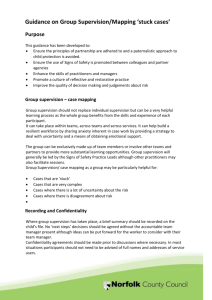
Supervision of the clinical workforce policy
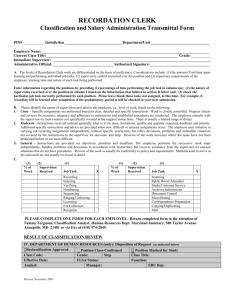
advertisement

Document name: Supervision of the clinical workforce policy Document type: Policy What does this policy replace? Update and alignment of previous SWYT and NHS Barnsley supervision policies. Staff group to whom it applies: Distribution: All staff employed by the Trust who have direct clinical contact with service users or provide supervision to those staff, including doctors in training. The whole of the Trust How to access: Intranet Issue date: October 2012 Next review: July 2015. Extension to May 2016 agreed by EMT 14 January 2016 Approved by: Executive Management Team Developed by: Alison Hill, Lead Nurse Community Mental Health/ Facilitator of Clinical Supervisor Training Barnsley BDU Director of Nursing, Clinical Governance and Safety Director leads: Contact for advice: Professional/Clinical Leads 1 CONTENTS 1 2 3 4 5 6 7 8 9 10 11 12 Introduction .................................................................................................... 4 Purpose .......................................................................................................... 4 Definitions ...................................................................................................... 5 3.1 Management Supervision ........................................................................ 5 3.2 Clinical Supervision ................................................................................. 5 3.3 Safeguarding children supervision .......................................................... 5 3.4 Preceptorship .......................................................................................... 6 Duties .............................................................................................................. 6 4.1 Executive Management Team ................................................................. 6 4.2 Clinical Governance and Clinical Safety Committee ................................ 6 4.3 The District Director ................................................................................. 6 4.4 General Managers, Associate Medical Directors, Service Managers, Clinical Leads, Consultants, Medical Tutors and Team Managers ........... 6 4.5 Supervisors ............................................................................................. 6 4.6 All Clinical Staff ....................................................................................... 7 Equality Impact Assessment ........................................................................ 7 Dissemination and Implementation Arrangements .................................... 7 Supervision Standards for Practice ............................................................. 7 7.1 Management Supervision ........................................................................ 7 7.2 Clinical Supervision ................................................................................. 8 7.3 Safeguarding Children Supervision ......................................................... 9 Training ........................................................................................................... 9 8.1 Management Supervision ........................................................................ 9 8.2 Clinical Supervision ................................................................................. 10 8.3 Safeguarding Children Supervision ......................................................... 10 Process for providing evidence of compliance with the policy .................. 10 Process for providing evidence of assurance ............................................ 11 Process for review and revision ................................................................... 11 References ..................................................................................................... 12 Appendix A Equality Impact Assessment Tool ............................................................................ 13 Appendix B1 Supervision Requirements of the Yorkshire Deanery ................................................ 15 Appendix B2 Supervision Form for Doctors ................................................................................... 31 Appendix C Sample Document Supervision Standards for Practice ............................................ 32 Appendix D Clinical Supervision Proforma .................................................................................. 53 Appendix D2 Clinical Supervision Contract ................................................................................... 54 Appendix D3 Supervision Record 1:1 ............................................................................................. 56 2 Appendix D4 Supervision Record Group ....................................................................................... 57 Appendix E Safeguarding Children Supervision .......................................................................... 58 Appendix E1 Contract for Safeguarding Children Supervision ...................................................... 58 Appendix E2 1:1 Safeguarding Children Supervision Record and Action Plan ............................. 59 Appendix E3 Safeguarding Supervision Contact Sheet/Record of Supervision ............................ 61 Appendix F Minimum Learning Outcomes for Clinical Supervision Training ............................... 63 Appendix G Checklist for the Review and Approval of Procedural Document ............................. 64 Appendix H Version Control Sheet .............................................................................................. 66 3 Supervision of the clinical workforce policy 1. Introduction South West Yorkshire Partnership NHS Foundation Trust (SWYPFT) recognises the important role that the appropriate supervision of clinical staff plays both in contributing to high quality clinical and professional practice leading to improved outcomes for the people using our services and also in maintaining the well-being of our workforce. Supervision supports the implementation of the workforce development strategy and sits with the clinical governance framework. This policy describes the different types of supervision endorsed within SWYPFT and sets minimum standards for the supervision of all clinical staff. Some clinical areas or professionals may have further requirements that are over and above these minimum standards. This policy provides a framework for practice for all clinical staff within the Trust, including local authority staff working in integrated teams. The format of the policy was designed to meet standards 6.1 of the National Health Service Litigation Authority (NHSLA) standards (2012-13), Care Quality Standards (outcomes 7, 14 and 16) and complies with the Trust policy for the development, approval and dissemination of policy and procedural documents. It should be read in conjunction with: Nursing Preceptorship Programme Policy and Procedures on the Protection, Safeguarding and Promoting the Welfare of Children Appraisal Policy Medical Appraisal Policy/Appraisal for consultants and Appraisal for non-consultants Dealing with poor performance at work policy/procedure 2. Purpose The purpose of this policy is to provide a formalised framework for the facilitation and monitoring of supervision of all staff employed by SWYPFT who have direct clinical contact with service users* and those who provide supervision to those staff. The term ‘clinical staff ‘is used to describe all of those staff, whether or not they have a professional health care qualification. *The term ‘service user’ is used within this document to refer to any person in receipt of SWYPFT clinical services including carers. Supervision is a practice focused, professional relationship involving a clinician reflecting on practice guided by a skilled supervisor. No single model of supervision can be adopted across the Trust as services must use the model that enables best practice delivery, therefore one of the responsibilities of service managers is to ensure that the model in use within their service is fit for purpose, provide evidence of this and that supervision activity is taking place. 4 3. Definitions The Trust is committed to the notion of effective supervision and recognises that different types of supervision are required to provide an efficient and effective modern health service. There are four types of supervision formally recognised and supported by the Trust: 3.1 Management supervision – This is the setting and monitoring of management objectives with an individual and is guided by organisation, business unit and team/service business plans. All staff employed by the Trust have an identified line manager who has a responsibility to ensure that their members of staff undertake induction, comply with the Trust’s appraisal process and Knowledge and skills Framework (KSF) review and identify any training and development requirements. For staff providing direct clinical care this will also include some form of caseload review where focus will include promoting safety, quality, defensible practice and identifying safeguarding issues. All medical staff have an annual job plan review, where this is considered inappropriate for staff grade/speciality doctors they must complete a record of regular supervision (Appendix B2). 3.2 Clinical supervision – ‘is regular, protected time for facilitated, in-depth reflection on complex issues influencing clinical practice. It aims to enable the supervisee to achieve, sustain and creatively develop a high quality of practice through the means of focused support and development. The supervisee reflects on the part s/he plays as an individual in the complexities of the events and the quality of practice.’ (Bond & Holland 2010:15). Clinical supervisors will have undertaken specific training to carry out this role. Clinical staff depending on profession and role will have differing clinical supervision requirements; this policy seeks to establish the expectation of a minimum level of clinical supervision. Focus in the sessions is based on the needs/issues identified by the supervisee/s. 3.3 Safeguarding children supervision – ‘is a formal, accountable process involving one or more practitioners with a suitably experienced supervisor. It affords professional support and learning which enables practitioners to develop knowledge, skills and competence, assume responsibility for their practice and enhance safety and protection of children in complex situations.’ (SWYPFT Safeguarding Children Supervision guidance, 2012). Sessions are facilitated by supervisors who are trained in child protection supervision and are based around a safeguarding children supervision record and action plan. Safeguarding children supervision is specifically targeted at clinical staff working routinely with children and young people or those working with a parent whose child is subject to Child Protection/ In Need or Common Assessment Framework (CAF) plan or where there are emerging safeguarding concerns identified. 5 3.4 Preceptorship - It is acknowledged as good practice that health care practitioners at point of entry to the profession, following five years or more away from the profession and when undertaking new roles, should engage in a period of preceptorship. The purpose of which is to provide staff with a supportive, nurturing relationship which assists their development and minimises the risk of inexperienced practitioners being given responsibilities which are beyond their scope of practice and therefore provides a safer environment for the novice, their colleagues and the service user. This type of supervision will not be described in any further detail within this policy as it is has its own guidance as stated within the Nursing Preceptorship Programme. 4. Duties The following duties apply to this policy: 4.1 Executive Management Team - The Director of Nursing, Clinical Governance and Safety is the lead director for supervision within the Trust, supported by the Medical Director. The lead director will be responsible for engaging relevant stakeholders in the development of the policy and ensuring appropriate arrangements are in place for managing any resource implications, including dissemination and training and for ensuring that the most current version is in use and obsolete versions have been withdrawn from circulation. The Director of Nursing, Clinical Governance and Safety will also link with the District Directors and the Director of Human Resources to identify any problems with the implementation or monitoring of this policy. 4.2 Clinical Governance and Clinical Safety Committee - The Clinical Governance and Clinical Safety Committee is responsible for scrutinising the implementation and effectiveness of this policy and providing assurance to the Trust Board. 4.3 The District Director - The District Director is responsible for monitoring the uptake of supervision as part of their monitoring of performance indicators. They will draw the relevant managers attention to any performance issues on an exception reporting basis. 4.4. General Managers, Associate Medical Directors, Service managers, Clinical Leads, Consultants, Medical Tutors and Team Managers - General Managers, Associate Medical directors, Service managers, Clinical Leads, Consultants, Medical Tutors and Team Managers are responsible for ensuring that there are sufficient supervisors and resources, including staff release within their services to provide supervision in line with this policy. They are also responsible for provision of evidence that the supervision models in use are fit for purpose and the minimum level of supervision provided meets service need. 4.5 Supervisors - All supervisors are responsible for ensuring that they have received relevant training and are competent to provide whichever form of supervision they are facilitating. 6 4.6 All clinical staff - All clinical staff have a duty to ensure that they seek out and participate in supervision in line with this policy. 5 Equality Impact Assessment This policy has no differential impact on equality, as identified by the equality impact assessment tool, completed in line with the SWYPFT policy for the development , approval and dissemination of policy and procedural documents, see appendix A. 6. Dissemination and Implementation Arrangements Once approved, the integrated governance manager will be responsible for ensuring the up-dated version is added to the document store on the intranet and is included in the staff brief. 7. Supervision Standards for Practice It is the responsibility of the line manager to ensure that management, clinical and safeguarding supervision is available to all clinical staff within their service. It is the responsibility of clinical staff to undertake supervision in line with organisational and professional requirements and to draw any shortfalls to their line manager’s attention. Staff with professional leadership responsibilities will provide advice to managers and staff to support this process. 7.1 Management Supervision - Management supervision will be delivered through the Trust’s current appraisal system and is line-management led, with the exception of doctors in core training (including those who are not directly employed by the Trust) who will follow the supervision requirements of the Deanery, for guidelines see appendix B1. Supervision provision for junior grade doctors should follow the guidelines for core trainees as far as possible and as amended by the associate medical director for education and training. During induction in the first 4 weeks of employment, staff will be allocated a line manager who will provide their management supervision. Management supervision is carried out by the person/role indicated on the job description. It is hierarchical in nature and the agenda is dictated by the supervisory manager. It is compulsory as part of terms and conditions of employment. Access to management supervision is arranged at the discretion of the supervising manager. Management supervision includes an annual staff appraisal and additional meetings can be arranged in response to staff and service need. The environment chosen for management supervision must be conducive to facilitating confidentiality during the session. However, material from these sessions can be shared with the wider organisation where this is appropriate e.g. higher management, Learning and Development Department; in these situations it is good practice to inform the supervisee of the intention to share information however their consent is not required. Where a staff member fails to reach required standards managers should deal with the minor performance problems of their staff as they arise. Where these are on-going or significant the ‘dealing with poor performance at work’ policy/procedure should be followed and the staff member informed of the same. 7 Documentation of management supervision sessions must be maintained in line with standards for clinical record keeping, remaining the property of SWYPFT and should be filed within the staff member’s personal file. 7.2 Clinical Supervision - Without exception all clinical services should strive to embed a clinical supervision culture within their services. It is recognised within the organisation that services have varying levels of clinical supervision culture and that some services particularly those outside of mental health services may have been working to a lower minimum requirement which does not comply with the recommended minimum supervision of 12 hours per year (pro rata for part time staff) as directed in the previous SWYPFT supervision policy. There is a paucity of evidence within the nursing research literature to determine what could be a ‘gold standard’ for the amount of recommended time spent in supervision except in mental health where monthly supervision was considered most effective (Edwards et al 2005). All mental health services across the Trust should work to the 12 hours per year minimum requirement. Where services outside of mental health currently do not meet the 12 hours per year requirement and where the service can justify a lower level of clinical supervision for example where there is a low level of complexity and clinical risk associated with the work being undertaken, a minimum of 6 hours clinical supervision must be undertaken per year – this decision must be reviewed on a yearly basis by service managers to determine that this lower minimum level of supervision supports the development and improvement/maintenance of high quality, innovative and defensible clinical and professional practice. It is considered good practice that services formally produce standards for supervision, where supervision expectations for all staff within their service are made explicit, see appendix C for an example. Across all services staff providing clinical supervision must undertake their own clinical supervision at the higher recommended minimum of 12 hours per year, as research has showed a detrimental effect on supervisor well-being where effective supervision is not accessed (White et al 1998). Supervision of supervisors also serves as a quality control and meets the necessary governance requirements. Undertaking safeguarding children supervision and specialist clinical supervision as part of an academic course may be counted towards minimum clinical supervision requirements, unless this is not permitted professionally. Management supervision should not be included as part of the minimum hours. Clinical supervision may be facilitated within a group setting or on a one to one basis. It can be received from outside of the Trust with the agreement of the line manager and the understanding of the supervisee that they have a responsibility to check that organisational policy and procedure allows them to follow guidance/advice from external supervisors. Clinical supervision must be provided by practitioners with competencies in the relevant area of clinical practice. This will usually be from a member of the same profession however where professionally there is no requirement for this, clinical supervision may be delivered by practitioners outside of the supervisee’s profession providing their guidance reflects any differences in professional code of conduct/practice. Staff may choose their supervisor from the clinical supervisor list held by the Learning and Development Department or from lists held locally. 8 Clinical supervision is facilitated around an agreement or contract between the supervisor and supervisee that details the responsibilities of both parties and the boundaries of the sessions (see appendix D2 for template). All clinical supervision agreements/contracts must include details of the boundaries of confidentiality and should be reviewed annually. Documentation of clinical supervision sessions must be maintained in line with standards for clinical record keeping (see appendix D for pro forma). It is recognised that the confidentiality of these records is paramount in order to facilitate disclosure within the sessions and make the best use of clinical supervision. Clinical supervision agreements/contracts must always stipulate where confidentiality breach would occur, in all cases harm to self or others either real or perceived would result in a breach and where behaviour contravenes the practitioner’s code of conduct or the law. Supervisors may negotiate additional breach conditions as part of the agreement. Outside of the breach conditions detailed on the agreement/contract consent to share information should be obtained from the supervisee. Breaching of confidentiality without good cause could result in disciplinary action. Documentation should be stored securely to maintain confidentiality. 7.3 Safeguarding children supervision - Line managers should make new clinical staff aware of the safeguarding children supervision process and paperwork, including how to arrange supervision, as part of induction. All staff identified as requiring safeguarding children supervision because of the nature of their caseload or the nature of a particular case will have an allocated safeguarding children supervisor. Safeguarding children supervision will be based on a written contract which should be reviewed annually (see appendix E1). See the SWYPFT Policy and Procedure on the Protection, Safeguarding Promoting the Welfare of Children which incorporates the Safeguarding Children Supervision Guidance for further details on the practice and processes involved in safeguarding children supervision. At every session a Safeguarding Children supervision record will be produced which will include any actions identified in order to safeguard children (see appendix E2 & 3). Documentation relating to safeguarding children supervision is the property of the organisation and will be held securely by the Safeguarding Supervisor and a copy provided to the supervisee. It is the responsibility of the supervisee to record within the healthcare record that they have accessed safeguarding children supervision and any actions arising from this. 8. Training Supervisors will be trained to carry out the various types of supervision that conform to professional requirements. The demands for training will be identified through the annual training needs analysis programme, reflecting the training needs identified in supervision and through the KSF and medical appraisal process. 8.1 Management Supervision - Management supervisor training needs can be met through a variety of leadership and development opportunities which include mentoring, coaching and experiential learning as well as accredited and in-house formal training therefore development is considered an ongoing process. Managers should be confident in their knowledge of the appraisal and KSF process prior to carrying out staff appraisal, it is acknowledged that many of the skills required for supervision are transferable from other areas of competence. 9 8.2 Clinical Supervision - The quality of supervision is paramount to good practice and therefore all practitioners who express an interest in becoming a clinical supervisor should be assessed by their clinical/professional lead as having: Credible clinical practice Evidence of continuous professional development Qualities consistent with good quality supervision provision such as warmth, honesty, integrity, empathy, respect and the ability to be reflective. All practitioners who meet the above criteria and are supported by their clinical/professional lead must be supported by their line manager in order to access Clinical Supervisor training; this can either be accessed in-house or through accredited training depending on professional requirements. People who have attained clinical supervisor qualifications in other employ and who are supported by their team manager and clinical/professional lead to take on the clinical supervisor role should provide details of their past training and experience to the Learning and Development Department, to determine that their training meets the minimum learning outcomes recognised by SWYPFT, see appendix G. Whereupon if deemed satisfactory their name and contact details will be added to the clinical supervisor database. Clinical supervisor training is a one-off event however, there is an expectation that clinical supervisors will use their own clinical supervision to embed and further develop their skills. Supervisors who are subject to poor performance objectives should be advised by their manager that they must not carry out their clinical supervisor role during this period. Re-instatement to this role should be considered on the recommendation of both the team manager and clinical/professional lead. It is the responsibility of clinical/professional leads within the Business Delivery Units (BDUs) to monitor the number of clinical supervisors that are available in their clinical area and determine on a yearly basis the number of new supervisors required both to meet workforce demand and counteract staff turnover bringing this information to the attention of operational management. 8.3 Safeguarding Children Supervision - Safeguarding children supervisors must have attended the appropriate child protection supervision training to be able to facilitate supervision. Practitioners interested in becoming safeguarding children supervisors who have the support of their line manager and clinical/professional lead to pursue this role, should contact the Child Safeguarding Unit for information. Safeguarding children supervisor training is a one-off event however, there is an expectation that clinical supervisors will use their own clinical supervision to embed and further develop their skills. 9. Process for providing evidence of compliance with the policy To provide assurance that staff undertake the appropriate levels of supervision outlined in this policy, monitoring will be facilitated via the management supervision/appraisal process. For trainee doctors this will be facilitated via the Yorkshire Deanery. Staff are expected to provide evidence that they have met the minimum clinical supervision attendance requirement by producing their annual record of supervision record (appendix D1) as part of their annual appraisal. 10 The staff appraisal pro forma prompts managers to consider that staff have met their minimum supervision requirements, where this expectation has not been met it is the responsibility of managers to include future compliance with supervision requirements as part of the staff members objectives. Where compliance continues to be problematic ‘dealing with poor performance at work’ policy/procedure should be followed and the staff member informed of the same. Doctors in training will complete a monthly supervision form as required by the Yorkshire Deanery (appendix B2). These will be monitored by their tutor. The Senior Tutor in the Trust will advise the Medical Director of any concerns regarding the supervision of doctors in training, or raised by the Yorkshire Deanery. Trust doctors will record supervision in their portfolio, which forms the basis of their annual appraisal by their line manager or Medical Director. 10. Process for providing evidence of assurance Trust Board assurance will be through the Clinical governance and Clinical Safety Committee and through the performance monitoring process at Board level, as part of key performance indicators around staff appraisal (compliance with all supervision requirements will be monitored by line managers at staff appraisal). The Director of Nursing, Clinical Governance and Safety will provide exception reporting to the Trust Board and the Clinical Governance and Clinical Safety Committee where deemed appropriate. The Medical Director will provide assurance to the Trust Board and/or the Clinical Governance and Clinical Safety Committee that the supervision requirements of the Yorkshire Deanery are being met, and that the requirements of the supervision policy are being met by Trust doctors. 11. Process for review and revision The policy will be reviewed by the agreed review date, in line with the Trust’s Policy for the development, approval and dissemination of policy and procedural documents. This may be brought forward if earlier review is required, for example because of an identified risk or change in national policy. The Integrated Governance Manager will notify the lead director three months before the policy is due for review. The lead director will check the policy. If no amendment is required, this should be reported to the Executive Management Team for ratification by the review date and the policy will be reissued. If the policy requires minor amendments, the revised policy will be presented to the EMT. If significant amendment is required, the process described in the Trust’s Policy for the development, approval and dissemination of policy and procedure documents should be followed. 11 12. References Bond M. and Holland S. (2010) Skills of Clinical Supervision for Nurses 2nd Edition. Maidenhead: Open University Press Butterworth T. et al (2008) Wicked spell or magic bullet? A review of clinical supervision literature 2001-2007. Nurse Education Today 28 (3): 264-272 Edwards D et al (2005) Factors influencing the effectiveness of clinical supervision. Journal of Psychiatric and Mental Health Nursing 12 (4): 405-414 DoH (2006) From values to action: the Chief Nursing Officer’s review of mental health nursing. London: COI DoH (2000) Framework for the Assessment of Children in Need and their Families London: the Stationery Office HM Government (2011) No health without mental health: a cross-government mental health outcomes strategy for people of all ages. HM Government (2010) Working together to Safeguard Children London: DCSF HMSO (2004) The Children’s Act London: HMSO NHSLA (2012) NHSLA Risk Management Standards (standard 6.1 clinical supervision) Slone Graham (2006) Clinical supervision in Mental Health Nursing Chichester: Wiley SWYPFT (2012) Policy and Procedures on the Protection, Safeguarding and Promoting the Welfare of Children (incorporating the Safeguarding Children guidance and Guidance of Child Visiting) Intranet Document store SWYPFT (2012) Nursing Preceptorship Programme Intranet Document store SWYPFT (2011) Policy for the development, approval and dissemination of policy and procedure documents Intranet Document store Turner J and Hill A (2011) Implementing clinical supervision (part 1): a review of the literature. Mental Health Nursing 31 (3): 8-12 12 Appendix A - Equality Impact Assessment Tool To be completed and attached to any policy document when submitted to the Executive Management Team for consideration and approval. Equality Impact Assessment Questions: Evidence based Answers & Actions: 1 Name of the policy that you are Equality Impact Assessing Supervision of the clinical workforce 2 Describe the overall aim of your policy and context? The overall aim of the policy is to define and describe the Trust’s approach to supervision. Who will benefit from this policy? All clinical staff 3 Who is the overall lead for this assessment? Director of Nursing, Clinical Governance and Safety 4 Who else was involved in conducting this assessment? Lead Nurse for Community Mental Health Barnsley BDU 5 Have you involved and consulted service users, carers, and staff in developing this policy? See appendix H for the consultation process for this policy. What did you find out and how have you used this information? To refine the document. 6 What equality data have you used to inform this equality impact assessment? N/A 7 What does this data say? N/A 8 Taking into account the information gathered. Does this policy affect one group less or more favourably than another on the basis of: Where Negative impact has been identified please explain what action you will take to remove or mitigate this impact. If no action is to be taken please explain your reasoning. YES NO Race N Disability N Gender N Age N Sexual Orientation N Religion or Belief N Transgender N Carers N 13 9 10 What monitoring arrangements are you implementing or already have in place to ensure that this policy: promotes equality of opportunity who share the above protected characteristics eliminates discrimination, harassment and bullying for people who share the above protected characteristics promotes good relations between different equality groups, Have you developed an Action Plan arising from this assessment? This policy aims to align the previous SWYPFT supervision policy and the NHS Barnsley clinical /professional supervision policy and meet the requirements of the CQC and NHSLA. N/A 11 Who will approve this Executive Management Team assessment and when will you October 2012 publish this assessment. 12 Once approved, please forward a copy of this assessment to the Equality & Inclusion Team: inclusion@swyt.nhs.uk If you have identified a potential discriminatory impact of this policy, please refer it to the Director of Corporate Development or Head of Involvement and Inclusion together with any suggestions as to the action required to avoid/reduce this impact. For advice in respect of answering the above questions, please contact the Director of Corporate Development or Head of Involvement and Inclusion. 14 Appendix B1 – Supervision Requirements of the Yorkshire Deanery Yorkshire School of Psychiatry Learning Agreement August 2011 to February 2012 GMC Number: Name of Trainee: Training Scheme: Employing Trust: Contract type: Year of training: Training Period ST CT LAT SHO SpR GP 1 2 3 4 5 6 From: Locality: To: Specialty: At the first meeting the trainee and Educational Supervisor should read and sign a learning agreement. The trainee will: Take an active part in the appraisal process including setting educational objectives and developing a personal development plan Endeavouring to achieve the learning objectives by Utilising the opportunities for learning provided in everyday practise Attending formal teaching sessions Undertaking personal study Utilising locally provided educational resources Using designated study leave funds appropriately Acting on the principles of adult learning through: Reflecting and building on his/her own learning experiences Identifying his/her learning needs Being involved in planning his/her education and training Evaluating the effectiveness of his/her learning experiences The educational/clinical supervisor will: Be available for, and take an active part in, the appraisal process including setting educational objectives Ensure that the objectives are realistic, achievable and within the scope of available learning opportunities Ensure that help and advice is available Ensure that there is a climate for learning Ensure that an individual doctor’s timetable allows attendance at formal teaching sessions, is appropriate for his/her training needs and that there is a correct balance between training and service in the placement 15 Signature: Trainee Educational Supervisor Signature: Name (print): Name (print): Date: Date: What do you need to learn? You should base your personal development plan on the College curriculum. The curriculum can be found on the College website along with portfolios that will allow you to record your learning. Rather than listing all the curriculum objectives as learning objectives in your personal development plan, you should refer to the curriculum and portfolio in a statement about attaining the appropriate objectives for your year of training. As your training progresses you may be better able to specify particular objectives which you might list in your personal development plan. Different placements can offer different opportunities to gain curriculum competences. As you consider the opportunities available to you in each placement, you should plan how you intend to make the most of them. You can use feedback to develop your PDP to focus on the areas of improvement highlighted in the assessments. Developing your PDP As you progress, self evaluation, reflective practice, multi-source feedback and direct assessment will all provide different perspectives on your performance and development. It is important to be aware of what information you are using when setting your learning needs and that you are not missing important feedback that may be available to you. For example, if all your learning needs originate from one feedback source it may be worth re-examining what other information is available to you. How will these needs be addressed and by when? Your plan should identify what you intend to do during the year and in each placement, how you will develop your learning and, most importantly, how and when you will be assessed. While reflective practice is extremely important, one of the key goals of the program is to demonstrate through your portfolio, a series of assessments that show development against the Curriculum, and progression towards competence. Setting yourself a target is always a good way to ensure progress. Discuss and agree realistic and achievable targets for demonstrating progress with your educational/clinical supervisor and record them here. 16 PERSONAL DEVELOPMENT PLAN Record here development needs identified with the educational supervisor arising from discussions about the learning agreement at the beginning of each year. This PDP is one component of the learning agreement. It should be updated whenever there has been a change - either when a goal is achieved or modified or where a new need is identified. Date The date on which the development need is recorded What development needs have I? How will I address them? Explain the need. Explain how you will take action, and what resources you will need? Date by which I Outcome plan to achieve the development goal How will your practice change as The date agreed a result of the with your appraiser development for achieving the activity? development goal. Completed Agreement from your appraiser that the development need has been met (signature of appraiser/supervisor and date) 1. 2. 3. 4 5. 17 Date The date on which the development need is recorded What development needs have I? Explain the need. Date by which I How will I plan to achieve the address them? development goal Explain how The date agreed you will take with your appraiser action, and for achieving the what resources development goal. you will need? Outcome Completed How will your practice change as a result of the development activity? Agreement from your appraiser that the development need has been met (date and signature of appraiser/supervisor) 6. 7. 8. 9 10. 18 Postgraduate Deanery Yorkshire and the Humber School of Psychiatry Placement Report February 2012 - August 2012 Please complete this form electronically then print off and sign The purpose of this report is to inform the regular reviews that are conducted of a Psychiatry specialty registrar’s progress through structured training. The report should reflect your experience of the trainee’s performance during their clinical placement and should be discussed with the trainee before submitting. The report relates to two main areas: The Trainee Knowledge (relevant to the placement) Professional competencies Full name GMC Number Date of Birth National training number(higher trainees only) The Post or Placement Name of consultant supervisor Specialty/sub-specialty GMC number of supervisor Hospital /Institution Months From To ……day…..month……year ……day…..month……year 19 The training was full-time Please delete as appropriate The training was part-time and the ratio of part-time to full-time was……………. 1. Knowledge-base relevant to the placement Insufficient Evidence Needs Further Development Competent Excellent Anything particularly good? Areas for development 2. Professional Competencies If you are viewing this document electronically, the footnote will appear when you hover your mouse pointer above the relevant footnote number Insufficient Evidence Needs further development Competent Excellent 1. Providing a good standard of practice and care 2. Decisions about access to carei 3. Treatment in emergenciesii 4. Maintaining good medical practiceiii 5. Maintaining performanceiv 20 6 Teaching and training, appraising and assessing.v 7. Relationships with patients vi 8. Dealing with problems in professional practice vii 9. Working with colleaguesviii 10. Maintaining probityix 11. Ensuring that health problems do not put patients at risk x Anything particularly good? Areas for development Endorsement Endorsement by Supervisor I confirm that the above is based on my own observations and the results of workplace-based assessments and has been discussed with the trainee concerned 21 Name Signed Date 1 This competency is about the clinical assessment of patients with mental health problems. It includes history-taking, mental state examination, physical examination, patient evaluation, formulation and record keeping. It also includes the assessment and management of patients with severe and enduring mental health problems. Evidence to consider will include WPBA’s, particularly the ACE, mini-ACE, CbD and multi-source feedback 2 This competency is about the application of scientific knowledge to patient management including access to appropriate care, and treatment. Evidence to consider will include WPBA’s, particularly the ACE, mini-ACE, CbD and multi-source feedback 3 This competency is about the assessment and management of psychiatric emergencies. Evidence to consider will include WPBA’s, particularly the ACE, mini-ACE, CbD and multi-source feedback 4This competency is about the maintenance and use of systems to update knowledge and its application to professional practice. This will include legislation concerning patient care, the rights of patients and carers, research and keeping up to date with clinical advances. Evidence to consider will include WPBA, reflective notes in the trainee’s portfolio, the trainee’s Individual Learning Plan and any record of educational supervision that they have kept 5 This competency is about the routine practice of critical self-awareness, working with colleagues to monitor and maintain quality of care and active participation in a programme of clinical governance. Evidence to consider will include multi-source feedback, records of audit and research projects undertaken and the trainee’s reflective notes on these projects. 6 This competency is about the planning, delivery and evaluation of learning and teaching; appraising and evaluating learning and learners; supervising and mentoring learners and providing references. Evidence to consider will include multi-source feedback, completed Assessment of Teaching forms and any quality data kept by the relevant teaching faculty or programme 7 This competency is about the conduct of professional patient relationships, including good communication, obtaining consent, respecting confidentiality, maintaining trust and ending professional relationships with patients. Evidence to consider will include WPBA’s, particularly the ACE, mini-ACE, CbD and multi-source feedback 8 This competency is about handling situations where there are concerns regarding the conduct or performance of colleagues, handling complaints and formal inquiries, holding indemnity insurance and providing assistance at inquiries and inquests. Evidence to consider will include CbD, multi-source feedback and reflective notes, including critical incident reports 9 This competency is about treating colleagues fairly, by working to promote value-based nonprejudicial practice; about working effectively as a member and a leader of multidisciplinary teams; arranging clinical cover; taking up appointments; sharing information with colleagues and appropriate delegation and referral. Evidence to consider will include CbD and multi-source feedback 10 This competency is about maintaining appropriate ethical standards of professional conduct which may include the following: providing information about your services; writing reports, giving evidence and signing documents; carrying out and supervising research; properly managing financial and commercial dealings; avoiding and managing conflicts of interest and advising others on preventing and dealing with them and appropriately managing financial interests that may have a relevance to professional work. Evidence to consider will include CbD and multi-source feedback and your review of reports written by the trainee. 11This competency is about the doctor’s awareness of when his/her own performance, conduct or health, or that of others might put patients at risk and the action taken to protect patients. Behaviours you may wish to consider: observing the accepted codes of professional practice, allowing scrutiny and justifying professional behaviour to colleagues, achieving a healthy balance between professional and personal demands, seeking advice and engaging in remedial action where personal performance is an issue. 22 Postgraduate Deanery Yorkshire and the Humber School of Psychiatry Annual Structured Report 2011 – 2012 Please complete this electronically, print off and sign. This report is to be submitted to the Annual Review of Competence Progression panel by the trainee’s current educational supervisor, summarising the trainee’s learning Portfolio since the previous assessment. This report should be discussed with the trainee before submitting it. Section 1: Basic information Trainee’s name: GMC number: Training number (if applicable): Core Training Scheme (delete as appropriate): Leeds & Wakefield / Bradford & Airedale / Calderdale & Kirklees / Hull & East Riding /North Yorkshire Higher Training Scheme (delete as appropriate): General Adult Psychiatry / Psychotherapy /Child / Old Age /Learning Disability / Forensic Year of training as Core or Higher trainee (delete as appropriate)i.e. first year Higher Trainees leave One One/two/three/four/five/six/seven Name of Educational Supervisor submitting report: Position: GMC number: Placements from August 2011 – August 2012: Placement 1 Educational supervisor: 23 Dates of placement: Number of sessions if trainee flexible Placement 2 Educational supervisor Dates of placement: Number of sessions if trainee flexible 24 Section 2: EVIDENCE SUMMARY Workplace based assessments (WPBAs) in current placement/s Assessment Date assessment took place ACE (1) Outcome –numerical score for performance at this stage of training should be entered here (2) (3) Mini-ACE (1) (2) (3) (4) DOPs (1) (2) CbD (1) (2) Mini-PAT (1) (2) PSQ (1) (2) CP (1) (2) JCP (1) (2) AoT (1) (2) Other (please describe) 25 Experiential outcomes (evidenced by portfolio review) Activity Date/s Comments Psychotherapy Please record training as evidenced in portfolio. Also record any restraints in receiving training. Audits Please record title of one audit as evidenced in portfolio Research projects Publications Teaching Management development Presentations Examination progress (must review RCPsych exam feedback) Exam Date(s) taken Passed or failed Notes/action points Date(s) taken Passed Notes/action points MRCPsych Paper 1 Paper 2 Paper 3 CASC Other exams 26 Trainee has evidence that they have completed PMETB feedback form Yes/No Other outcomes Delete as appropriate Date Notes Reported adverse incidents Complaints Record if justified or unjustified in view of person who investigated complaint Sick leave Other leave (maternity, paternity, carers, compassionate) On calls completed (record number only) For trainees not on out of hours rota record number of assessments of individuals with a range of diagnosed conditions and with first line management plans conceived and implemented. 27 Section 3: Overall Summary 3. Professional Competencies In assessing these domains you should rate the trainee against your expectations for the current stage of training. When this report is completed in the final placement of a stage of training, you should assess against the standard expected for the completion of the stage. If you are viewing this document electronically, the footnote will appear when you hover your mouse pointer above the relevant footnote number Insufficient Evidence Needs further development Competent Excellent 1. Providing a good standard of practice and carexi 2. Decisions about access to carexii 3. Treatment in emergenciesxiii 4. Maintaining good medical practicexiv 5. Maintaining performancexv 6 Teaching and training, appraising and assessing.xvi 7. Relationships with patients xvii 8. Dealing with problems in professional practice xviii 9. Working with colleaguesxix 10. Maintaining probityxx 11. Ensuring that health problems do not put patients at risk xxi 28 2. Professionalism Anything especially good? Areas for development Concerns identified* Health I confirm/do not confirm that there are no health concerns that impact on this trainees fitness to practice Total days sick since last review – xxxx Probity I confirm/do not confirm that there are no concerns in relation to probity for this trainee Complaints/adverse incidents (or none) * Where cause for concern is documented the basis for this must be clear and explicit Please delete as necessary Section 4: TRAINER DECLARATION I confirm that (tick as appropriate): I understand that I have a professional duty to document any concerns identified AND I have reviewed the evidence required to demonstrate fitness to progress for the relevant year of training and consider the trainee fit to progress and suitable for a career in psychiatry OR I have concerns about this trainee which have been documented in the report Print Name ________________________ Signed _________________________ Date _______________ Section 5: TRAINEE DECLARATION I confirm that: The evidence provided to inform my annual review is a complete, accurate record of the evidence collected and assessments undertaken during the relevant training period Print Name ________________________ Signed _________________________ Date _______________ 29 Section 6: COLLEGE TUTOR DECLARATION The college tutor should verify this review. I confirm that: I have checked this review and can confirm that to the best of my knowledge it represents a complete and accurate review of the trainee’s evidence Print Name ________________________ Signed _________________________ Date _______________ 30 Appendix B2 – Supervision Form for doctors SUPERVISON RECORD NAME: DATE OF SESSION: SUPERVISION KEY DISCUSSION POINTS: AGREED ACTIONS: SIGNED: SUPERVISOR’S NAME: SUPERVISOR’S SIGNATURE: Please complete after your supervision session and bring to the next session for sign off by your supervisor. Ensure this record is kept for appraisal / revalidation purposes. 31 Appendix C Sample document supervision standards for practice SAMPLE DOCUMENT SUPERVISION STANDARDS for CLINICAL STAFF WORKING WITHIN COMMUNITY MENTAL HEALTH SERVICES BARNSLEY BDU Authors: Alison Hill, Lead Nurse, Sandra Keen, Deputy Manager Community Mental Health, Jude Mitchell, Lead OT, Lisa Tattershall, Senior Social worker and Lisa Winter, Consultant Psychologist, Julie Warren-Sykes, Designated Nurse for Safeguarding (Mental Health) Acknowledgements to Clinical Leads: Joanna Burton, Rachel Butterworth, Eamonn Lynott and Mark Stoud for their help in shaping this document. 32 CONTENTS Page 1. Introduction. 3 2. Purpose. 5 3. Roles and Responsibilities. 6 4. Standards for Practice 4.1 Management Supervision 8 4.2 Clinical Supervision 10 4.3 Safeguarding Children Supervision 17 5. Auditing the standards 18 6. References. 19 7. Review of the standards for supervision. 20 8. Appendix Record of clinical supervision one to one. (D3) Annual record of clinical supervision session. (D1) Record of Group clinical supervisor session.(D4) Contract form – supervisor/supervisee.(D2) Clinical Supervision Audit pro forma REMOVED Safeguarding Children Supervisee record (E6) Safeguarding Children Supervision contract (E1) Safeguarding children personal development plan (E4/E5) Management supervision pro forma (3) 33 1 INTRODUCTION 1.1 Community Mental Health Services recognises the importance of supervision in contributing to the development of practitioners and improving the quality of service delivery. 1.2 This document provides standards of practice for all staff within the Community Mental Health Business Unit in relation to the supervision of their work and includes managerial supervision, clinical supervision and safeguarding children supervision. It should be read in conjunction with SWYPFT Policy Supervision of the Clinical Workforce, Barnsley Metropolitan Council (BMBC) Adult Social Services Directorate Supervision Procedure and SWYPFT Policy and Procedures on the Protection, Safeguarding and Promoting the Welfare of Children. 1.3 Managerial supervision provides a framework of accountability for the service and facilitates the escalation of clinical and non-clinical issues to the point within the organisation that has the authority to deal with them. It also formally facilitates staff development via staff development reviews (SDR) and monitors staff performance. The primary focus of managerial supervision is effective service delivery and patient welfare. 1.4 The functions of management supervision can be described as the bringing together of people and resources to achieve the goal of providing good quality care and treatment for people with mental health needs. This will include the effective organisation of work/workload and delegation of responsibilities, monitoring of activity and performance, identification of development needs and contributing to safe working practice. 1.5 Clinical supervision supports the implementation of the organisational development strategy and sits within the clinical governance framework, it is not a management tool, but rather a support for the development and improvement or maintenance of high quality clinical and professional practice in the delivery of patient care. The primary focus of clinical supervision is staff development/welfare and the delivery of high quality care. 1.6 The functions of clinical supervision have been described by Proctor (1986) as: Formative – the educative process of developing skills Restorative – supportive help for professionals working constantly with stress and distress and; Normative – concerned with developing competent practice, the internalisation of professional ethics, standards, self management and monitoring. 34 Within the knowledge and skills framework (DOH 2004) staff are required to provide evidence of their professional development, clinical supervision is one means of achieving this. 1.7 Safeguarding children supervision is a formal process of professional support and learning which aims to ensure that clinical practice safeguards children and promotes their welfare. 1.8 Safeguarding children supervision is achieved by facilitating reflective discussion, assessment, planning and review, thereby supporting the development of good quality, innovative practice provided by safe, knowledgeable and accountable practitioners. Sessions are facilitated by supervisors who are trained in child protection supervision and are based around a Safeguarding Children developmental plan. 1.9 The Community Mental Health Service is committed to the notion of effective supervision and recognises that different types of supervision are required to provide an efficient and effective modern mental health service whilst at the same time ensuring staff are supported and encouraged to reach their professional potential. 2. PURPOSE 2.1 The purpose of this document is to provide standards of supervision; managerial, safeguarding children and clinical for all clinical staff working with the Community Mental Health Business Unit. Different types of supervision particularly management supervision and clinical supervision are often different to define and distinguish one from the other (Yegditch, 1999), this document attempts to provide a working framework to assist staff in the implementation of managerial, safeguarding children and clinical supervision. 2.2 The aims of managerial supervision are: To assist in the delivery of the service to those people with mental health needs as described in the operation policy of the specific team/service. This includes, contributing to improving quality, timely service delivery and cost effectiveness (which includes staff performance and use of resources). 35 As part of the above duty the manager will be required to assess the performance of the individual staff member through Staff Development Review and identify any training requirements they have. The manger will jointly with the staff member identify and agree individual objectives that will add to the improvement of service delivery. To monitor that staff are working within the policy and procedures set down by SWYPFT and to take action where this is found not to be so. To escalate and issues that increase clinical/organisational risk through the management structure to the point where there is the appropriate authority to deal with them. 2.3 The aims of clinical supervision are: To facilitate staff to critically reflect on their practice through the medium of reflective practice. To safeguard standards by facilitating the internalisation of professional standards/conduct, ethics and self-management To develop professional expertise, clinical skills and promote the use of evidence based practice. To encourage a culture of continuous quality improvement To share and utilise knowledge To explore beliefs and values around the concept of recovery from mental illness. To acknowledge the staff member as a sentient being and facilitate the expression of emotions. To provide an enabling process that allows staff to achieve, sustain and develop creatively a high quality of practice through means of focused support and development. To provide a life-long learning experience that should continue throughout their employment at SWYPFT and beyond. 2.4 The aims of safeguarding children supervision are: 3. To enable and empower practitioners to develop knowledge and competence To provide a safe and structured environment for practitioners to reflect on, plan, review and account for their safeguarding children work. To provide support and recognition of the stress and uncertainties which safeguarding work may involve. ROLES AND RESPONSIBILITIES 3.1 Managerial Supervision 36 3.1.1 Responsibility of Line Managers (Supervisory Managers) The line manager will be responsible for monitoring that all types of supervision are taking place appropriately, in accordance with the standards in this document. 3.1.2 Responsibility of staff (Management supervision) Staff will ensure that they comply with attendance and use of managerial supervision sessions in accordance with the standards within this document. 3.2 Clinical Supervision 3.2.1 Responsibility of Managers Should ensure staff have dedicated time available to attend clinical supervision in line with this framework, as stated in para. 4.2.9. Should ensure staff comply with attendance at clinical supervision, monitoring attendance via staff performance review 3.2.2 Responsibility of Clinical supervisors It is the responsibility of the clinical supervisor: to initiate and lead development of the clinical supervision agreement. to be available to the supervisee during the sessions and be accountable for any advice they offer. 3.2.3 Responsibilities of the Supervisee It is the responsibility of the supervisee: to protect time and space for clinical supervision, by keeping agreed appointments and time boundaries. to prepare for the supervision in advance to bring material to the session and consider priorities to be honest, open and engage in reflective practice to be open to change and development 3.3 Safeguarding Children Supervision 3.3.1 Responsibility of Managers Should ensure that the safeguarding children dept are aware of new staff joining the service who will require safeguarding children supervision. 37 Should arrange with the new staff and the safeguarding children dept an induction within the first month of employment. Should ensure that staff have dedicated time available to attend safeguarding children supervision in accordance with this framework. 3.3.2 Responsibility of Supervisors Ensure that within the first month following appointment staff receive an induction with their safeguarding children supervisor, and are made aware of the supervision process and paperwork, including how to arrange supervision. At this induction the safeguarding children supervision contract will be completed and signed (Appendix E ) Provide information about the philosophy, aims and structure of supervision Be available to staff for supervision and share responsibility for arranging sessions Review the records for the families discussed, signing them to confirm supervision has taken place, and discussing how recording can be enhanced Agree and sign the supervision record for each family discussed Complete / update the supervisee development plan at each session Bring any factors which prevent or hinder staff from accessing supervision to the attention of service managers 3.3.3 Responsibility of staff (supervisee) Share responsibility for arranging supervision sessions Ensure dedicated time is set aside free from interruptions for the duration of the session Prepare for the session by completing the supervision record for each family to be discussed (Appendix E ) Agree and sign both the supervision record for each family and the Development Plan (Appendix E ) Bring any factors which result in the staff member being unable to attend supervision sessions to the attention of their service managers 4 STANDARDS FOR PRACTICE 4.1 Management supervision 4.1.1 Standard MS1 – During induction in the first 4 weeks, staff will be allocated a line manager who will provide their management supervision. Management supervision is carried out by the person/role indicated on the job description. It is hierarchical in nature and the agenda is dictated by the supervisory manager. It is compulsory as part of terms and conditions of employment. 38 4.1.2 Standard MS2 – Line Managers for management supervision purposes will be at band 6 and above or Senior Social Workers. It is within management supervision that any concerns or issues around work load and capacity, relationships within the team, development needs and attendance at mandatory or other training events, sickness and absence or a person’s performance at work may be addressed. A band 5 Nurse may undertake management supervision of junior staff where this is identified as development in terms of their CPD within the SDR process. They will carry out this work under the supervision of a band 6 Nurse. NB. Some professions, e.g. social workers, combine both management and clinical supervision within one supervision session (This hybrid-type of supervision is not recommended practice as it leads to confusion with regards to the focus of the session, dominance of the supervisors agenda and a lack of clarity with regards of ownership of any documentation that is produced within the session ultimately impacting on the quality of clinical supervision received). 4.1.3 Access to Management Supervision Standard MS3 – All clinical staff should receive management supervision to the frequency described in this framework. Standard MS4 – Management supervision is arranged at the discretion of the supervising manager. Management supervision should be undertaken as a minimum for one hour four times per year, in addition to the staff members SDR. Where there are additional needs meetings may be held more frequently at the discretion of the manager. Staff can access their manager on a needs basis in-between their set meetings. 4.1.4 Standard MS5 – Documentation of management supervision sessions must be maintained in line with The Trust’s Standards for Record-Keeping. Standard MS6 – Documentation of management supervision sessions remain the property of SWYPFT. Documentation/Record Keeping in Management Supervision A record of management supervision must be kept by the supervisory manager. 39 Records of issues raised in management supervision sessions and any actions arising from these, should be detailed by the supervisory manager – it is considered good practice to request counter signature of the record with these records remaining the property of SWYPFT. These records, where appropriate, should meet the Trust’s record keeping standards, e.g. be legible, in black ink, and be held securely to maintain confidentiality; note, they may be called upon as management evidence during disciplinary proceedings. A copy of the record may be offered to the person under supervision at the discretion of the supervisory manager. In line with the finding in the Norris Report (2010) line managers should consider whether information collected as part of management supervision should be entered into the particular staff members personal file, advice from Personnel Dept should be sought with regards to this. Supervisory managers may choose to keep their records in varied formats – however, an example can be found at appendix 3. Supervisory management records should be retained for the period that the staff member is employed by NHS Barnsley CSD and held securely by the supervisory manager. Where staff members leave our service, advice should be sought from Personnel Dept with regards to approval to destroy these records. Records should be destroyed via the destruction of confidential material process. 4.1.5 Standard MS7 – The environment chosen for management supervision must be conducive to facilitating an appropriate level of confidentiality during the session. Choice of venue is at the discretion of the line manager. Consideration must be given to the level of confidentiality the venue can provide, particularly in terms of sensitive information being overheard by third parties. 4.2 Clinical Supervision 4.2.1 Standard CS1 – Staff will choose their own clinical supervisor unless there are the exceptions detailed with this guidance. Clinical supervision is carried out by the staff member’s supervisor of choice. Clinical supervisors should not be selected for staff by line managers – except as a recommendation following a disciplinary hearing. 40 4.2.2 Standard CS2 – Staff members who carry out clinical supervision will undertake the Trust’s Clinical Supervisor Training or equivalent. Clinical supervisors must undertake clinical supervisor training to prepare them for the role, in order to be supported to undertake the training they must be seen as credible clinicians by their peers to ensure that clinical supervision is a meaningful positive process. Clinical supervisors who are external to SWYPFT should within their supervision agreement acknowledge the boundaries of their knowledge of SWYPFT policies and procedures and how this is to be managed 4.2.3 Standard CS3 – All clinical supervisors must undertake their own clinical supervision. Clinical supervisors must have their own regular clinical supervision where they can take their own clinical/developmental issues and any clinical/developmental issues arising from their supervision practice. 4.2.4 Standard CS4 – Staff will be able to choose the mode of supervision that meets their professional needs. A mixed economy of modes of clinical supervision will be available, one to one, group, peer and expert within the Community Mental Health Business Unit and practitioners should choose the mode that best suits their professional needs. 4.2.5 Standard CS5 – The function of clinical supervision will follow Proctor’s Tripartite Model. It is recommended in the Trust’s clinical supervision training that the process of clinical supervision will be delivered through Proctor’s Tripartite model which asserts that formative, restorative and normative functions should receive equal consideration within sessions with no one function dominating the session. 4.2.6 Standard CS6 – Recovery values will be integrated into clinical supervision. Clinical supervision within the Community Mental Health Business Unit will facilitate the sharing of recovery values as described in the NHS Barnsley CSD ‘Policy for the implementation of the recovery model incorporating physical well-being’. 41 4.2.7 Standard CS7 – Evidence based practice will inform guidance delivered as part of clinical supervision. Clinical supervision will provide an opportunity to address the theorypractice gap (Rolfe 1996) by the sharing of evidence-based practice in relation to the clinical issues raised. 4.2.8 Standard CS8 – The underpinning theory used within the delivery of clinical supervision will reflect the underpinning theory recommended for the clinical work of the supervisee. The underpinning philosophy used during clinical supervision will vary dependent on the clinical work being undertaken, for example, for practitioners utilising CBT within their practice a CBT framework should be used, for practitioners utilising a PSI approach a stress-vulnerability (Zubin and Spring 1977) within the emerging best practice framework (NIMHE 2004) should be used. 4.2.9 Access to Clinical Supervision This table serves to identify the minimum standard of frequency and duration of supervision for the roles identified – where staff are working with high risk and complexity, supervision arrangements should be adjusted to meet their increased need. Job Role Clinical supervision frequency and duration Delivery Counsellor 60-90 minutes monthly By accredited clinical supervisor of their choice Nurse One hour - 12 times By trained clinical supervisor of per year their choice Nurse in Preceptorship year One hour – Monthly By named preceptor Non-medical prescriber 90 hours during training – negotiated needs thereafter By designated psychiatrist Occupational Therapist (OT) One hour - 12 times By trained clinical supervisor of per year their choice OT in Preceptorship year One hour - Monthly Physiotherapist One hour - 12 times By trained clinical supervisor of per year their choice By named preceptor 42 Job Role Clinical supervision frequency and duration Delivery Physiotherapist in Preceptorship year One hour – Monthly By named preceptor Psychologist Assistant/trainee 90 minutes - weekly By qualified Clinical Psychologist (Trainees may be supervised by course approved alternate) Psychologist Highly Specialised One hour - weekly By qualified psychology professional trained in clinical supervision Psychologist Principal One hour – fortnightly By qualified psychology professional trained in clinical supervision Psychologist /Psychotherapist Consultant 60-90 minutes monthly By senior psychology professional trained in clinical supervision Psychological Well-being Practitioner One hour weekly By qualified psychology professional Psychotherapy Trainee One hour per six hours client contact By qualified psychotherapist in same model CB Psychotherapist Trainee One hour weekly By qualified/accredited CB Psychotherapist (CBP) CBT Psychotherapist (IAPT) 1-2 hours monthly By Senior CBP Psychotherapist Senior One hour - monthly By qualified Psychotherapist accredited / experienced in supervision Social worker One hour - Monthly Combined management and clinical supervision carried out by named senior social worker/professional support manager 43 Job Role Clinical supervision frequency and duration Delivery Social Worker in preceptorship year 1.5 hour -2 weekly at for first 3 months, then one hour – monthly Combined management and clinical supervision carried out by registered social worker. Support worker One hour - 12 hours per year By trained clinical supervisor of their choice Students Refer to specific requirements for placement. Refer to specific requirements for placement 4.2.10 Standard CS10 – All clinical supervision relationships will have a clinical supervision agreement drawn up jointly with the supervisor and supervisee. Clinical Supervision Agreement All clinical supervision relationships will have a written agreement with a review date of not more than one year, which details boundaries in terms of: Confidentiality Availability of supervisor Frequency/duration of sessions Resources available Documentation Although the agreement is a joint responsibility, the responsibility for initiating and ensuring that an agreement is developed rests with the clinical supervisor. 4.2.11 Standard CS11 – The boundaries of confidentiality will be made explicit within the clinical supervision agreement. Confidentiality Boundaries around confidentiality should be made explicit as part of the agreement and both parties should be aware of the circumstances in which a breach of confidentiality will occur (where the supervisee is receiving clinical supervision following recommendations from a disciplinary hearing special attention needs to be given to this). 44 The maintenance of confidentiality within clinical supervision is fundamental to a high quality experience; therefore breaches of confidentiality must be based on protection from harm and where behaviour contravenes the practitioner’s code of conduct or the law. Supervisors must enter in the clinical supervision agreement that they may take some material from their supervision sessions to their own clinical supervisor. Where this happens they should reassure supervisees that they will not be identified by name and that their clinical supervisor has a duty of confidentiality. Supervisees must be informed that this is non-negotiable and is the main mechanism that assists in the maintenance and promotion of quality within clinical supervision. 4.2.12 Standard CS12 – Clinical supervision will be arranged around the availability of the clinical supervisor. Availability of supervisor Clinical supervision sessions are arranged around the availability of the clinical supervisor. The supervisee has no right to demand additional supervision from that which is arranged but may discuss any unforeseen supervision needs with their supervisor who will then determine if they have the appropriate capacity to meet the additional need. Dependent on profession the number of supervisees a supervisor engages varies, for example in nursing it is recommended that clinical supervisors aim to take on three supervisees, in social work it is recommended that supervisors aim to take six supervisees. Any increase or reduction in the recommendations should be negotiated with their line manager. 4.2.13 Standard CS9 – clinical staff will receive clinical supervision of the frequency and duration specified within table 4.2.9 in line with their professional background and job role. Frequency/duration of sessions The frequency and duration of sessions is to be agreed between the clinical supervisor and supervisee. Staff are expected under the SWYPFT supervision of the clinical workforce policy to access clinical supervision regularly with a minimum of 12 hours per year. When staff are negotiating the duration of sessions they should bear in mind the nature of the work undertaken in clinical supervision and ensure that adequate time is allowed to facilitate this. 45 When staff are negotiating the frequency of sessions they should bear in mind that there is some inter-relatedness between sessions in terms of feedback and review and ensure that frequency is planned to assist with this. 4.2.14 Standard CS13 – the environment for clinical supervision chosen must be conducive to facilitating the work carried out in clinical supervision. Resources Resources such as a quiet environment that is conducive to confidential and developmental work are a requirement in clinical supervision. Who is responsible for arranging this should be decided as part of the agreement. It is important that clinical supervision sessions are not interrupted by routine telephone calls – however, it is acknowledged that urgent calls by their nature would be allowed. 4.2.15 Standard CS14 – Documentation of clinical supervision must be maintained and be kept in line with the Trust’s Standards for Record-Keeping. Record Keeping All clinical staff must keep their own records of attendance at clinical supervision sessions as evidence that they are meeting their minimum requirements under the policy. For the purpose of evidencing clinical supervision sessions have taken place, when asked during SDRs, a pro forma signed by the supervisor showing the dates of attendance for clinical supervision can be found at appendix D. For documentation of the session the SWYPFT pro forma can be used – alternatively practitioners may have their own preferred pro forma which can be used. All sessions must be recorded and the SWYPFT record-keeping guidelines must be followed. Records of the sessions can be written by the supervisee or by both/either parties, each party requires a copy of the record and has a duty to keep these records in a secure place which affords them the consideration given to any other confidential record. Records of clinical supervision sessions should be retained by each party whilst they remain in clinical practice. Some consideration may need to be given to the potential of supervision records being subpoenaed from previous periods of employment i.e. that the person has left this organisation may not be the point at which records are destroyed. 46 The records are the property of the supervisor/supervisee and unless agreed differently in the clinical supervision agreement cannot be disclosed to a third party unless both are in agreement or where breaches of confidentiality are based on protection from harm and where behaviour contravenes the practitioners code of conduct or the law. Standards relating to Identification and Training of Supervisors 4.2.16 Standard CS15 – Practitioners who wish to become clinical supervisors must meet the selection criteria outlined in this framework. Standard CS16 – Clinical Supervisors must be able to show evidence of up-dating their practice in line with the CPD requirements of their profession. Standard CS17 – Those who have undertaken clinical supervision training will fulfil this role whilst working as a clinician with the Community Mental Health Business Unit. Standard CS18 – Clinical Supervisors who are subject to poor performance objectives will cease to work as clinical supervisors during this period and will be subsequently re-instated to the role on the recommendation of their clinical lead and team manager. Identification and training of clinical supervisors It is essential to the delivery of high quality clinical supervision that clinical supervisors have the knowledge, skills and qualities to carry out this role. All practitioners who express an interest in becoming a clinical supervisor should be assessed by their clinical/professional lead as having: Credible clinical practice Evidence of continuous professional development Qualities consistent with good quality supervision provision such as warmth, honesty, integrity, empathy, respect and the ability to be reflective. All practitioners who meet the above criteria and are supported by their clinical/professional lead must be supported by their line manager in order to access the Trust’s Clinical Supervisor training or equivalent. Supervisors who are subject to performance review should be advised by their manager that they must not carry out their clinical supervisor 47 role during this period. Re-instatement to this role should be considered on the recommendation of both the team manager and clinical lead The community mental health business unit has made a commitment to provide clinical supervisors with ongoing support in addition to their own individual clinical supervision throughout the time they carry out a clinical supervision role, by providing bi-monthly support and up-date sessions for clinical supervisors and by developing a resource file specifically for clinical supervisors. 4.3 Safeguarding Children Supervision 4.3.1 Standard SG1 Where any concerns are raised around child protection within clinical or managerial supervision, the supervisor must direct the practitioner to seek safeguarding children supervision. Safeguarding children supervision can be arranged by contacting the Safeguarding Unit. 4.3.2 Standards SG2 Safeguarding children supervisors must have attended the appropriate child protection supervision training 4.3.3 Standard SG3 Safeguarding children supervision will be undertaken in a 1:1 confidential environment. 4.3.4 Standards SG4 A supervision contract will be formulated between supervisor and supervisee at the induction session (or first session when changing supervisor) 4.3.5 Standard SG5 The supervisee will be responsible for the preparation of the issues to be discussed and complete relevant paperwork prior to the session . Due to the session length, it is likely that a maximum of 3 cases can be discussed at each session, supervisees with more cases that require supervision will need to book a further session. The supervisor, in collaboration with the supervisee will formulate a Safeguarding Children development plan, which will be brought to all sessions by the supervisee, and updated at each session. 48 4.3.6 Standard SG6 Boundaries of confidentiality will be respected and reflected in the supervision agreement. Supervision sessions are confidential to the supervisor and the supervisee, and issues arising may only be disclosed outside the session following discussion between the supervisor and supervisee. However both supervisor and supervisee will work within the professional code of conduct for their profession, and SWYPFT Employment Policies. The professional codes of conduct and the Employment Policies take precedence over the supervision agreements. Anonymised supervision records will be made available to the Designated Nurse safeguarding children for quality assurance purposes. Supervision will be undertaken within a framework of anti-oppressive and non-discriminatory practice. Both supervisor and supervisee will be expected to challenge practice that is outside of these frameworks. Safeguarding children and child protection are recognised as being stressful. Safeguarding children supervision will form a safe environment for supervisees to discuss their feelings 4.3.7 Standard SG7 All documentation identified under the responsibilities of supervisors and supervisees must be completed appropriately. This has been appendixed to this document at appendix E 5 AUDITING SUPERVISION STANDARDS 5.1 Audit of Management Supervision A baseline e-mail audit of management supervision activity will be undertaken – as part of this audit staff will be asked to identify their supervisory manager and the frequency of their supervision meetings. This will be repeated to measure compliance with the standards. 5.2 Audit of Clinical Supervision The auditing of the clinical supervision standards will be based on an audit programme rolling over three years: in year one the standards that are applicable to supervisees only will be audited, year two standards that are applicable to supervisors only will be audited in year three standards that are applicable to supervisees only will be audited 49 A further telephone audit of clinical supervisor’s activity will be carried out on a yearly basis to measure the extent of implementation of clinical supervision with the community mental health business unit 5.3 Audit of Safeguarding Children Supervision 5.3.1 The quality and effectiveness of safeguarding children supervision will be monitored as an ongoing exercise in the following ways: Qualitative audits of supervisee experience of safeguarding children supervision will be conducted within the first year following this protocol, and every 2 years. 6 5.3.2 Regular evaluation of the safeguarding children supervision Record for compliance and quality. 5.3.3 Safeguarding children supervision will be reported as part of the quarterly report for the Director of professions REFERENCES Barnsley Metropolitan Borough Council (BMBC) Adult Social Services Directorate (2009) Supervision Procedure Children’s Workforce Development Council (2007) Providing Effective Supervision Leeds. CWDC. Department of Health (2006) From values to action: The Chief Nursing Officer’s review of mental health nursing. London: COI Department of Health (2000) Framework for the Assessment of Children in Need and their Families London. The Stationery Office. DFES (2004) National Framework for Children, Young People and Maternity Services London. DFES HM Government, (2010) Working Together to Safeguard Children London. DCSF HMSO (2004) The Children Act. London. HMSO Lord Laming (2003) The Victoria Climbié Inquiry Report. London. The Stationery Office Lord Laming (2009) The Protection of Children in England London. The Stationery Office Morrison, Tony (2007) Staff Supervision in Social Care Brighton. Pavilion 50 NHS Barnsley Care Services Direct (CSD) (2009) Clinical/Professional Supervision Policy NHS Barnsley (2010) Safeguarding Children Supervision Policy. Slone, Graham (2006) Clinical Supervision in Mental Health Nursing Chichester: Wiley. YEGDICH, Tania (1999) Clinical Supervision and managerial supervision: some historical and conceptual considerations. Journal of Advanced Nursing 30 (5), 1195-1204. 7 8 REVIEW OF THIS DOCUMENT 7.1 The standards will be reviewed 3 years from the date of approval 7.2 Audit of supervision activity will contribute to the review. APPENDIX Examples of Record Keeping Paperwork :Appendix 1 Clinical supervision pro forma – see appendix D Appendix 2 – Safeguarding children supervision pro forma – see appendix E 51 Appendix 3 LINE MANAGEMENT SUPERVISION Name of Supervisee: Date: Name of Supervisor: Venue: Matters Arising Supervisee Personal Agenda Caseload/Workload/Clinical Issues Safeguarding/Risk Issues Anti oppressive/Anti discriminatory Practice (Equality & Diversity) Training (Mandatory/Non-mandatory) Management Issues/Feedback/Development Supervisee Signature: Supervisor Signature: Date and time of next session: 52 Appendix D – Clinical Supervision pro forma RECORD OF SUPERVISION Appendix D1 Name of Supervisee: Name of Supervisor: Date/Duration Type (Group or 1:1) Supervisor signature 53 Clinical Supervision Contract Appendix D2 SUPERVISEE NAME: DESIGNATION/AREA OF WORK: SUPERVISOR NAME: DESIGNATION/AREA OF WORK: 1. FREQUENCY OF CONTACT/MINIMUM HOURS REQUIREMENT 2. LENGTH OF SESSION 3. VENUE OR PERSON RESPONSIBLE FOR ARRANGING VENUE 4. RECORD KEEPING A record of the session must be documented – in keeping with the standards for healthcare records. Documentation will held securely – describe process, 54 5. CONFIDENTIALITY All information disclosed in the clinical supervision session will be kept confidential with the following exceptions: Where harm to self or others is disclosed. Where unsafe, unethical or illegal practice is disclosed that the supervisee is unwilling to go through appropriate procedures/channels to address. To maintain high quality clinical supervision the supervisee has to agree to allow the supervisor to take any issues they feel appropriate from the session forward to their own clinical supervision, however the supervisor agrees to disclose the minimum of information necessary. Where supervisees choose to integrate their supervision records within their CDP portfolio, any record should avoid personal identification of service users or third parties, as service users may be able to apply for access to such records under the Data Protection Act. 6. REVIEW PROCESS 7. PROCEDURE FOR RESOLVING CONFLICT/ISSUE OF DIFFERENCE 8. CANCELLATION/RE-ARRANGEMENT PROCEDURE SIGNATURES DATE 55 REVIEW DATE: SUPERVISION RECORD 1:1 Appendix D3 SUPERVISEE: SUPERVISOR: DATE: KEY ISSUES BROUGHT: COMMENTS/REFLECTIONS: OUTCOMES/PLAN: SIGNATURES: DATE: 56 SUPERVISION RECORD: GROUP Appendix D4 SUPERVISOR NAME (PRINT): DATE: SIGNATURE: SUPERVISEES NAMES (PRINT): 1. 2. 3. 4. 5. 6. 7. 8. DURATION: SUPERVISEE SIGNATURES: KEY ISSUES BROUGHT: COMMENTS/REFLECTION: OUTCOMES/PLAN: 57 Appendix E – Safeguarding Children Supervision pro forma Appendix E1 Contract for Safeguarding Children Supervision Name of Supervisee – Name of Supervisor – Frequency / Duration of Supervision Sessions – Minimum of 3 monthly for minimum of 1 hour. The supervisor will: Encourage the utilisation of reflection to facilitate the supervisee’s critical analysis of practice. Create a forum which facilitates the supervisee to explore values, assumptions and attitudes in relation to practice. Provide professional support. Constructively challenge elements of practice where required. Ensure that the supervisee remains focused on the child and where required considers the needs of other children in the family. Promote effective interagency working and information sharing. Ensure that Local Safeguarding Children Board policies and procedures are adhered to. Agree any actions required and identify timescales for their implementation with the supervisee. The supervisee will: Identify families of concern for discussion within the supervision framework. Present case files for children and families discussed within supervision where practically possible Utilise reflection to facilitate professional development. Maintain professional accountability and responsibility for their actions. It is the responsibility of the supervisee to record within the clinical record that they have accessed safeguarding children supervision and any actions arising from this. N.B. Personal issues discussed within the context of supervision will remain confidential unless it becomes clear that withholding information may place a child/young person/adult or family at risk. Contract agreed Supervisee ……………………………………….. Date …………………………. Supervisor ……………………………………….. Date ………………………….. 58 Appendix E2 1:1 Safeguarding Children Supervision Record and Action Plan Action Plan Date Supervisee’s Name Supervisor’s Name Review of issues/actions discussed at last session (if applicable): Issues/children discussed at today’s session: 59 Action agreed for each issue or child Date of Next Meeting: Signed (Supervisee) Signed (Supervisor) Cc Supervisee Supervision File 60 Appendix E3 Safeguarding Supervision Contact Sheet/Record of Supervision Name: ……………………………………………………………………………………… Date Notes Signature 61 Date Notes Signature 62 Appendix F Minimum Learning outcomes for Clinical Supervision Training On completion of the training the learner will: have knowledge of the context within which supervision is provided and an understanding of the inherent responsibility. understand the importance of modelling the professional role. have knowledge of developmental models of learning which may have an impact on supervision. have an awareness of a number of supervision frameworks. will understand how the SWYPFT policy on clinical supervision impacts on practice. understand the importance of a safe environment in facilitating learning and the factors that affect the development of a supervisory relationship. have an awareness of contracting and negotiating with supervisees and the importance of maintaining documentation.. have an understanding of the transferability of professional skills into supervision. have an understanding of constructive criticism and ongoing positive feedback. will understand the role of reflective practice in clinical supervision. The learner will understand the need for undertaking ongoing clinical supervision in their development as a clinical supervisor. 63 Appendix G - Checklist for the Review and Approval of Procedural Document To be completed and attached to any policy document when submitted to EMT for consideration and approval. Title of document being reviewed: 1. 2. 4. 5. 6. Comments Title Is the title clear and unambiguous? YES Is it clear whether the document is a guideline, policy, protocol or standard? YES Is it clear in the introduction whether this document replaces or supersedes a previous document? YES Rationale Are reasons for development of the document stated? 3. Yes/No/ Unsure YES Development Process Is the method described in brief? YES Are people involved in the development identified? YES Do you feel a reasonable attempt has been made to ensure relevant expertise has been used? YES Is there evidence of consultation with stakeholders and users? YES Content Is the objective of the document clear? YES Is the target population clear and unambiguous? YES Are the intended outcomes described? YES Are the statements clear and unambiguous? YES Evidence Base Is the type of evidence to support the document identified explicitly? YES Are key references cited? YES Are the references cited in full? YES Are supporting documents referenced? YES Approval Does the document identify which committee/group will approve it? YES If appropriate have the joint Human 64 Title of document being reviewed: Yes/No/ Unsure Comments Resources/staff side committee (or equivalent) approved the document? 7. 8. 9. 10. 11. Dissemination and Implementation Is there an outline/plan to identify how this will be done? YES Does the plan include the necessary training/support to ensure compliance? YES Document Control Does the document identify where it will be held? YES Have archiving arrangements for superseded documents been addressed? YES Process to Monitor Compliance and Effectiveness Are there measurable standards or KPIs to support the monitoring of compliance with and effectiveness of the document? YES Is there a plan to review or audit compliance with the document? YES Review Date Is the review date identified? YES Is the frequency of review identified? If so is it acceptable? YES Overall Responsibility for the Document Is it clear who will be responsible implementation and review of the document? YES 65 Appendix H Version Control Sheet This sheet should provide a history of previous versions of the policy and changes made Version Date Author Status Comment / changes March 2009 May 2010 Marie Knott Final Final versions approved by SWYPFT and NHS Barnsley Trust Boards Supervision Policy Group Final 1 July 2012 Alison Hill Lead Nurse Community Mental Health/ Clinical Supervisor Training Facilitator Draft SMYPFT Supervision policy for clinical staff and NHS Barnsley Clinical/professional supervision policy aligned. 1 August 2012 Alison Hill Lead Nurse Community Mental Health/ Clinical Supervisor Training Facilitator Draft First draft sent out for consultation: Tim Breedon, Dr Adrian Berry, Anna Basford, Ann Hargate, George Smith, Julie Fleetwood, Karen Batty, Anne Hoyle, Simon Plummer, Dr Nisreen Booya, Julie Hickling, Sean McDaid, Richard Clibbens, John Cordall, Caroline Rake, Tonia Devenport, Sheila Lewis, Professor Nigel Beail, Carol Bishop, Carol Circuit, Diane Collinson, Di Dillon, Ruth Donnoghue, Sue Dymock, Janet foster, Helen Dixon, Sarah Hudson, Kyra Ayre, Anita McCrum, Deborah McLeaod, Ann Meynell, Hiliary Mosley, Janet Owen, Kathryn Padgett, Sandra Montisci, Bob Senior, Simon Robinson, Julie Smith, Andrew Stones, Jill Thicket, Alison Thomas, Dawn Thomas, Linda Wake, Helen Walker, Sean Rayner, Sue Wing, Dave Ramsay, Andrea Wilson, Jeremy Robbins, Dr Keith Sands, Dr Suresh Chari, Clinical Supervisors Up-date and Support Session (Barnsley Mental Health) Staff side: Paul Smith, David Pickersgill HR: Hilary Bannister, Kate Redican, David Batty, Marilyn Gill, Janet Hirst 2 Sept 2012 Alison Hill Lead Nurse Community Mental Health/ Clinical Supervisor Training Facilitator First draft reviewed and amended following feedback from: Prof. Nigel Beail, Ann Hargate, Sarah Hudson, Sharon Kehoe, Julie WarrenSykes, Jeremy Robbins, Andrea Wilson, Julie Smith, Anne Hoyle, Dawn Thomas, David Ramsay, George Smith, Christine Harrison, John Cordall, Dr Lisa Winter, Simon Plummer, Dr Delyth James, Julie Hickling 66 67