, Cozaar would be titrated upward to 50mg (or higher if needed and as BP would allow) with another 6 month recheck. Once the hyper filtration has decreased, would follow up with annual collections and continue Cozaar. **Ace Inhibitors suggested: Losartan (25-100mg), Vasotec (2.5mg), Enalapril , Lisinopril (5mg), (Benazepril, Monopril, Cozaar - 10mg titrate upward as needed and as BP allows) Follow Periodically: All respondents would follow-up in 3-6 months. Initiate Other Treatment: (Below comments taken from surveys returned) A 24-hour creatinine is not particularly helpful as patients' hyperexcrete creatinine. It is likely that renal function will continue to worsen and thus patient will require careful follow-up. The few studies done on the use of ACE inhibitors do show benefit but follow-up is short. Follow patient at least every three months in heme clinic and then renal follow-up as suggested by nephrology. Although there is no data, the inevitability of this patient ending up on dialysis would make me consider hydroxyurea therapy and I would discuss this with the patient. Avoid NSAIDS (causes decline of GFR). Low protein diet, no beta-blockers, or potassium-sparing diuretics as they can potentiate hyperkalemia. Proteinuria can be the first clinical sign of glomerlular injury/nephritic syndrome. I would start momopril 10mg and titrate dose as tolerated to BP. I will evaluate BP and basic metabolic profile in one month and consider titrating dose based on BP. I repeat a spot urine Pr:Cr and U/A after 3 months to assess protein wasting. SUMMARY/DISCUSSION: As you can see by the responses above, all practitioners who responded to this case would further investigate this patient's renal status. While the specific approaches vary somewhat, and are worth reviewing to see what might fit in your practice, general principles are apparent: Recognition and Evaluation of Renal Disease: All providers recognized that significant renal disease may be present in this patient and all felt additional work-up and/or careful follow-up was indicated. Proteinuria, hypertension, and increasingly severe anemia have long been recognized to predict end-stage renal disease in patients with sickle cell disease (1,2), may have onset in late childhood, but is more common in adults. Almost all practitioners would do a 24 hour urine for protein, though at least one provider would do a spot urine for protein and creatinine, looking for a ratio >0.3. There was a small study using the albumin/creatinine ratio in sickle cell disease patients which found this to be a sensitive (100%), but somewhat non-specific (87.2%) test (3). They suggested patients with ratios >0.45 should have 12-hour urine collections to confirm increased albumin excretion. However, unlike the patient in this case, all the patients in the study had normal serum creatinine values, so likely had better renal function than our patient. Additionally, it is sometimes much easier to screen with a spot urine than obtain an accurate 24-hour collection. There was recognition that there is increased creatinine secretion in patients with sickle cell disease, making a serum creatinine and creatinine clearance a poor indicator of GFR. At least one provider uses the creatinine clearance to look for increased values as an indicator of hyperfiltration, thought to be an early indication of sickle nephropathy, as is seen in diabetic patients. Some providers are able to obtain an inulin clearance. This method will more accurately measure GFR (4,5), but it may not be readily available in all practices. In some practices, a nephrologist is involved, either to provide consultation or a renal biopsy. Evaluation for nonsickle cell causes of renal dysfunction is important, as other diagnoses might be present (e.g. glomerulopathies, autoimmune disorders, hepatitis C) which might require other therapies (e.g. steroids). Initiation of Therapy with ACE/ARB: The majority of practitioners would begin therapy once either proteinuria and/or hyperfiltration was recognized. The therapy of choice for most is an angiotensin-converting enzyme inhibitor (ACE). Small studies have been done in sickle cell disease patients using enalapril (6, 7) and captopril (8) to reduce proteinuria and/or microalbuminuria. Some practitioners use lisinopril (prinivil, zestril), benazepril (lotensin) or fosinopril (monopril). Though these newer ACE inhibitors have not been specifically studied in sickle cell disease, their anti-proteinuric effects have been demonstrated in other disease states. Some providers would initiate therapy with losartan, an angiotensin II receptor blocker (ARB). Others would use this as an alternative in patients who do not tolerate an ACE inhibitor (due to angioedema, cough or other reactions). As with newer ACE inhibitors, there are no reports of the effect of ARB on proteinuria or hyperfiltration in sickle cell disease, but data suggests improvements in these parameters in other diseases. Continued Monitoring and Therapy: After initiation of therapy, most practitioners have a standard approach to monitor response to therapy, titrating drug dosing as tolerated. Given the potential for progression to renal failure despite therapy, at least one provider would discuss the use of hydroxyurea in an effort to curb disease progression. There are no data available yet on the potential effect of hydroxyurea on renal function. There was also recognition of the need avoid NSAIDs or at least use them with great care, given the deleterious effect on GFR, which has been demonstrated in sickle cell disease patients (4,9,10). Early Detection: The presence of microalbuminuria is thought to be an early indication of renal dysfunction (11), and this microalbuminuria was reduced by captopril in a small study of normotensive adults with sickle cell disease (8). These observations have led to a recommendation in the most recent NIH consensus document that routine screening for microalbuminuria show be performed for adults with sickle cell disease. REFERENCES 1. Powars DR, Eliott-Mills D, Chan L, Niland J, Hiti A, Opas L, Johnson C. Chronic renal failure in sickle cell disease: Risk factors, clinical course, and mortality. Annal of Int Med 115:8 614-620, 1991. 2. Sklar AH, Campbell H, Carunana RJ, Lightfoot BO, Gaier JG, Milner P. A population study of renal function in sickle cell anemia. J Artif Organs 13:4, 231-236, 1990. 3. Lima CS, Bottini PV, Garlipp CR, Samtos AO, Costa FF, Saad ST. Accuracy of the urinary albumin to creatinine ratio as a predict of albuminuria in adults with sickle cell disease. J Clin Pathol Dec;55(12):973-5, 2002. 4. Allon M, Lawson L, Eckman JR, Delaney V, Bourke E. Effects of nonsteriodal antinflammatroy drugs on renal function in sickle cell anemia. Kidney Int.34:500-506, 1988. 5. Guasch A, Millicent VUA, Mitch WE. Early detection and the course of glomerular injury in patients with sickle cell anemia. Kidney International 49:786-791, 1996. 6. Falk RJ, Scheinman J, Phillips G, Orringer E, Johnson A, Jennetter JC. Prevalence and pathologic features of sickle cell nephropathy and response to inhibition of angiotensin- converting enzyme. N Engl J Med Apr;326(14):910-5, 1992. 7. Aoki RY, Saad STO. Enalapril reduces the albuminuria of patients with sickle cell disease. Am J of Med 98: 432-435, 1995. 8. Foucan L, Bourhis V, Bangou J, Merault L, Etinne-Julan M, Salmi RL. A randomized trial of captopril for microalbuminuria in normotensive adults with sickle cell anemia. Am J Med Apr;(4):339-42, 1998. 9. Allon M. Renal abnormalities in sickle cell disease. Arch Intern Med 150:501-504, 1990. 10. Scheinman JI. Sickle Cell Disease and the kidney. Sem in Nephrology 23;1:66-76, 2003. 11. Aoki RY, Saad ST. Microalbuminuria in sickle cell disease. Braz J Med Biol Res. 23:1103-1106, 1990. Back to Top For additional information please contact: Colorado Sickle Cell Center If you are experiencing problems using this website contact Webmaster