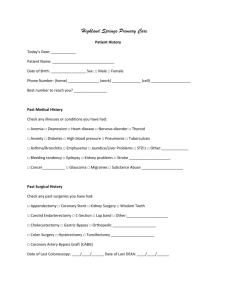
New Patient Questionnaire (General)
advertisement

Pediatric Surgical Services, Inc. New Patient Medical History Questionnaire To assist us in caring for your child, please complete the following questionnaire Why are you here today? What has been done thus far for this problem? (i.e. lab tests, X-rays, ultrasounds, MRT, CT, VCUG, medications) HISTORY OF PATIENT'S BIRTH Ended early, @ ________________ Full Term wks. Gestation Vaginal Scheduled C-section No Yes Please explain: No Yes What? Mother's pregnancy with patient was: Delivery was: Complicated pregnancy or delivery? Medications taken while pregnant? Hospitalizations Surgeries Blood Transfusions Contagious Disease Psychological Care Is child still receiving psychological care? No No No Yes Yes Yes When? When? When? No No Yes Yes What? When? No Yes By whom? Emergency C-Section PAST MEDICAL HISTORY Where? Why? Where? Why? Where? Where? Where? Why? CHILDS FAMILY HISTORY Have any blood-related patient, sibling, grandparent, aunt, uncle or cousin of the patient had problems concerning: Anesthetic Asthma Bleeding Cancer Developmental delays Diabetes Heart Disease Liver or kidney disease Seizures Tuberculosis Bedwetting Other No No No No Yes Yes Yes Yes Who? Who? Who? Who? Deceased? Deceased? Deceased? Deceased? No No No No Yes Yes Yes Yes Age: Age: Age: Age: No No No Yes Yes Yes Who? Who? Who? Deceased? Deceased? Deceased? No No No Yes Yes Yes Age: Age: Age: No No No No Yes Yes Yes Yes Who? Who? Who? Who? Deceased? Deceased? Deceased? Deceased? No No No No Yes Yes Yes Yes Age: Age: Age: Age: SOCIAL HISTORY Patient's parents are: Who does patient live with? Attends school? Other Rev. 5/07 Married Unmarried No Yes Divorced Grade: Separated Widowed (one parent is deceased) School: New Patient Medical History Questionnaire Page 1 of 2 CURRENT MEDICATIONS Homeopathic or Natural Remedies/vits 1. 2. 3. 4. Medication and dose 1. 2. 3. 4. REVIEW OF SYSTEMS Has the patient had any problems with: HEENT (head/eyes/ears/throat) Headaches Eyes Ears Nose Swollen glands Sinus problems Pulmonary (lungs) Asthma/Wheezing Persistent Cough Shortness of Breath Cardiac (heart) Heart defect(s) Skin turning blue Heart murmur(s) Palpitations GI (digestive system) Stomach Constipation Diarrhea Nausea/Vomiting Allergies Endocrine (hormonal system) Excessive appetite Excessive thirst No No No No No No Yes Yes Yes Yes Yes Yes No No No No No No No No Yes Yes Yes Yes Yes Yes Yes Yes No No No No Yes Yes Yes Yes No Yes Musculoskeletal (muscle and bone) Muscles Bones Arms Legs Hips Back Feet Hematologic/Lymph (blood) Clotting problems Bleeding problems Bruising easily Neurologic (nervous system) Head Injury Seizures Psychological Depression Anxiety/nervousness Sleep disorder Integumentary Poor wound healing Rashes To what? No No Yes Yes Weight problem Cold/heat intolerance ______________________________________ _____________________ Provider Signature Date Date Reviewed Prov. Initials Date Reviewed Prov. Initials Date Reviewed Prov. Initials Date Reviewed Prov. Initials Note: Changes to ROS, medical, family and social history is documented in progress note. Rev. 5/07 New Patient Medical History Questionnaire Page 2 of 2 No No No No No No No Yes Yes Yes Yes Yes Yes Yes No No No Yes Yes Yes No No No No No No No No Yes Yes Yes Yes Yes Yes Yes Yes No No Yes Yes