Med K Orientation
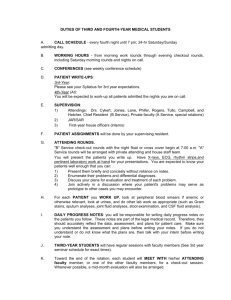
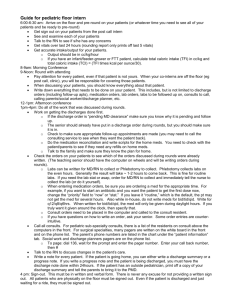
advertisement

July 24, 2009 MED K – ORIENTATION CHEAT SHEET Welcome to Med K, a unique medicine service that is rich with teaching and caring experiences. This can be a very fulfilling rotation and you will have opportunities to grow as well as greatly impact the health of patients under your care. Below are important responsibilities we stress on this service. Responsibility Morning Rounds Interdisciplinary Rounds X-Ray Rounds Attending Rounds White Boards Rounds Report Discharge Planning Satisfaction Surveys Expectations Pre-round M-F then Attending Rounds at bedside and always ending at 10am at which time the Resident goes to AM Report. Rounds must be efficient and structured to be completed in a timely fashion. The Attending and Resident will round with Social Work Case Manager and Charge Nurse M-F at 11:15am. M, W, F at 1:15pm. Two to three times per week. Med G and Med K will combine these didactic sessions. Collectively ‘owned’ by Medical, Nursing, Social Work, Ancillary Services (PT, OT etc), the boards in patient rooms are used to communicate important data (procedures, plans) to patients and their families. They should be kept up to date and accurate by all. At the end of each day the Rounds Report should be updated to reflect anticipated plans and on-going and future needs for the patient. Begin formulation of discharge plans at the time of admission. Where the patient will go to after release, medications coverage, central lines, PT/OT, O2, IV therapy, dialysis, all must be anticipated and planned for early. Encourage patients to complete these surveys, particularly the many patients who may have had a good experience. 1 Explanation We believe that there is value in the team rounding together in terms of continuity of care and teaching. This is an essential part of the day and aims to coordinate the care team to deliver service in an efficient fashion. Invaluable for care and learning. Required for teaching aims of the service. Patients often complain they are out of the loop. The white boards are popular and helpful in keeping patients up to date on plans. Use them. Social work uses the data in the report to work on plans while the team rounds in the morning. The goal is not to discharge patients from the hospital earlier than medically necessary but to reduce avoidable delays in discharge. A fraction of patients complete the survey and often these are those who have something to complain about. As the survey is used to gauge quality of service, encouragement of broader use will reflect our service. July 24, 2009 MEDICINE K WARD SERVICE ORIENTATION EXPECTATIONS and RESPONSIBILITIES for HOUSESTAFF and STUDENTS Welcome to Med K. This is a busy service and you will learn a lot in the short time you are part of our team. The Division of Infectious Diseases faculty members are very committed to ensuring that you have a first rate experience, both fun and educational. We also hope that at the end you will realize why all of us love our work so much. There are certain expectations that we want you to meet and that you should expect of us. Please read the following to better understand what it is we expect of you and what we will aim to provide to advance your training. If you have any questions please ask your attending. For All Team Members: 1. TAKE CARE OF YOUR PATIENTS: Most of you want to do well on this rotation. To receive a great evaluation you should behave like the physician you aim to become and take responsibility for your patient. The patient is ‘yours’ and that means they are your responsibility. You need to know everything about them. -Take a complete history and review all old records on your admissions: If the patient was transferred from another hospital, institution or referred from an outside physician, call that person/institution the day or night of admission and get a copy of the record faxed to the ward. If the patient is not a good historian then call family members. Call the microbiology laboratory at the outside hospital or the state TB laboratory if the patient had any cultures sent there and call again until the culture is final. (Important: Be sensitive to the fact that if a patient is HIV+, their family members may not be aware of the diagnosis.) -Perform a complete physical exam on each patient: It is not appropriate for housestaff or students to take short-cuts such as “no focal findings” on neurology exam or “clear” on lung exam. Most physical findings need to be evaluated and described via inspection, palpation/percussion and auscultation. We expect you to do this. In particular, you need to learn what is appropriate in terms of a physical exam for particular findings or complaints. For instance, someone who is clearly dizzy and exhibiting symptoms of orthostatic hypotension, should have orthostatics performed. Someone with a brain mass needs a detailed neurologic exam. If a woman has abdominal pain, she needs a pelvic exam. If you need to open up your old Physical Diagnosis textbook, do so. -Physical exam instruments: Get ophthalmoscopes/otoscopes, reflex hammers, flash lights and tongue depressors. We will be assuming that you have such items. -Review the EKG on your admission so you know what it looks like. -Review the laboratory results: Look back at old microbiology results in patients with recurrent or chronic infections. -Visit radiology and ask the radiologist on call to go over the CXR, MRI, etc of your patients. Simply reading ARTAS reports is not optimal. All films, and abnormal radiographs 2 July 24, 2009 in particular, must be inspected by you with a radiologist, if not at the admission then at Xray rounds. -Aim to make a diagnosis the day of admission. Writing orders for sputum gram stain is not sufficient. It needs to be done! Pretend the patient is a relative, would you like them to sit around waiting for the diagnosis? -Learn from patients and their families. Take the time to listen to their stories, their lives and learn how they cope. -Take responsibility for your patients. You should know every test result and every event that happens to your patient as well as each medication they are taking. There will be little tolerance for not knowing results of cultures or serological tests or the medication list. -Progress Notes: With WebCis there is a great temptation to cut and paste from prior notes to the next. This renders these important sources of information useless. This will not be acceptable on Med K. Make certain that the information in the progress note is up to date and informative, reflecting the events and discussions of the day. Up date problems lists, medications, procedures and assessments every day. -Discharges: Start discharge planning on admission. Consider where the patient will go to next and anticipated needs such as oxygen, IV antibiotics, ability to afford medications, PT, OT, dialysis etc. If a PICC or central line is needed, order sooner rather than later. All patients must have a clear understanding of their diagnoses, discharge medications, and follow-up, including a way to get their prescriptions filled. This MUST BE DOCUMENTED will not happen unless the person taking care of them ensures it. The medication instructions for patients must be written in lay terms. The intern must meet with the patient to go over their medications and follow up appointments. Only a licensed clinician should do this. Discharge summaries must be dictated the day of discharge. All HIV+ patients can receive a post-hospitalization appointment in the ID Clinic. Call Lynda Bell at 6-7199 to arrange. -Think ‘big picture’. If a patient keeps getting admitted for an illness, either you have the wrong diagnosis or something is happening to the patient that is making them sick, either environmental or social. 2. ROUNDS AND TEAM LEARNING. There are ample opportunities for independent and group learning during your rotation. -Independent learning: You are expected to read about the diseases your patient may have, their diagnosis and management. For the resident and medical students, you should be a source of information to the interns and team as a whole. You need to pull articles (not just UpToDate) and share what you read with your busy interns and team-mates. Rounds: -Morning Work Rounds – The morning work rounds are critical to the dual missions of patient care and medical education. All team members should arrive on time and prepared to discuss the details of the care of patients for whom you are caring. Rounds will start at a time that will allow for each patient to be seen and discussed prior to 10 am when the resident must be at Morning Report. Rounds will be efficient and focused. 3 July 24, 2009 Pre-rounding before Morning Work Rounds is essential and will avoid surprises during work rounds. On rounds, the intern or student must be prepared to formally present on new and established patients. The resident and attending will provide teaching at the bedside and assess presentations for organization, accuracy and style. This is a chance for students and interns to shine! Always pay attention to patient comfort and privacy (draw curtains, close doors, turn back on TVs, etc). Proper infection control techniques must be followed. -Social Work Rounds – Every day, typically at 11:15 am, the attending and resident should meet with the ward social workers and clinical care coordinators to discuss discharge planning, coordination of inpatient services and referrals and outpatient access to care. It is unacceptable to send a patient home on new medications that he or she cannot afford. This meeting is crucial to maintaining a reasonable ward census and coordinating essential services for our patients. If you cannot make these rounds, out of courtesy, let the social worker know. See the Social Work Survival Guide below for helpful contact numbers and advice. -Attending Teaching Rounds – At least two times a week, the attending will ask that the team convene for formal sit-down teaching rounds. This should be a protected time dedicated to learning. Ask questions, bring papers to discuss. When paged out of rounds, please inform the caller that you are in attending rounds and will call them back. All efforts will be made to combine Med G and Med K teaching rounds. -Radiology Rounds – As part of the teaching experience we will round with a radiologist three times a week (every Monday, Wednesday and Friday at 1:15 pm). Attendance is mandatory and we are certain you will find this to be a very useful and enlightening experience. Bring a list of films you want to review. -Wednesday Morning ID Rounds – The Med K team is expected to attend the Med K conference every Wednesday morning at 8:30 am in the 5th floor Orthopedics Conference Room. Unknown cases from the ward and consult services will be presented. Students who volunteer to present cases are typically praised for their initiative. -Morning Report – Residents must go to morning report except on Wednesdays when the ID conference occurs. We mean it. 3. GENERAL TIPS -Dress appropriately for working hard and follow the hospital dress code. -Be nice to ancillary personnel such as the nurses, aides, pharmacists, social workers and secretaries. They work hard and appreciate your acknowledgement of their role in the health team and they’ll make your life easier. Remember, they too are your teachers. -Ask for help if you need it. -Never lie! It is much better to say ‘I don’t know.’ -Think prevention: flu, pneumovax, mammogram, PAPs, rectal, STD’s. -We understand that the socialization process of becoming a physician can be painful but thousands have gone through the process before and survived. Look in mirror every day 4 July 24, 2009 and say “I am a good person, a smart person and I would not be here if that were not true.” Trust the many hours of education and hard work that got you to where you are today. -If you are not having a good learning experience, tell the attending as soon as possible what can be done to improve your rotation. -If you have specific rotation requirements, i.e. observed complete physical exam, please tell the attending on the first day of the rotation. -Don’t get in arguments with other physicians, students, or staff about your patient’s care. If you think your patient needs something done and another health care worker refuses to do it then call your resident or attending to facilitate. -Don’t get the disease yourself and think about communicable diseases Never sit on the bed and always be on the look out for loose needles Never do a procedure using sharps if you are tired or don’t know what you are doing. If you stick yourself call your attending and resident immediately. 4. ATTENDING RESPONSIBILITIES TO HOUSESTAFF AND STUDENTS -Attending lectures. -Bedside teaching. -Accessibility to you for additional questions. -Feedback on performance, areas for improvement, presentations and write-ups early in the rotation. -For students, physical diagnosis rounds at least once a week. -Formal meeting with attending half way through rotation to give assessment. 5 July 24, 2009 For Medical Students DON’T BE PASSIVE, FIND LEARNING OPPORTUNITIES. Each patient provides a learning opportunity. There are no boring patients. The 63 year-old woman with a community acquired pneumonia and the 56 year-old man admitted to rule-out MI can both provide a wealth of learning for you. Learn why she was prescribed a quinolone and how the HCTZ he is taking works. As a first and second year student you are a dependent learner where you are told to memorize 10 facts, given a study guide on the 10 facts and then told the 10 facts that will be on the exam and then given the exam with 10 facts. As a third and fourth year student you need to realize quickly that what you learn is dependent on you taking the initiative to begin the life long process of learning medicine. -Students should not have to be told to jump in during rounds. If they hear of someone with a murmur of mitral regurgitation on working rounds, they need to take out their stethoscopes and listen with the rest of the team or come back later with the resident or attending. -Volunteer to do every procedure on every patient whether your own or not (i.e. starting IVs, central lines, chest, spinal and abdominal taps, putting in Foley catheters, etc). If you don’t do them you won’t learn them and will have a painful internship. This is your best opportunity to learn these procedures. -Help your intern and volunteer to stay over on your night on call to learn the cross-cover routine procedures such as a fever workup, mental status change, chest pain, acute SOB, and falling out of bed. You should be able to think of the differential and carry out the work up for these clinical scenarios in your sleep. -Don’t wait to be told to work up a patient, keep asking your resident if there is a patient for you to see, even if it is not your on call day. -READ, READ, READ: We have a tendency here to gain "knowledge" by asking people superior (e.g. the resident asks the attending, the student asks the resident) and stopping there - instead of looking things up - both in texts AND in journals. It's OK to ask as a starting place (or even better AFTER looking it up). You should challenge your superiors make them back up their statements, rather than using them as the "gold standard". You should read and learn about every problem. Do PUBMED searches on your patient’s diagnoses. -WRITE UPS SHOULD BE THOROUGH: Patients come in with chief complaints and problems, not a list neatly divided up into cardiovascular, pulmonary, endo, etc. Therefore H&P’s should be problem focused. We want to see a detailed problem list where each problem is listed down to every laboratory and physical exam finding and that the distillation of how these inter-relate or do not is included in the discussion with a differential diagnosis for the top 1-3 complaints/findings. The difference between high pass and honors is that there is some evidence of independent learning which does not involve simply textbooks or Up-to-Date. Remember, honors is a grade bestowed for superior work. To get this grade you need to be extraordinary. On the Medicine Wards you need to order your discussion focusing on the different problems the patient has such as chest pain, diarrhea, headache, fever, etc and then list a differential diagnosis for each problem along with pertinent positives and negatives in history, physical exam and laboratory data and the 6 July 24, 2009 pathogenesis of your final idea as to diagnosis. Don’t regurgitate a textbook instead relate the discussion to your patient (See example below). Ask your resident for help with your write up. Write ups should be given to the attending within twenty-four hours of admission. PRESENTATIONS: There is an art to presenting information and it is perhaps one of the most important tasks a physician does other than diagnosing a patient’s illness. If you don’t convey the information accurately then the person assuming care may misunderstand you with disastrous consequences. Presenting to an attending. Most of us will want a 2 minute presentation. Ideally you should memorize the information, but you can use a 3x5 card if needed. This will force you to think about the patient, figure out what is important and what isn't, and present a coherent and concise story. The goal is to use the oral presentation effectively - like you would to communicate to a colleague. You must learn to distill all the information and think about what's important and make a reasonable differential diagnosis. In your presentation to the attending, tell a story, don’t wander and don’t editorialize. Read presentation out loud to yourself before presenting to attending so you can hear yourself editorialize and then delete it. Ask attending how you are doing and what needs to be done to improve 7 July 24, 2009 Social Work Survival Sheet for MDG/K Housestaff POE PAGER: 123POEH OR HELPDESK 65647 Patients are typically on 6BT 8 BT: 6-5441, fax # 919-843-0160 3 West: 6-2601 fax# 919- 843-0162 3 Anderson/ICCU: 6-1939 6BT: 6-5426 Fax # 919-843-0161 6WST-6-7025 Key resources: All available thru hospital directory. Care Coordinator: Carolyn Edmonds, RN Social Worker: Carroll Anstead, LCSW MPCU: 6-7483 Pager 216-3767 Phone 966-7850 Pager 347-0204 Phone 966-7876 Resident Assistant: Monique Kambaji Pager 347-1850 Other Resources: PT/OT: 6-2056 Speech: 6-2347 Interdisciplinary Rounds: Pls call CCM Staff if you’re not able to attend. MDK: 1115 am M-F. 6bt. MDG: 11am? M-F 6bt Skilled Nursing Facility (SNF), Assisted Living (AL), and Rest Home Patients Some facilities (Carol Woods, Carolina Meadows) have multiple levels of care. You must know what level the patient is coming from to determine if a return to the same level is appropriate. Notify CCM team when you can estimate the date of discharge. You need to do: FL2 form Stat discharge summary (dictate at least 2 hours prior to expected d/c) Green sheet orders Prescriptions, depending on the facility (check with Sherry) Ambulance transfer authorization form if needed Discharge times: Transfers to a new facility usually accepted only until 5pm Mon-Fri. Returns to previous facilities may be accepted on Sat on a case by case basis. Most facilities will “hold” a bed for a patient for a day or two. If longer is required, the pt/family must pay a daily fee to have the bed held. Note: NG/Corpak tubes are not accepted by SNF’s. Enteral feeds must be via PEG. Caring for Inmates Key information for inmates will be on yellow sheet in front of chart. Care Coordinators handle discharge planning and will identify which facility the inmate will transfer to. Dept of Corrections MD must accept the inmate back into the prison system prior to discharge. You should discuss an inmate’s condition with him/her and family just as you would with any other patient EXCEPT: NEVER DISCLOSE THE EXPECTED DISCHARGE DATE. (security risk) Advise the guard of a potential discharge outside of the inmate’s room as soon as you know it. Inmates may give their own informed consent. Next of kin may be contacted to provide consent for an incompetent inmate. Inmates may not have visitors (security risk) Guards are responsible for determining if and/or when an exception is made (very rare). You cannot override this decision. There is no early release/parole for hospice. The prison system can provide hospice services. Inmates/family have absolutely no input into discharge date or place. Do not give a prescription to an inmate. Inmates returning to low security facilities may need prescriptions for new meds, which should be given to the guards. Most inmates will return to facilities with a prison physician who will write orders for meds dispensed by the prison pharmacy. 8 July 24, 2009 The Care Coordinator and service Pharmacist have access to the Dept of Corrections Formulary. This can be helpful when starting an inmate on a new medication. If possible, discharges should occur prior to 2pm. This avoids having to bring in an additional shift of guards for the inmate. To discharge an inmate, you need to do: Discuss with Care Coordinator to verify the destination facility. You or Care Coordinator advise guards outside the inmate’s room. Identify if inmate is medically appropriate to travel by squad car vs. ambulance. -Call MD/prison official identified on yellow sheet (front of chart) to obtain acceptance for transfer back to prison system. -Once accepted, write pending discharge order/notify patient’s care nurse -Stat discharge summary @ least 2hrs prior to d/c time -Green sheets -Prescriptions (only occasionally, check with Care Coordinator) Dialysis Patients: Dialysis unit is located on 3 West (6-1382). You will need your ID badge to access. Dialysis Centers phone numbers are posted in back of the 3West Nurses’ Station over printer. New Start Dialysis patients need the following: Labs: Hepatitis B surface antigen and antibody and C antigens, Ekg in the last year, CXR in the last month, Chem 10,CBC and Albumin. HIV and PPD prn. Check with social worker. Vein Mapping should be done as well, with eventual surgical consult for fistula or graft placement. Please save non-dominant arm for future access. Limit venipunctures as much as possible. Can use hands for IV’s. LABS CAN BE DRAWN AT HD!! Dialysis Patient Discharges: (if patient received any dialysis while here)- You need to do: --A STAT dictated discharge summary, cc/faxed to Dialysis Center --Fax the “green d/c sheet” orders to HD center (Sherry will do this M-F) --Telephone the center if there are any changes in the patient’s regimen, i.e. antibiotics post dialysis -- ------Any new orders ie: dry wt, or changes in dialysis orders need to be communicated to the outside dialysis unit. --ABX at HD: Document in d/c summary abx, last dose given, when abx due, last level. Attending needs to call attending at dialysis center with orders( Carolina Dialysis centers require an order for all antibiotics to be given during dialysis signed by the attending or fellow) National Kidney foundation guidelines can be found at www.kidney.org/professionals/dogi/guidelines/doqiupva_v.html Should you be interested in a copy please let me know. IV Access for post-discharge antibiotics: PICC line is appropriate for: Short term (2-6weeks) IV abx @ SNF or home. Longer term therapy may need a different catheter (Hickman) The PICC RN team must evaluate patient for possible bedside placement first. If the patient is not a candidate for a PICC, write an order for placement in VIR and calling VIR in addition (6-4645). As soon as need for post-discharge antibiotics is identified, You need to do: -Write order: “ PICC RN to evaluate for PICC line. Anticipate d/c on ____ for ___ weeks home abx.” Write this when need identified, even if over a weekend. (PICC team phone: 6-3132, pager 216-8219) -For D/C to home: Inform your CCM staff and Call Home Infusion Nurses (phone: 60969, pager 123-4280) to advise. Write drug order on Green Sheets and sign. (allows outside pharmacy to order drug prior to D/C) -For D/C to SNF/Facility: Notify CCM. Assure IV med and duration is on FL2 PHYSICAL and OCCUPATIONAL THERAPY REFERRALS 9 July 24, 2009 Before writing the order: What is the benefit of the referral?? Guidelines for PT and/or OT (examples): Patients who have a functional decline (PT), self-care deficits (OT) Post-op chest/CABG (PT) Acute strokes (PT/OT) Neuromuscular patient on PLEX and IVIG protocols (PT) MS patients on IV steroids (PT) Patients who have recent falls who may benefit from assistive device (PT) Patients needing family training prior to d/c/assessment of equipment needs (PT or OT) Patients who have had a prolonged hospital or ICU stay (not on day of d/c) General debility patients, recommendations for level of care changes Revised 3/07 10 July 24, 2009 Example of a write up: Cc: 58 year old male comes in c/o crushing chest pain over his left chest which moved into his left arm. HPI: This man was in his usual state of health when shortly after finishing his morning jog he developed crushing chest pain over his left chest which moved to his arm and was associated with sweats, nausea and dizziness and lasted 20 minutes. He called EMS but the pain was over by the time they arrived. His history is remarkable for hypertension, diet controlled hyperglycemia, smoking one ppd for 20 years and a positive family history for heart disease with a father dying at age 48 of a heart attack. He has never had chest pain previously. He denies having a history of hypercholesterolemia. There was no relationship of the chest pain to a meal and it was not positional. No prior history of esophageal or gastric disease. No prior history of pulmonary disease. ROS: List out. All: None FH: CVD in father. Mother died of breast cancer at age 70. Two brothers alive and well. No children SH: Smokes 1 PPDx 20 yrs. Does not drink alcohol or use illicit drugs. Works as professor and lives in own home. Has State Health Plan for insurance. Sexually active with wife of 29 years, states monogamous PMH: No previous surgery or hospitalizations. Medications (use generic name): hydrochorthiazide 25 mg daily PE: Lying BP 160/100 HR 100 37.5 po Standing 160/100 115 RR 18 Adenopathy: No cervical axillary or inguinal adenopathy Ears: No exudates, TM’s clear Eyes: PERRLA, Discs sharp, conjunctiva clear Oropharynx: No lesions Neck: Supple without thyromegaly. Chest: Symmetrical rib movement. No dullness to percussion. Clear to auscultation. 11 July 24, 2009 Cardiovascular: no JVD. PMI 4th ICS, midclavicular line. S1, split S2 with a soft holosystolic murmur heard best at the apex. (DRAW PICTURE) Abd: BS present in all 4 quadrants. Soft non tender with no palpable spleen. Liver span is 10 cms. (DRAW PICTURE OF ANY SCARS) GU: Testes descended with no masses or tenderness. Circumcised penis with no lesions. Rectal: No mass, small firm prostate without lesions. Stool brown, guaiac negative. No CVAT Ext: No cyanosis, clubbing or edema. Pulses. Normal pulses PT, DP, femoral, radial and carotid. No carotid bruits. Neuro: Alert and oriented x 3. CN 2 through 12 intact (list out). Motor strength: List out by muscle group. Sensation: Nl pin prick, light touch and position sense both legs and arms as well as torso. Cerebellar: Nl FNF and Heel to Shin, rapid alternating movement. Reflexes: Draw and test all including Babinski Labs: CK 56 MB 3.5 Troponin T <0.029. Repeat 4 hours later: CK 140 MB 6.6 Troponin T 0.094. Normal ALT, AST, CBC and diff. CXR clear lung fields with no cardiomegaly. EKG: Normal sinus rhythm with a rate of 70/min. Normal axis and intervals. Symmetrical T wave inversions in leads II, III, and aVF. Discussion: This 58 year old male presents with symptoms of an acute coronary syndrome. Evidence supporting this diagnosis is the history of crushing chest pain radiating to his left arm after exertion, cardiac risk factors of smoking, hypertension, hyperglycemia and pos FH as well as cardiac exam of a murmur of mitral regurgitation suggesting papillary muscle dysfunction and EKG findings suggesting myocardial ischemia.. There is no evidence that the patient had esophageal spasm or reflux or history for it, was not associated with eating or position. Also, there is no evidence for a pulmonary cause for his chest pain as his CXR was clear and there is no evidence of peripheral deep venous thrombosis. His clinical history and exam findings do not suggest acute pericarditis. Acute coronary syndromes encompass a spectrum of clinical disorders that are characterized by an imbalance in the energy supply and demand of the myocardium. The etiology is usually the formation of thrombus at the site of a pre-existing atherosclerotic plaque. This patient has experienced a non-ST segment elevation myocardial infarction (NSTEMI) – there is myocardial necrosis as evidenced by the elevation in troponin, but no electrocardiographic evidence of transmural injury or infarction. Since thrombus formation is the inciting event in acute coronary syndromes, initial therapy includes treatment with anticoagulant and antiplatelet drugs. Heparin and low-molecular-weight heparin inhibit thrombin formation and activity, inhibiting 12 July 24, 2009 thrombus formation and facilitating thrombus resolution. Aspirin therapy, by inhibiting the amplification of the platelet activation process, also provides acute benefit. In selected patients, thienepyridines, such as clopidogrel, or antagonists of the platelet glycoprotein IIbIIIa receptors reduce the risk of recurrent ischemia or infarction. Anti-ischemic agents, especially nitrates and beta-blockers, are important elements of therapy in patients with NSTEMI. In high risk patients, coronary angiography and revascularization reduce the risk of cardiovascular events and rehospitalization. The long-term management of patients who present with acute coronary syndromes includes blood pressure control, lipid-lowering therapy, smoking cessation, dietary modification, and regular aerobic exercise. References: Libby P. Current concepts of the pathogenesis of acute coronary syndromes. Circulation 2001;104:365-372. Gluckman TJ, et al. A simplified approach to the management of non-ST-segment elevation acute coronary syndromes. JAMA 2005;293:349-357. Mehta SR, et al. Routine vs selective invasive strategies in patients with acute coronary syndromes. JAMA 2005;293:2908-2917. 13