Efficacy of x-ray mammography screening in diagnosing breast cancer
advertisement

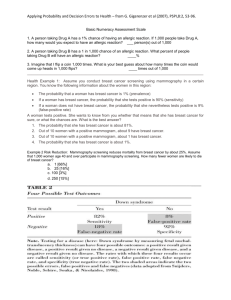
Efficacy of x-ray mammography screening in diagnosing breast cancer Author: Sahra Abdallah Haji Tutors: Dr A. Dora Dr C. Elwell 1 page of 7 Contents Executive Summary…………………………………………………………………...2 What is x-ray mammography?.......................................................................................3 How age affects the mammogram………………………………………………..……4 Alternatives to mammography………………………….……………………..…...….6 Is x-ray mammography efficient? ………………………………………………...…..7 Executive Summary Mammography is an apparently safe procedure that is carried out with the minimum radiation exposure possible. But, how efficient really is mammography in reducing the death rate due to breast cancer? Is it worth using it to diagnose breast cancer when the procedure could itself cause cancer? This report aims to evaluate the risks of having a mammogram for women of different ages. Alternatives are also considered. It should be used by medical specialists to assess whether it is worth screening a female patient since breast cancer is more prevalent in women than men. 2 page of 7 What is X-ray mammography In 1895, Wilhelm Roentgen took an x-ray image of his wife’s hand, Bertha. This was only shortly after having discovered x-rays. The image was made possible because xrays are largely absorbed by materials of high densities such as bone. As a result, these show up as white areas on x-ray film. Mammography is a diagnostic imaging examination that exploits this property of xrays. It is significantly useful for the early detection and treatment of breast cancer since it can spot cancers as small as a grain of table pepper (1). These can be easily missed when taking a self examination as they are too small to sense. The overall procedure should only take about ½ an hour or less. It involves tightly compressing the breast between two parallel plates. A pulse of x-rays is then used to take the image. The x-ray dose is low, usually around 2.03 mGy (2, 3). During the procedure, the breast is flattened to evenly spread out the tissue (4). Resultantly, the xray attenuation is about the same for the overall region of the breast. In addition, the radiation dosage absorbed by the breast is at a minimum. The craniocaudal view of the mammogram, looking vertically down on the breast, is the most anatomically recognisable. It is the main one used to determine whether abnormal growths, cysts or tumours are present in the breast. These appear as areas of abnormally high density in comparison to normal breast tissue. (5) Figure 2- Craniocaudal view f right breast Figure 2 - Mediolateral oblique view of left breast (6) Nonetheless, other views such as a medio-lateral oblique view, looking at the breast from the opposite shoulder, are also taken. This is so that the densities of the tissue can be compared from different angles. Comparisons of mammograms helps reduce the probability of false positives and false negatives (7). 1 www.ehealthmd.com/library/hrt/HRT_glossary.html http://www.ingentaconnect.com/content/rsm/jms/1998/00000005/00000002/art00006 3 http://bjr.birjournals.org/cgi/content/abstract/73/867/278 4 http://www.cancer.org/docroot/PED/content/PED_2_3X_Mammography_and_Other_Breast_Imaging _Procedures.asp 5 http://brighamrad.harvard.edu/Cases/bwh/images/268/reillymammo1.gif 6 http://breast-cancer-research.com/content/2/6/392/figure/F1 7 http://cmic.cs.ucl.ac.uk/studentships/ 2 3 page of 7 How age affects the mammogram Over the past century, there have been a number of medical debates over the age at which regular screening should commence. In the UK, most women between 50 and 70 have been invited for a mammogram every three years since 1988 (8,9). But, younger women from about the age of 34 can be screened as well especially if these women have first-degree relatives that have had cancer. “Mammographic screening before age 50 years is less effective than at older ages and the associated radiation risks are higher. (10)” This is because young women have denser breasts (11) that contain microcalcifications (12) and have thick epithelial tissue. As a result, a younger woman’s breast absorbs more of the radiation from the surface (13). Therefore, the radiation is less likely to penetrate deeper into the breast tissue, which is the area where malignant cancers are most likely to be found. Microcalcifications are calcium ions, which are spread out inside the fatty tissue of the breast in an inhomogeneous manner. As well as increasing the absorbed dosage of radiation, they reduce the image quality of mammograms. Consequently, it is difficult to differentiate between smaller cancers and the microcalcifications. This is very significant since the whole point of screening is to find the cancer in its early stages (14), before it has the chance to spread. If the internal features of the breast are ambiguous, then there is no point of taking the mammogram in the first place. Furthermore, it increases the probability of false positives. However, since breast cancer takes about 20 years to develop, it is less likely that young women have cancer anyway, Up to age 25, 1 in 15,000 (15) will develop breast cancer. This means that screening younger women unnecessarily exposes other organs to radiation, without contributing to the diagnosis. Since high density breasts absorb more radiation, the breast screening of young women may actually induce cancer. Sadly, cancers grow more rapidly in younger women (16). So, there’s an increased risk of them developing the induced cancer. Fortunately, breast density is not constant throughout women’s lifetimes (17). Older women tend to have smaller breast density. Additionally, as women get older, the thickness of the epithelial tissue decreases. On a mammogram, epithelial tissue would normally appear white and make the internal features of the breast harder to distinguish from the surface. But, not only do older women’s breasts have thinner epithelial tissue and low breast density but they also have higher fat content. The 8 http://www.cancerscreening.nhs.uk/breastscreen/publications/nhsbsp-the-facts-english-2007.pdf http://www.cancerscreening.nhs.uk/breastscreen/ 10 http://www.nature.com/bjc/journal/v93/n5/full/6602683a.html 11 http://www.medicalimagingmag.com/issues/articles/2003-05_01.asp 12 http://www.medicalimagingmag.com/issues/articles/2003-05_01.asp 13 http://bjr.birjournals.org/cgi/content/abstract/73/867/278 14 http://www.netdoctor.co.uk/health_advice/examinations/mammography.htm 15 http://www.cancerscreening.nhs.uk/breastscreen/breastcancer.html 16 http://womens-health.jwatch.org/cgi/content/full/2004/1208/1 17 http://jnci.oxfordjournals.org/cgi/content/full/96/19/1432 9 4 page of 7 resultant effect is a higher mammographic sensitivity mammograms that are less problematic to interpret. (18) , which results in clearer Overall, this means it is more beneficial to image older women because they are more at risk of getting breast cancer anyway. Up to the age of 70, 1 in 15 will develop breast cancer at some time in their life (19). And so, older women are more likely to be diagnosed with breast cancer. In addition, the chances of inducing breast cancer from radiation, decreases with age (20). Therefore, it is unlikely to have been caused by the procedure. There are other factors, which are thought to affect how effective the diagnosis is. These are the ethnicity of the patient; whether the patient smokes and whether there is a family history of breast cancer. In addition, the patient’s menopausal status and how often the patient is screened can also have a significant consequence on how effective the diagnosis is (21). 18 http://jama.ama-assn.org/cgi/content/abstract/276/1/33 http://www.cancerscreening.nhs.uk/breastscreen/breastcancer.html 20 Cancers detected and induced, and associated risk and benefit, in a breast screening programme, The British Journal of Radiology, 74 (2001), 1121–1127 © 2001 The British Institute of Radiology 21 http://jama.ama-assn.org/cgi/content/abstract/276/1/33 19 5 page of 7 Alternatives to mammography There are other emerging options for detecting breast cancer and improving image quality: Full field digital mammography provides the high resolution (22) and contrast required to produce high quality mammographic images (23). Clinical trials in the US have suggested it could especially be useful for imaging ‘radiographically "dense" breasts’(24). Nevertheless, equipment and maintenance costs would be significantly more than the standard methods used (25). Hence, it would take too long to implement. Magnetic resonance imaging (MRI) is more sensitive than mammography ( 26 ). It can successfully image dense breast tissue as well as breast implants. These are difficult to image using traditional mammography. Furthermore, the images can be reconstructed in 3D so the exact positions of the cancer can be located. This is particularly beneficial for young women and those at high risk of getting cancer (27). It is safer because MRI does not use radiation thus it cannot induce cancer. Nevertheless, it is not the most cost-effective option. Currently, a yearly MRI screening is not recommended for women who have a breast cancer lifetime risk of less than 15% (28). Figure 3 - 3D MRI scan of breast from 42-year-old patient 22 http://books.google.com/books?hl=en&id=cRIEuSBBEAMC&dq=breast+imaging&printsec=frontco ver&source=web&ots=LnRVYKC0Jx&sig=1RiVQ6nDkrLHpPsVoXgKHzBrNcE#PPA416,M1 23 http://www.cancernews.com/data/Article/210.asp 24 http://www.cancernews.com/data/Article/210.asp 25 http://en.wikipedia.org/wiki/Mammography http://www.cancer.org/docroot/PED/content/PED_2_3X_Mammography_and_Other_Breast_Imaging _Procedures.asp 27 http://www.radiologyinfo.org/en/info.cfm?pg=breastmr&bhcp=1 28 http://www.cancer.org/docroot/PED/content/PED_2_3X_Mammography_and_Other_Breast_Imaging _Procedures.asp 26 6 page of 7 Is x-ray mammography efficient? Breast cancer is one of the major causes of death from cancer for women and is second only to lung cancer (29). So, doctors obviously need to have a fast, safe and economically effective way of diagnosing the illness without making it worse. This should also lead to a clear reduction in the mortality rate from breast cancer. X-ray mammography is still used because most doctors believe the benefits of finding out whether a patient has breast cancer far outweigh the risks of inducing the cancer. Nonetheless, the main arguments against x-ray mammography are false positives, false negatives and inducing cancer. False positives cause patients to become stressed. They may find it hard to cope with being told that they have cancer, only for them to be told later that it was a mistake. However, this mostly applies to younger women since they are more likely to be diagnosed with false positives. False negatives, allow the cancer to develop since the cancer is not discovered straight away. Again, this affects younger women more because a cancer lump could be mistaken for a microcalcification. For a two-year screening interval, the ratio between the number of cancers induced to those prevented is 1:242 for 50-69 and 1:66 for 40:49 years of age (30).. This ratio would decrease for a three-year screening interval. This is sufficient evidence to show that mammography screening for women between 50 and 69 years of age, is more beneficial than for women who are 40-49 and younger (31). In the UK, breast cancer is being detected earlier for women aged 50 and over (32). Furthermore, largely due to the implementation of the NHS Breast Screening Project, there has been a reduction in the mortality rate due to breast cancer (33). This means that breast screening in the UK seems justifiable, for now. 29 http://books.nap.edu/catalog.php?record_id=11016 http://www.ingentaconnect.com/content/rsm/jms/1998/00000005/00000002/art00006 31 http://www.iarc.fr/ENG/Press_Releases/archives/pr139a.html 32 http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T1B-41CNTJ62&_user=5193083&_origUdi=B6T1B-41CNTJ6S&_fmt=high&_coverDate=01%2F08%2F2000&_rdoc=1&_orig=article&_acct=C000010182&_versi on=1&_urlVersion=0&_userid=5193083&md5=1f85f74265d2a41539073ff13d1f229c 33 http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6T1B-41CNTJ62&_user=5193083&_origUdi=B6T1B-41CNTJ6S&_fmt=high&_coverDate=01%2F08%2F2000&_rdoc=1&_orig=article&_acct=C000010182&_versi on=1&_urlVersion=0&_userid=5193083&md5=1f85f74265d2a41539073ff13d1f229c 30 7 page of 7