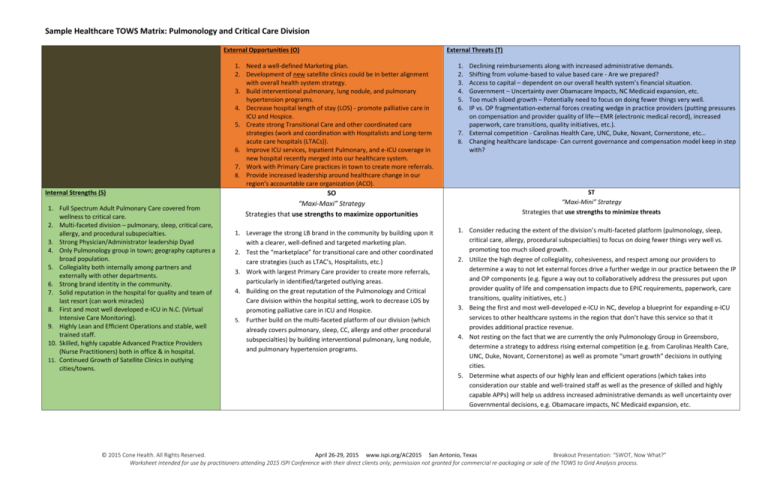
Sample Healthcare TOWS Matrix: Pulmonology and Critical Care Division
External Opportunities (O)
1. Need a well-defined Marketing plan.
2. Development of new satellite clinics could be in better alignment
with overall health system strategy.
3. Build interventional pulmonary, lung nodule, and pulmonary
hypertension programs.
4. Decrease hospital length of stay (LOS) - promote palliative care in
ICU and Hospice.
5. Create strong Transitional Care and other coordinated care
strategies (work and coordination with Hospitalists and Long-term
acute care hospitals (LTACs)).
6. Improve ICU services, Inpatient Pulmonary, and e-ICU coverage in
new hospital recently merged into our healthcare system.
7. Work with Primary Care practices in town to create more referrals.
8. Provide increased leadership around healthcare change in our
region’s accountable care organization (ACO).
Internal Strengths (S)
1. Full Spectrum Adult Pulmonary Care covered from
wellness to critical care.
2. Multi-faceted division – pulmonary, sleep, critical care,
allergy, and procedural subspecialties.
3. Strong Physician/Administrator leadership Dyad
4. Only Pulmonology group in town; geography captures a
broad population.
5. Collegiality both internally among partners and
externally with other departments.
6. Strong brand identity in the community.
7. Solid reputation in the hospital for quality and team of
last resort (can work miracles)
8. First and most well developed e-ICU in N.C. (Virtual
Intensive Care Monitoring).
9. Highly Lean and Efficient Operations and stable, well
trained staff.
10. Skilled, highly capable Advanced Practice Providers
(Nurse Practitioners) both in office & in hospital.
11. Continued Growth of Satellite Clinics in outlying
cities/towns.
SO
“Maxi-Maxi” Strategy
Strategies that use strengths to maximize opportunities
1. Leverage the strong LB brand in the community by building upon it
with a clearer, well-defined and targeted marketing plan.
2. Test the “marketplace” for transitional care and other coordinated
care strategies (such as LTAC’s, Hospitalists, etc.)
3. Work with largest Primary Care provider to create more referrals,
particularly in identified/targeted outlying areas.
4. Building on the great reputation of the Pulmonology and Critical
Care division within the hospital setting, work to decrease LOS by
promoting palliative care in ICU and Hospice.
5. Further build on the multi-faceted platform of our division (which
already covers pulmonary, sleep, CC, allergy and other procedural
subspecialties) by building interventional pulmonary, lung nodule,
and pulmonary hypertension programs.
External Threats (T)
1.
2.
3.
4.
5.
6.
Declining reimbursements along with increased administrative demands.
Shifting from volume-based to value based care - Are we prepared?
Access to capital – dependent on our overall health system’s financial situation.
Government – Uncertainty over Obamacare Impacts, NC Medicaid expansion, etc.
Too much siloed growth – Potentially need to focus on doing fewer things very well.
IP vs. OP fragmentation-external forces creating wedge in practice providers (putting pressures
on compensation and provider quality of life—EMR (electronic medical record), increased
paperwork, care transitions, quality initiatives, etc.).
7. External competition - Carolinas Health Care, UNC, Duke, Novant, Cornerstone, etc…
8. Changing healthcare landscape- Can current governance and compensation model keep in step
with?
ST
“Maxi-Mini” Strategy
Strategies that use strengths to minimize threats
1. Consider reducing the extent of the division’s multi-faceted platform (pulmonology, sleep,
critical care, allergy, procedural subspecialties) to focus on doing fewer things very well vs.
promoting too much siloed growth.
2. Utilize the high degree of collegiality, cohesiveness, and respect among our providers to
determine a way to not let external forces drive a further wedge in our practice between the IP
and OP components (e.g. figure a way out to collaboratively address the pressures put upon
provider quality of life and compensation impacts due to EPIC requirements, paperwork, care
transitions, quality initiatives, etc.)
3. Being the first and most well-developed e-ICU in NC, develop a blueprint for expanding e-ICU
services to other healthcare systems in the region that don’t have this service so that it
provides additional practice revenue.
4. Not resting on the fact that we are currently the only Pulmonology Group in Greensboro,
determine a strategy to address rising external competition (e.g. from Carolinas Health Care,
UNC, Duke, Novant, Cornerstone) as well as promote “smart growth” decisions in outlying
cities.
5. Determine what aspects of our highly lean and efficient operations (which takes into
consideration our stable and well-trained staff as well as the presence of skilled and highly
capable APPs) will help us address increased administrative demands as well uncertainty over
Governmental decisions, e.g. Obamacare impacts, NC Medicaid expansion, etc.
© 2015 Cone Health. All Rights Reserved.
April 26-29, 2015 www.ispi.org/AC2015 San Antonio, Texas
Breakout Presentation: “SWOT, Now What?”
Worksheet intended for use by practitioners attending 2015 ISPI Conference with their direct clients only; permission not granted for commercial re-packaging or sale of the TOWS to Grid Analysis process.
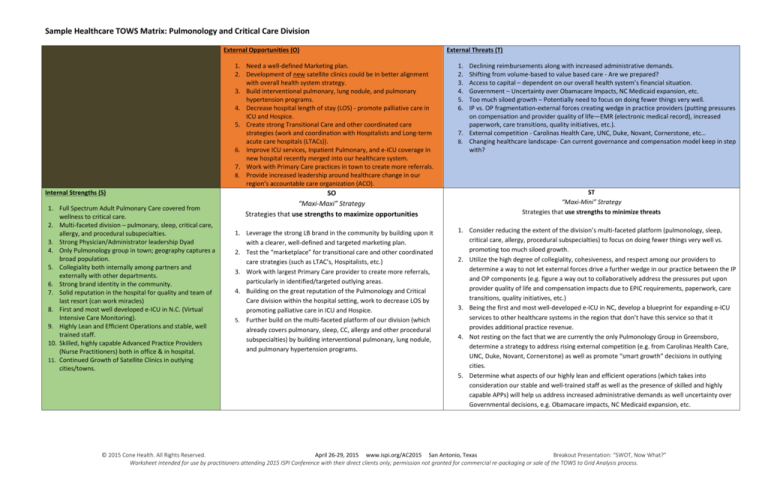
Internal Weaknesses (W)
1. Handoff of medical care: ill-defined transitional care
strategies.
2. Specific Physician Performance/Behavior Issues
affecting Employee Engagement and Patient
Satisfaction.
3. As we grow differing sub-specialties, becoming more
siloed.
4. Established/set referral patterns in the community not
completely in our favor.
5. Being multi-faceted requires manual, complex
scheduling of provider time (office, e-ICU, hospital, call,
etc.).
6. Need for greater standardization of documentation and
protocols.
7. Need for cohesive succession planning (retiring
providers, Division Leadership elections, etc…)
8. Expand sleep medicine practice- specifically home sleep
studies.
9. Continuation Plan for Allergy Lab once doctor in charge
retires.
10. Expand into other areas of Pulmonary Subspecialties
(Occupational Health, Chronic Obstructive Pulmonary
Disease, Pulmonary Hypertension, Asthma, etc…).
WO
“Mini-Maxi” Strategy
Strategies that minimize weaknesses by taking advantage of
opportunities
1. Minimize ill-defined transitional care strategies by investigating
possibilities around coordinated care strategies with CH, Hospitalists,
and LTAC’s.
2. Reduce inpatient vs. outpatient conflicts by providing intentional,
increased leadership around setting proper expectations of physician
behavior and respectful rules of engagement.
3. Disrupt disadvantageous set referral patterns established in the
community by working intentionally with largest Primary Care
provider to create more referrals.
4. Establish a well-defined succession plan (that address retiring
providers, Division leadership, etc.) by intentionally developing the
leadership potential within the division.
5. In the creation of a well-defined marketing plan, give special
consideration to promoting/highlighting the offering of expanded
sleep medicine services (e.g. home sleep studies).
6. Identify targeted successor(s) from the pipeline of leadership
potential within the division to enable the continuation of the
Allergy Lab.
7. Use NP team’s skillsets innovatively by determining ways to
integrate them intentionally into transitional care and other
coordinated care strategies (CH, Hospitalists, and LTAC’s).
WT
“Mini-Mini” Strategy
Strategies that minimize weaknesses and avoid threats
1. Stop the perpetuation of siloed growth by reducing the intentional development of more
differing sub-specialties.
2. Address the forces creating a wedge in the practice from an IP and OP fragmentation
standpoint (such as compensation and provider quality of life issues due to EPIC, paperwork,
care transitions, quality initiatives, etc.) by starting first to reconcile philosophies and establish
standards of behaviors for respective providers in each of the groups.
3. Determine way to build on solid reputation as only pulmonary group in the area in order to
offset encroaching external competition (CHS, UNC, Duke, Novant, Cornerstone).
4. Determine methods for our division to proactively address governance and compensation
model issues and concerns, particularly in light of the changing healthcare landscape.
5. Determine strategies to address Governmental uncertainty related to Obamacare impacts, NC
Medicaid expansion, etc.
© 2015 Cone Health. All Rights Reserved.
April 26-29, 2015 www.ispi.org/AC2015 San Antonio, Texas
Breakout Presentation: “SWOT, Now What?”
Worksheet intended for use by practitioners attending 2015 ISPI Conference with their direct clients only; permission not granted for commercial re-packaging or sale of the TOWS to Grid Analysis process.