5 - Acusis
advertisement

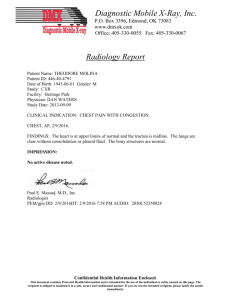
<BODY> PRESENT ILLNESS: This 73-year-old patient of mine states that she has had chills and felt very weak yesterday. She called her son, who brought her into the emergency room. She was seen in the ER and workup showed that she had a chest x-ray which was negative; CT scan, questionable infiltrate at the right base; however, the __________ is abnormal. She also had some tenderness in the right upper quadrant/right mid quadrant, suggesting that she may have an ascending cholangitis. She is being admitted at this time, started on antibiotic therapy. Dr. Walsh has seen the patient and we may be getting a GI consultation, infectious disease consultation. PAST MEDICAL HISTORY: She has a history of hypertension with hypertensive cardiovascular disease, history of parotid tumor for which she had a resection and, in addition to that, chemotherapy at Valley Medical Center. She also had a meningioma; most of it was removed, expect some was left in. This was many, many years ago by Dr. Emeka Nchekwube, a neurosurgeon. Patient has a very forgetful memory, especially for any recent events. She denies any chest pain. No shortness of breath. No cough, cold, or urinary symptoms. Past medical history and social history has been extensively documented here and Regional Medical Center. ALLERGIES: PENICILLIN. MEDICATIONS: 1. Micardis HCT 80-12.5 once a day. 2. Propranolol 100 mg daily. 3. Salicylate 750 mg 2 times a day. 4. Vicodin 1 q.6 h. p.r.n. 5. Calcium with vitamin D twice a day. 6. Propoxyphene-N 100-650 mg 1 every 4 hours p.r.n. 7. Fergon 325 mg daily. 8. Clonazepam 0.5 mg daily. REVIEW OF SYSTEMS: CONSTITUTIONAL: She denies any headache, is occasionally dizzy. EYES, EARS, NOSE, AND THROAT: She is moderately hard of hearing. RS: No cough, no shortness of breath at rest, hemoptysis. CVS: No history of angina, myocardial infarction, ectopic heartbeat. GI: See present illness. GU: No dysuria. PSYCHIATRIC: History of forgetfulness, as discussed above. CNS: No history of seizure, loss of consciousness. PHYSICAL EXAMINATION: GENERAL: This is a female who is lying in bed who looks in discomfort but not severely ill. VITAL SIGNS: Blood pressure 120/58, respirations 20, heart rate 70, temperature 98. HEENT: Normocephalic, no trauma. Scalp is normal. Face shows good healing from dissection of left parotid tumor. Pupils are equal. Extraocular movements are normal. She has some weakness on the left side after resection of her meningioma. She is not anemic or icteric. Mouth negative. NECK: Supple. Carotids are felt without bruits. There is no thyroid enlargement. CHEST WALL: With no deformity. BREASTS: No masses. LUNGS: On auscultation, clear. HEART: PMI outside the midclavicular line. There is no ventricular heave, rub, or gallop. ABDOMEN: Soft, distended. There is a questionable mild tenderness in the right mid quadrant. No spleen or liver enlargement, no ascites. Inguinal areas show no lymphadenopathy, no hernia. GENITALIA: External genitalia normal. EXTREMITIES: Reveal no clubbing, no cyanosis, no edema. NEUROLOGIC: Patient is conscious, able to move her extremities. No focal deficit noted. ASSESSMENT: 1. Ascending cholangitis, rule out choledocholithiasis. 2. Status post cholecystectomy. 3. Hypertension and hypertensive cardiovascular disease. 4. Degenerative arthritis. 5. Vascular dementia. 6. Status post resection of meningioma many years ago. 7. Status post resection of a parotid carcinoma with radiation therapy and chemotherapy. 8. Allergic rhinitis. 9. Possibly __________ disease of the lung. </BODY> <BODY> This 47-year-old patient is admitted from the emergency room with severe anemia and epistaxis. Patient is an unfortunate patient who suffers from recurrent epistaxis from his posterior nares, also some GI bleeding from a significant angiodysplasia of his GI tract. Has had multiple admissions to this hospital. His hemoglobin outpatient was 5.8. The dialysis nurse called me. I advised him to come to the ER. When seen in the emergency room, his chest x-ray showed potential pulmonary hypertension, otherwise, no acute cardiomegaly. He has a history of occult sarcoidosis in the past. This is well documented. His EKG shows a normal sinus rhythm with an old possible inferior myocardial infarction. Initial hemoglobin confirmed that it was low, 5.4, and we will admit him, give him 3 units of packed cells. He probably will need more blood, so we may have to dialyze him again tomorrow. He denies any chest pain or abdominal pain. No gross blood per stool, but stool is guaiac positive. PAST MEDICAL HISTORY: ALLERGIES: __________. Unknown. MEDICATIONS: 1. Procardia XL 60 mg twice a day. 2. Diovan 60 mg b.i.d. 3. 4. 5. 6. 7. 8. Lisinopril 20 mg b.i.d. Lopressor 50 mg q.8 h. Minoxidil 5 mg b.i.d. __________ 600 mg at bedtime. Prednisone 10 mg daily. Fluoride 1 a day. REVIEW OF SYSTEMS: He denies any headache. Has been dizzy, though. EYES/EARS/NOSE/THROAT: Hard of hearing. RS: Cough, shortness of breath with exertion. No hemoptysis. CVS: No history of angina, myocardial infarction. GI: Appetite has been poor, according to him, for a couple days. Bowel movement: He has noticed some black stool. GU: No dysuria. PSYCHIATRIC: Negative. CNS: No history of seizure. PHYSICAL EXAMINATION: GENERAL: This is an acute and chronically ill-looking man. VITAL SIGNS: His blood pressure is 112/70, respirations 16, heart rate 102, temperature 98. HEENT: Normocephalic, atraumatic. Scalp is normal. Face shows no asymmetry. Pupils are equal without significant AV nicking. Fundi __________, not icteric. His mouth and ears are negative. NECK: Supple. Carotids are felt without bruits. No thyroid enlargement. CHEST WALL: Shows slightly increased AP diameter. LUNGS: To auscultation, decreased air entry bilaterally with bilateral rhonchi. HEART: PMI outside the midclavicular line. No heave, no rub, no gallop. ABDOMEN: Soft. No tenderness. No spleen or liver enlargement. No ascites. Inguinal area shows no lymphadenopathy, no hernia. Femoral pulses are felt. GENITALIA: Normal. EXTREMITIES: No clubbing, no cyanosis, and no edema. NEUROLOGIC: Done by ER physician. Patient is conscious, able to move his extremities. No focal deficit noted. ASSESSMENT: 1. Severe symptomatic anemia. Recurrent epistaxis from the posterior nares. 2. Recurrent gastrointestinal (GI) bleeding secondary to angiodysplasia of the GI tract. 3. Endstage renal disease. 4. Hypertension. 5. Hypertensive cardiovascular disease. 6. Sarcoidosis. 7. Cirrhosis of the liver. </BODY> <BODY> This patient was brought in by the family with shortness of breath, chest discomfort, and pain in the left hip and left thigh. Patient, who has been on chronic maintenance hemodialysis at the satellite dialysis unit, was supposed to be going for dialysis today, but she got progressively short of breath with pain in the leg. She was brought to the emergency room and was seen by the ER physician. At this time, a chest x-ray revealed a moderate amount of congestive heart failure. Chest pain. EKG showed no evidence of an acute myocardial injury. Enzymes were unremarkable. It was felt that she may have a tightness from fluid overload. Her left hip and left leg pain will be evaluated; an x-ray has been ordered. She denies any mechanical fall. The patient has severe end-stage renal disease with diabetes, hypertension, hypertensive cardiovascular disease, coronary artery disease, and obesity. She is using a PermCath in the right side for chronic maintenance hemodialysis. PAST MEDICAL HISTORY, SOCIAL HISTORY, FAMILY HISTORY: previous chart. ALLERGIES: On MORPHINE SULFATE. MEDICATIONS: 1. Vicodin 1 tab at bedtime. 2. Diovan 160 mg twice a day. 3. AcipHex 20 mg daily. 4. Norvasc 10 mg daily. 5. Coreg 80 mg daily. 6. Folic acid 1 mg b.i.d. 7. Amaryl 2 mg daily. 8. Lipitor 20 mg at bedtime. 9. Sinemet 25-100 one b.i.d. 10. Celebrex 200 mg daily. 11. Renagel 800 mg t.i.d. with meals. REVIEW OF SYSTEMS: GENERAL: No headache, no dizziness. EYES, EAR, NOSE AND THROAT: Hard of hearing. RS/CVS: See present history. GI: Appetite has been poor, according to the family. Bowel movement constipation. No diarrhea. No hematemesis or melena. GU: No dysuria. PSYCHIATRIC: Negative. CNS: No seizures. PHYSICAL EXAMINATION: GENERAL: Chronically ill-looking female lying in bed; is moaning and groaning at this time. VITAL SIGNS: Blood pressure 159/52, respirations 21, heart rate 58, temperature 99. HEENT: Normocephalic, atraumatic. Scalp is normal. Face shows no asymmetry. Her pupils are equal. There is significant AV nicking in her fundi. She is moderately anemic, not icteric. Her mouth and ears are negative. NECK: Supple. Carotids are felt without bruits. There is no thyroid enlargement. CHEST: Chest wall shows no deformity. She has a PermCath on the right side at subclavian area. Lungs with bilateral rales about two-thirds of the way. HEART: PMI outside the midclavicular line. No thrills, heaves, rubs, or gallop present. ABDOMEN: Large panniculus. Liver palpable below the costal margin. There are no abdominal masses. No bruits. Inguinal area shows no lymphadenopathy, no hernia. Femoral pulses are felt. Pulses are present in all 4 extremities. EXTREMITIES: No clubbing, no cyanosis, no edema. There is no evidence of obvious deformity of the left leg. When moving her left leg, it is painful and also tenderness in the thigh. There is no evidence of any swelling. Homans sign is negative. She has no calf tenderness. NEUROLOGIC: The patient is conscious, is fairly alert, according to the family, and moves her extremities. No deficit noted. ASSESSMENT: 1. Congestive heart failure, significant fluid overload, rule out myocardial infarction. 2. Chest pain. 3. Left hip and leg pain, full evaluation, x-rays will be done. 4. Hypertension. 5. Hypertensive cardiovascular disease. 6. Type 2 diabetes mellitus. 7. Diabetic peripheral neuropathy. 8. Diabetic peripheral vascular disease. 9. Nephropathy with endstage renal disease. 10. Anemia of chronic disease. </BODY> <BODY> This patient was admitted with right upper quadrant pain and fever. ADMITTING DIAGNOSES: 1. Ascending cholangitis. 2. Choledocholithiasis, status post cholecystectomy. 3. Hypertension with hypertensive cardiovascular disease. 4. Degenerative arthritis. 5. Vascular dementia. 6. Status post resection of meningioma many years ago. 7. Status post resection of parotid carcinoma with radiation therapy and chemotherapy. 8. Allergic rhinitis. 9. Severe chronic interstitial lung disease. Patient was started on antibiotic therapy. Patient was consulted by Dr. Brian Levitt in GI consultation, and impression was that the patient go to get ERCP. Seen also in consultation by Dr. Michael Charney for antibiotic therapy and by Dr. Hugh Walsh, general surgeon. Patient initially had quite a bit of right upper quadrant pain. She was kept n.p.o. on intravenous fluids. Findings of that were a __________ small papilla. Only superficial cholangiogram obtained. Per Dr. Stone, unable to obtain deep cannulation, contrast drained quickly. No sphincter study was done. PD not cannulated or injected, according to doctor. Patient was observed and continued antibiotic therapy. Blood culture grew also E coli for which she was on Levaquin. There was no significant __________ which was sensitive, but then we switched her to Levaquin. She seemed to be better. She had pain, but her liver function tests improved and are coming back to normal. Her white count is back to normal now. She is anemic, but she has been advised to take her Fergon 240 mg daily at discharge. DISCHARGE DIAGNOSES: 1. Ascending cholangitis. 2. Possibly choledocholithiasis. 3. Small sphincter ampulla of Vater. 4. Possibly jaundice due to above. 5. Hypertension, hypertensive cardiovascular disease. 6. Degenerative arthritis. 7. Vascular dementia. 8. Status post resection of meningioma many years ago. 9. Status post infection of the left parotid tumor due to radiation therapy and chemotherapy. 10. Anemia of chronic disease. </BODY>