Patient Medical History
advertisement

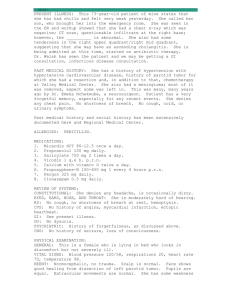
Name:__________________ Date of Visit: __________________ New Patient Form Reason for Visit: □ Abnormal Chest X-Ray □ ABPA □ Asthma □ Asbestosis □ Chest Congestion □ Chest Pain □ Chronic Cough □ COPD □ Fatigue □ Hemoptysis □ Hypoxia □ Lung Mass/Cancer (circle) (Expose to Asbestos) □ Pulmonary Hypertension □ Rhinitis □ Shortness of Breath □ Pneumonia Type _____________ □ Sleep Apnea □ Snoring □ Tuberculosis □ Smoking Cessation □ Pleurisy □ Bronchitis □ Cystic Fibrosis □ Nose Bleed □ Carcinoid □ Emphysema □ Occupational Lung Disease □ Cataplexy □ Emphysematous Bleb □ Pleural Effusion □ Hypertension □ Hyperlipidemia □ Gastroesophogeal Reflux □ Depression □ Restless Leg Syndrome □ Sarcoidosis Condition(s) Not Presented: _____________________________________________________________________________________ Is this a Follow Up After: □ Hospitalization □ Lab Test □ Diagnostic Procedure (X-Ray, CT Can, etc) Is this a Pre-Op Visit? □ Yes □ No If yes what procedure? _______________________________________ Past Medical History: □ Abnormal Chest X-Ray □ Chest Congestion □ Hypothyroidism □ ABPA □ Chest Pain □ Asthma □ Chronic Cough □ Hypertrophy of Prostate (Enlarged) □ Hypoxia □ Asbestosis □ Depression (Expose to Asbestos) □ Irritable Bowel Syndrome □ Interstial Lung Disease □ Lung Mass/Cancer □ Pneumonia Type _____________ □ Positive Skin Test for Tuberculosis □ Restless Leg Syndrome □ Rhinitis □ Anxiety □ Arthritis-Rheumatoid □ Diabetes □ Embolism-Pulmonary □ Sarcoidosis □ Seizure Disorder □ Atherosclerosis □ Bronchitis (Acute) □ Bronchiectasis □ Carcinoid (Cancer) □ Cardiomyopathy □ Cataplexy □ Emphysema □ Emphysematous Bleb □ Fatigue □ Gastroesophogeal Reflux □ Hepatitis □ Hiatal Hernia □ Multiple Sclerosis □ Nyocardial Infarction □ Nose Bleed □ Occupational LungDisease □ Obesity □ Osteoporosis □ Congestive Heart Failure □ COPD (Chronic Bronchitis) □ Cystic Fibrosis □ Hypertension □ Pulmonday Hypertension □ Shortness of Breath □ Sinusitus □ Smoking Cessation □ Snoring □ Sleep Apnea-Central □ Sleep ApneaObstructive □ Insomnia □ Hemoptysis □ Pleurisy □ Narcolepsy □ Hyperlipidemia □ Pleural Effusion □ Tuberculosis (circle) Name:__________________ Date of Visit: __________________ Allergy History: □ No Known Allergies □ No Known Drug Allergies □ Allergy History Unknown □ Have had an “Allergic Reaction”, but do not know cause? Reaction Experienced: __________________________________________________________________ Medication Allergies: □ ACE Inhibitors □ Aminoglycosides □ Barbiturates □ Cephalosporin □ Erythromycins □ Iodine (Contrast) □ Penicillin □ Other: ___________ □ Other: ___________ Food Allergies: Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ Reaction:______________ □ Acetaminophen Reaction:_____________ □ Aspirin (Salicylates) Reaction:____________ □ Benzodiazepines Reaction:____________ □ Codeine (Derivatives) Reaction:____________ □ Morphine (Derivatives) Reaction:____________ □ Anesthetics Reaction:____________ □ Zithromax Reaction:____________ □ Other: ____________ Reaction:____________ □ Other: ____________ Reaction:____________ □ Food:____________ Reaction:______________ □ Food:____________ Reaction:______________ □ Food:____________ Reaction:______________ Environmental: □ Food:____________ Reaction:______________ □ Food:____________ Reaction:______________ □ Food:____________ Reaction:______________ □Mold Reaction:______________ □Dust Reaction:______________ □ Other: ___________ Reaction:______________ □ Other: ___________ Reaction:______________ □ Pollen Reaction:______________ □ Insect Bite(_______) Reaction:______________ □ Other: ___________ Reaction:______________ □ Other: ___________ Reaction:______________ Family History: □ No known Pertinent □ Apnea □ Bleeding Disorder □ CHF □ CVA □ Diabetes □ Goiter □ Hypercholesterolemia □ Insomnia □ Myocardial Infarction □ Pulmonary Fibrosis □ Restless Leg Syndrome □ Suicide □ TIA Family History Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ □ Asthma □ Cancer: ___________ □ Coronary Heart Disease □ Depression □ Emphysema □ Heart Disease □ Hypertension □ Kidney Disease □ Narcolepsy □ Respiratory Condition □ Seizure disorder □ Thyroid problems □ Tuberculosis Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Family Member:________ Name:__________________ Date of Visit: __________________ Social History: Are you at risk for HIV? □ Yes □ No If yes, what are your risk factors? □ Unprotected Sex □ Caregiver of HIV Pos. Individual(s) □ Injection Drug User □ Transfusion Recipient □ Occupation □ Other: __________________ Are you currently employed? □ Yes □ No □ Disabled □ Disabled due to HIV □ Disabled due to non-HIV condition □ Part Time □ Retired □ Self Employed □ Unemployed not looking for work □ Full Time □ Unemployed Looking for Work □ Other Primary Occupation? ___________________________________________________________________ Marital Status: □ Single □ Married □ Divorced □ Widowed Do you Exercise: ___Yes ____ Hours Day _______ Day(s) Weekly ___No Exercise Daily Sleeping Habits: ________ Hours Nightly on Average Alcohol Use: □ Do Not Drink □ Quit Drinking (When?) Tobacco Use: □ Occasional Use □ Moderate Use □ Heavy Use (1-8 beverages x monthly) (2-10 beverages weekly) (6+ beverages daily) Date: _______________ □ Never Smoked □ Smoke ( ___ pks daily) □ Smoke (non-cigarette) Type: ______________ □ Chewing Tobacco □ Quit Smoking When did you quit? How many years previously smoked? ____ When you did smoke, how many pks daily? _______ Date: ______________ Drug Use: □ No Drug Use □ Quit Drug Use (When?) Date: _______________ Drug Used? _________ □ Intermittent Use (Social 1x 1-3 months) □ Intermittent Use (Social 1x 1-3 months) □ Occasional Use (2-3 x monthly ) □ Occasional Use (2-3 x monthly ) □ Daily Use (1-2 x Daily ) □ Daily Use (1-2 x Daily ) □ Smoke (Non-Tobacco) How often exposed? □ Smoke (2nd Hand) How often exposed? □ Chemicals (________) How often exposed? Drug Used? _________ Environmental Exposure: □ Pets / Animals How often exposed? Name:__________________ Daily: ___________ Weekly: ___________ Monthly: ___________ Date of Visit: __________________ Daily: ___________ Weekly: ___________ Monthly: ___________ Daily: ___________ Weekly: ___________ Monthly: ___________ Daily: ___________ Weekly: ___________ Monthly: ___________ Travel History: Have you traveled outside of the US recently? Where and When? Country / Date: / Country / Date: / Country / Date: / Country / Date: / Medication History: List only medications currently being taken; include over the counter drugs and vitamins/supplements. Name: Dose: (2 x daily, etc) Name: Dose: (2 x daily, etc) Past Surgical: Name of Procedure: Date Performed: Where/Who performed by: Diagnostic Studies: Have you had any test(s) (x-rays, CT scan, MRI, etc) performed in preparation for your visit today? **Female patients: When was your last Mammogram? Date:______________________ Name of Procedure/Lab: Date Performed: Where/Who performed by: Name:__________________ Date of Visit: __________________ Comments: Is there any Medical History or Comments related to your condition(s) that you would like to note? _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ Review of Symptoms: Are you experiencing or recently experienced any of the following: General: □ Appetite Loss □ Fatigue □ Fever □ Night Sweats □ Obesity □ Weight Gain □ Weight Loss □ Unable to Sleep Lying Flat □ Respiratory: □ Bloody Sputum □ Cough □ Difficulty Breathing □ Difficulty Breathing Exertion □ Sputum Production □ Wheezing □ Waking with Shortness of Skin: □ Bruising □ Itching □ Nail Color Changes □ Rash □ □ □ □ □ Breast: □ Breast Mass □ □ □ □ □ □ HENT: □ Headache □ Nasal Congestion □ Seasonal Allergies □ Sleep Apnea □ Snoring □ Hoarseness □ □ □ Cardiovascular: □ Chest Pain □ Edema □ Palpitations □ Swelling in Extremities □ □ □ Neck: □ Neck Mass □ Swollen Glands □ □ □ □ □ □ □ Gastrointestinal: □ Diarrhea □ Difficulty Swallowing □ Heartburn □ Nausea □ Vomiting □ □ Neurological □ Decreased Memory □ Seizures □ Stroke □ Weakness □ □ □ □ □ □ □ Psychiatric □ Anxiety □ Change in Sleep Pattern □ Depression □ Early Awakening □ Easily Irritated □ Hypersomnia □ Impaired Cognitive Function □ Inability to Concentrate □ Insomnia □ Panic Attacks □ Trouble Falling Asleep Endocrine □ Libido Changes □ Thyroid Problems □ □ Hematology □ Blood Clots □ Enlarged Lymph Nodes □ □ □ □ Breath or Wheezing Musculoskeletal □ Join Pain □ Muscle Pain □ Muscular Weakness □ □ □ □ □ □ □ □