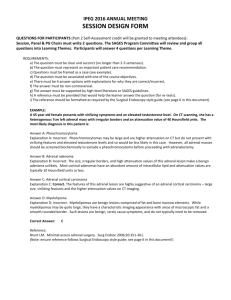
suspected ADRENAL `INCIDENTALOMA`
advertisement

Clinical Guideline SUSPECTED ADRENAL ‘INCIDENTALOMA’ SETTING Trust-wide FOR STAFF Part 1 - Medical staff, including radiologists, who identify a possible case Part 2 – Specialist medical staff within Endocrine Team PATIENTS Patients with an unexpected adrenal lesion following diagnostic imaging _____________________________________________________________________________ BACKGROUND ‘Incidentaloma’ is an internationally accepted term for a lesion incidentally discovered through diagnostic imaging, without prior clinical suspicion of tumour / disease. Published evidence (1,2) suggest the following pathology for adrenal incidentalomas; Endocrine inactive adenoma Metastases Cortisol secreting adenoma Adrenocortical carcinoma Phaeochromocytoma Conn’s Other causes 41 - 85% of cases ‘’ 15 - 19% ‘’ 5 - 10% % ‘’ 2 - 10 ‘’ 3 - 8% ‘’ 2 - 5% % ‘’ 2- 9 Part 1 REFERRAL TO ENDOCRINE TEAM Medical staff that identify a possible adrenal incidentaloma should refer the patient to the Endocrine Team for further investigation. Referral details should include Hospital Registration Number Surname Forname Date of Birth Date of diagnostic imaging Imaging report number Part 2 ENDOCRINE TEAM ONLY (overleaf) Version 1 Sept 2011 - Review Sept 2014 Author Dr Karin Bradley, Endocrinology Consultant Page 1 of 3 Part 2 ENDOCRINE TEAM ONLY The algorithm below describes the diagnostic pathway There are no long term data to be confident of the appropriate duration of imaging or hormonal surveillance but abnormal secretion has been detected during prolonged follow-up 3,4,5. The risk of endocrine abnormalities was higher in patients with a baseline lesion ≥ 3cm. This guideline is consistent with recent clinical practice guidelines1,6,7,8. ASSESSMENT OF ENDOCRINE STATUS Careful personal and family history and full examination Proceed as appropriate if underlying endocrinopathy suspected RECOMMENDED OUT-PATIENT TESTS IF NO ENDOCRINE PHENOTYPE SUSPECTED 1. 2. 3. Two 24 hour urine collection samples for catecholamines (N.B. regional laboratories may use alternative baseline screening tests) to help exclude phaeochromocytoma#. Ideally avoid interfering medication including paracetamol, many antihypertensives, catecholamine containing drugs & some antidepressants). Plasma metanephrines may be indicated, especially in the context of a genetic phaeo/paraganglioma syndrome. 1mg overnight dexamethasone suppression test to exclude subclinical Cushing's (*see below). (1mg dexamethasone at 11PM followed by serum cortisol at 9 am next morning. The morning cortisol should ideally be <50nmol/l. Values 50nmol/l138nmol/l fall into an area of clinical uncertainty and surgery may be discussed as an option especially in the presence of diabetes or hypertension. In the absence of any classic phenotype further Cushing’s investigations probably only helpful if overnight result >138nmol/l or clinical progression9. However, UFC (urinary free cortisol), low dose dexamethasone suppression test, morning ACTH or midnight salivary cortisol may be considered. Aldosterone/Renin ratio (ARR) only in hypertensive patients to exclude Conn's syndrome. Aldosterone and renin levels are affected by many anti-hypertensive agents. Ideally use doxasozin alone for 4-6 weeks pre-testing. Correct potassium to normal pre test. If ARR sufficiently elevated (refer to local laboratory range) then proceed to a confirmatory test e.g. saline infusion or fludrocortisone suppression and adrenal CT. Adrenal vein sampling should be considered unless patient <40years with clear unilateral >1cm adenoma10. BIOCHEMICALLY FUNCTIONING (Include subclinical Cushing’s in this category but remember that surgery for this indication remains controversial. BIOCHEMICALLY NON-FUNCTIONING Consider presence of diabetes, hypertension or other CV risk and patient choice when counselling) Less than 4cm in size Baseline malignancy risk ~ 2% Hounsfield units less than 10, benign appearance on CT & no personal history of malignancy 1. 2. 3. 4. 4cm or greater in size Baseline malignancy risk Size 4-6cm ~ 6% risk6, Size >6cm ~ 25% risk6 Hounsfield units more than 10 (? fat poor benign adenoma in 25 % cases) or history of malignancy11,12 Repeat CT scan 6 months after baseline scan and calculate contrast washout at 10 minutes. Consider MRI in women of reproductive age or where there is impaired renal function or known contrast sensitivity No repeat imaging required2. Hormonal surveillance at baseline and at 2 years. Hormonal surveillance at 4 years if baseline size ≥ 3 cm3. Up to 20% will become hormonally active2. Consider surgery if mass becomes hormonally active. When discharging to GP care recommend referral for re-evaluation if symptoms dictate as rarely functional activity has been described after prolonged follow-up. Version 1 Sept 2011 - Review Sept 2014 Consider surgery. Refer to neuroendocrine tumour (NET) MDT. Remember the need for peri- and post-operative steroids if evidence of endogenous hypercortisolaemia. Postoperatively ensure resolution of any abnormal biochemistry. If adrenal carcinoma suspected measure testosterone, DHEA, 17OHP & androstenedione and CT chest. FDG-PET can be a useful tool for identifying adrenal malignancy. Contrast washout greater than 60% in 10 minutes3 – likely fat poor benign adenoma Contrast washout less than 60% at 10 minutes3 or an increase in size >1cm. Author Dr Karin Bradley, Endocrinology Consultant Page 2 of 3 #It is worth noting that a phaeochromocytoma is extremely unlikely if Hounsfield units are less than 10. A phaeochromocytoma diagnosis becomes more likely if the Hounsfield units are more than 10 and the lesion is more than 3cm in size. *Various medications may interfere with dexamethasone metabolism and this should be taken into account when interpreting the overnight dexamethasone suppression test. These include sertraline, fluoxetine, paroxetine, trazodone, citalopram, bupropion, venlafaxine, atorvastatin, simvastatin, verapamil, diltiazem, amlodipine, nifedipine, felodipine, irbesartan, losartan, olanzapine, quetiapine, proton pump inhibitors, propranolol, pioglitazone, clonazepam and topiramate13. _________________________________________________________________________ REFERENCES 1. National Institute of Health consensus statement. Management of the Clinically Inapparent Adrenal Mass 2002. Volume 19 (2) 2. Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y & Bornstein SR. The Clinically Inapparent Adrenal Mass: Update in Diagnosis and Management. Endocrine Reviews 25(2):309–340. 3. Barzon L et al. Development of overt Cushing’s syndrome in patients with adrenal incidentaloma. European Journal of Endocrinology (2002) 146 61–66 4. Funder JW, Carey RM, Fardella C, Gomez-Sanchez CE, Mantero F, Stowasser M, Young WF, Jr, Montori VM, Endocrine Society 2008 Case detection, diagnosis, and treatment of patients with primary aldosteronism: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 93(9):3266-3281. 5. AACE/AAES Medical Guidelines for the Management of Adrenal Incidentalomas . Endocrine practice 2009; 15 (Suppl 1) 6. Hamrahian H et al. Clinical utility of non contrast computed tomography attenuation value (hounsfield units) to differentiate adrenal adenomas/hyperplasias from nonadenomas: Cleveland Clinic experience. J Clin Endocrinol Metab 2005; 90(2):871-7. 7. Szolar D et al. Adrenocortical Carcinomas and Adrenal Pheochromocytomas: Mass and Enhancement Loss Evaluation at Delayed Contrast-enhanced CT. Radiology 2005: 234 (2). 479-485 8. Barzon et al. Risk factors and long-term follow-up of adrenal incidentalomas. J. Clin. Endocrinol. Metab. 1999 84: 520-526 9. Libe et al. Long-term follow-up study of patients with adrenal incidentalomas. European Journal of Endocrinology (2002) 147 489–494 10. Bulow B et al. Adrenal incidentaloma – follow-up results from a Swedish prospective study. European Journal of Endocrinology (2006) 154 419–423 11. Gopan T et al. Evaluating and managing adrenal incidentalomas. Cleve Clin J Med. 2006 Jun;73(6):561-8 12. Young W. The Incidentally Discovered Adrenal Mass. N Engl J Med 2007;356:601-10 13. Valassi E et al. Concomitant medication use can confound interpretation of the combined dexamethasone-corticotropin releasing hormone test in Cushing’s syndrome. JCEM 2009; 94: 4851-9. QUERIES Endocrine Specialist Registrar (referrals) bleep 6216 Endocrine Consultants Dr K Bradley, Dr B Ahmad Dr N Thorogood Prof S Lightman Prof A Levy Prof D Wynick via switchboard Version 1 Sept 2011 - Review Sept 2014 Author Dr Karin Bradley, Endocrinology Consultant Page 3 of 3