INTERNAL MEDICINE RESIDENCY PROGRAM – RWJMS
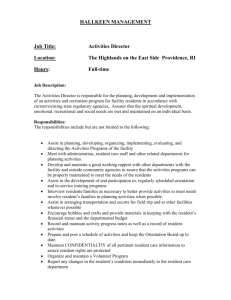
advertisement

POLICY MANUAL 2012-2013 INTERNAL MEDICINE RESIDENCY PROGRAM INDEX CALL COVERAGE COMMUNICATION COMMUNITY SERVICE CONTINUITY CLINIC DAILY CONFERENCE ATTENDANCE DRESS CODE DUE PROCESS DUTY HOURS ELECTIVES EVALUATION FLOAT AND PERSONAL DAYS HOUSESTAFF SELECTION HOUSESTAFF SUPERVISION LEAVE OF ABSENCE MEDICAL DOCUMENTATION MEDICAL RECORDS COMPLETION – RWJUH MEDICAL RECORDS COMPLETION – UMCP MOONLIGHTING NATIONAL CONFERENCES NON-TEACHING PATIENT COVERAGE ORDER WRITING PERFORMANCE DEFICIENCES PHARMACEUTICAL INDUSTRY PINCH HITTER USAGE PROCEDURES PROMOTIONS RECOMMENDATION LETTERS RESEARCH SCHEDULING REQUESTS SERVICES – RWJUH SERVICES – UMCP SICK DAYS SUBSPECIALTY FELLOW AND INTERNAL MEDICINE RESIDENT INTERACTION TEACHING SERVICE RESPONSIBILITIES FOR MEDICAL INTENSIVE CARE UNIT SERVICE (ICU) AT RWJUH AND UMCP TEACHING SERVICE RESPONSIBILITIES FOR MEDICAL TEACHING SERVICE (MTS), CARDIOLOGY TEACHING SERVICE (CTS), ONCOLOGY TEACHING SERVICE (OTS), NIGHT FLOAT AND BACK-UP AT RWJUH AND UMCP TRANSITIONS OF CARE TRAVEL POLICY UMDNJ POLICY MANUAL UNIVERSITY HOLIDAYS VACATIONS 2 of 92 Compliance with all UMDNJ policies is required. The UMDNJ policy manual can be reviewed at the following site: http://www.umdnj.edu/oppmweb/Policies/contents.html 3 of 92 Policy Name: Dress Code Policy Policy Number: 1 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: To ensure that residents appear professional at all times. Policy: All house staff must wear a clean white coat at all times. Men - must wear a shirt and tie with slacks, even on weekends. Women - must be neat and professional at all times. Jeans, tee shirts, open-toed shoes, etc. are not acceptable attire. Scrubs may only be worn during Night Float and during overnight ICU or overnight floor call. 4 of 92 Policy Name: Work Hour Policy Policy Number: 2 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: To ensure that residents are well rested and able to provide safe, effective patient care while maintaining compliance with the ACGME work hour rules. Policy: The work week for each resident will be restricted to a maximum of 80 hrs/week when averaged over 4 weeks. This includes residency activities and moonlighting hours irrespective of the site or type of assignment. Random duty hour audits will be conducted and necessary adjustments made to ensure full compliance. When averaged over a 4 week rotation, residents must have at least 1 day in 7 free of residency related activities. A day off is defined as one continuous 24 hour period free from all clinical, educational, and administrative duties. Each resident must have an 8 hour duty free period between all daily shifts and after in-house call. They must also have at least 14 hours free of duty after 24 hours of in-house duty. Continuous on-site duty, including in-house call, must not exceed 24 hours for PGY 2 and PGY 3 residents. No new patients may be accepted after 24 continuous hours on duty. Continuous on-site duty, including in-house call, must not exceed 16 hours for PGY 1 residents. In unusual circumstances, residents, on their own initiative, may remain beyond their scheduled period of duty to continue to provide care to a single patient. Justifications for such extensions of duty are limited to reasons of required continuity for a severely ill or unstable patient, academic importance of the events transpiring, or humanistic attention to the needs of a patient or family. Under those circumstances, the resident must: appropriately hand over the care of all other patients to the team responsible for their continuing care; and, document the reasons for remaining to care for the patient in question and submit that documentation in every circumstance to the program director. Residents will not be assigned to in-house overnight on call duty at a frequency greater than every fourth night. 5 of 92 Weekdays: Residents on elective are to be at Board Review at 7:00 am. Residents on service, if not at Board Review are required to be at sign in rounds in the residency call room at RWJUH or residency lounge at UMCP at 7:00am. Residents on elective may leave at 4:30pm or until all the work is done. Residents on service may sign out no earlier than 4:30pm. (unless post overnight call). Residents in clinic may not leave clinic until all the residents at that clinic site and day have seen all their patients, even if on call that day. Weekends/Holidays: Residents on elective are off, unless they are the pinch hitters for that period. Residents on service are required to be at sign in rounds in the residency call room at 8:00am. Residents on service may sign out no earlier than 12:00pm. 6 of 92 Policy Name: Non-Teaching Patient Coverage Policy Policy Number: 3 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: To ensure that residents’ service responsibilities are limited to patients for whom they have primary diagnostic and therapeutic responsibility, as per the ACGME regulation. Policy: 1. Residents will not respond to emergencies on non-teaching service patients unless it is a code situation. 2. Residents will not place any orders on non-teaching service patients. 3. Residents will only admit those patients that who will remain on the teaching services during their hospital admission. 7 of 92 Policy Name: Medical Documentation Policy Policy Number: 4 Approval by Program Leadership: 7/1/05 Amendment Date: 5/31/09 Purpose: To ensure safe patient care and efficient communication among healthcare providers. Policy: All resident progress notes, procedure notes and H&Ps must be dated, timed and signed by the resident, with name and pager number printed legibly under the signature. All H&Ps must be co-signed by a senior resident and an independent brief resident note must be included. All progress notes written by a medical student must be accompanied by a addendum from a resident or intern. H&Ps written by medical students will not be accepted as part of the medical record. All patient interactions, family meetings and evaluations in a cross-coverage situation should be clearly documented. All notes written by residents and placed in the medical record are legal documents and falsification of them is a criminal action. 8 of 92 Policy Name: Order Writing Policy Policy Number: 5 Approval by Program Leadership: 7/1/05 Amendment Date: 5/31/09 Purpose: To ensure safe patient care by providing a single point of contact for medical orders. Policy: In the non-emergency setting, residents must write all orders for patients under their care, with appropriate supervision by the attending physician. In an emergency setting, should an attending physician write an order on a resident’s patient, the attending must communicate his/her action to the resident or cross-covering resident in a timely manner. 9 of 92 Policy Name: Daily Conference Attendance Policy Policy Number: 6 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: To ensure that residents participate in the art, science, and business of medicine curriculum. Policy: A. Board Review: Board review is from 7:00am to 7:45am Monday – Friday from July – May. It is held in MEB 108B at RWJUH and in the classroom next to the noon report room in the 1st floor of Lambert House at UMCP. It is videoconferenced between the two sites. All PGY-2 & 3 on RWJ floor service and night float are encouraged to attend. All PGY-2 and PGY-3 residents on service on UMCP floor service are encouraged to attend. PGY-2 & 3 residents on night float at UMCP are REQUIRED to attend. All PGY-1, 2 & 3 residents ON ELECTIVE are REQUIRED to attend and MUST attend at their elective site. Ideally, a resident should not miss board review unless there are extenuating circumstances. If extenuating circumstances occur, a resident may not miss more than two board review sessions during a two week elective block or four board review sessions during a four week elective block. These include days missed for personal days, sick days, and interview days. Hospitalizations will not be counted. Interview days in excess of the time allotted need to be approved by the chief resident. Absences from board review in excess of the above will result in the resident being placed on Academic Warning/Probation as outlined in Policy #25. Additional offenses after the resident has been placed on Academic Warning/Probation may result in dismissal proceedings. B. Night Float Rounds: At RWJUH, night float rounds will be held daily from 7:45 to 8:30am except on holidays, weekends, and days of Grand Rounds conferences. The attending will meet the team by MEB 108B. At UMCP, night float rounds will be held daily from 8:00 to 8:30am except on holidays, weekends, and days of Grand Rounds conferences. The 10 of 92 senior night float resident will contact the attending to find out where they will meet. C. Conference: EVERY resident is responsible for attending all conferences while on floor service or in-house elective listed below and in case of conflict, please contact the chief resident directly. Those residents on the oncology service are encouraged to attend noon conference based upon census but are required to attend Grand Rounds. Every resident may be assigned to give Journal Club, CPC and/or M&M conference during the year. All Journal Club articles must be approved by the chief residents. 1. RWJUH: Monday through Friday in MEB 108B unless otherwise stated. Please follow times based on the monthly schedule for conferences. a) Noon Report: Daily starting at noon. b) Core Conference: Multiple times a week following Noon Report and includes Journal Club. c) Grand Rounds: Wednesdays from September - June in CAB 1302 from 8:00am to 9:00am. d) Art of Medicine and Business of Medicine Conferences: Occurring alternating months in MEB Room 108B, time to be determined. e) M&M: Occurring the last week of every month where each service team presents 2. UMCP: a) Noon Report: Monday, Wednesday, Thursday, and Friday in Class Room #3 Lambert-1st floor at noon. b) Grand Rounds: Tuesdays from September - June in Ground Floor Conference Room A from 8:00am to 9:00am. c) Art of Medicine and Business of Medicine Conferences: Occurring alternating months, time to be determined. See monthly schedules 11 of 92 d) Core Conference: Multiple times a week following noon report. See monthly schedules. e) M&M: Occurring the last week of every month where each service team presents appropriate cases D. Clinic Conference: Residents will be assigned topics within the Outpatient Johns Hopkins Internal Medicine Curriculum. Residents should review their assigned topic prior to clinic and be prepared to moderate the discussion with supervision by the clinic preceptor. E. Failure to present a CPC/M&M/Journal club or any other scholarly activity: If a resident is not prepared to present at conference, he/she will have to present that conference at a later date. In addition, an extra conference presentation will be assigned along with a written formal explanation regarding the event. 12 of 92 Policy Name: Housestaff Selection Policy Policy Number: 7 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: This policy ensures that the residency program selects the best qualified individuals without discrimination. Policy: Applicants are selected based on their preparedness, abilities, aptitude, academic credentials, communication skills, and personal qualities such as motivation and integrity. The program does not discriminate with regard to gender, race, age, religion, color, national origin, disability, or veteran status. The selection protocol for all applicants involves review and verification of the application with supporting documents and a formal interview process. When applying for a PGY II or PGY III position, a letter of reference from the applicant’s former program director will be required. For admission to the PGY III year of training, the applicant must have passed USMLE step 3, NBMOE Part III or COMLEX Level III. In addition, all applicants must fulfill criteria for registration, permits, or licensure with the New Jersey Board of Medical Examiners Review the UMDNJ-Robert Wood Johnson Medical School Graduate Medical Education Policy Manual, policy number I.1, for further details. 13 of 92 Policy Name: Promotions Policy Policy Number: 8 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: To establish minimum proficiency criteria for advancement to the next level of training as determined by the Residency Promotions Committee. Policy: 1. Proficiency Criteria for Determination of Advancement in Training Advancement to PGY2 Level of Training: Medical 1. Demonstrate knowledge needed to obtain a comprehensive history Knowledge and perform a physical exam, interpret basic laboratory studies, and generate a differential diagnosis. 2. Demonstrate knowledge and application of the basic pathophysiology and natural history of those diseases encountered in caring for one’s patients. 3. Demonstrate knowledge of inpatient clinical parameters for patients under one’s care, including generation of a diagnosis, the clinical course and an updated problem list. Patient Care 1. Demonstrate the skills needed to perform a comprehensive history and physical exam, interpret diagnostic studies, and generate a meaningful and timely patient care plan, including all orders. 2. Demonstrate the ability to synthesize, present and document (including medical records) the above in the form of a meaningful timely patient care plan. 3. Demonstrate the ability to recognize, assess and treat emergencies. 4. Demonstrate the ability to generate meaningful consultative requests while understanding the relationships of consultants to the primary care physician(s). 5. Perform procedures as indicated and with the necessary supervision. Maintain accurate logs and web-based entry of procedures performed as prescribed by the Procedural Committee of the Residency Program. Interpersonal & Demonstrate the ability to communicate effectively with patients, Communication families, colleagues, all members of the health care team and office staff Skills (residency, private office, and clinic). Professionalism 1. Demonstrate a high standard of personal honesty and integrity. 2. Exhibit humanistic qualities in caring for the patients. 3. Demonstrate active participation in working and teaching rounds. 4. Respond to administrative requests, pages, and email communication in a timely manner. 5. Accept reading and teaching assignments as prescribed by the senior 14 of 92 Systems Based Practice Practice Based Learning resident, attending, or chief residents. 6. Record >80% attendance at all academic conferences and board review with active participation. 7. Adherence to all program policies and requirements. 8. Demonstrate the ability to accept feedback related to any of the competencies and demonstrate change. 1. Demonstrate an awareness of team structure and function. 2. Demonstrate the ability to identify resources within the local healthcare delivery system with the sole aim of promoting patient care. 1. Demonstrate an interest and awareness in accessing resources needed to incorporate evidence into the clinical decision making arena. 2. Demonstrate enthusiastic participation in the outcomes project aimed at measuring and improving clinical parameters for select disease modules. Each of the above criteria in combination assess the ability of the intern to transition into their role as TEAM LEADER where necessary skills in medical knowledge, data gathering, clinical insight and critical thinking lend itself to effective leadership and role modeling. Residents should use the milestones file on the residency website as a guide to determine if they are meeting current requirements. 2. Proficiency Criteria for Determination of Advancement in Training Advancement to PGY3 Level of Training: In addition to meeting the junior level proficiency criteria, PGY-2s must demonstrate progression in the competencies as outlined below in order to advance. Residents should use the milestones file on the residency website as a guide to determine if they are meeting current requirements. Medical Knowledge Patient Care 1. Display further expansion of medical knowledge, including evidencebased guidelines, specific disease-based recommendation and refinement in history taking skills and physical exam signs using a selfdirected learning style. 2. Demonstrate evidence of outside reading. 1. Demonstrate the ability to construct, present and document a concise and relevant resident note with greater emphasis on the clinical assessment and care plan. 2. Accept responsibility and demonstrate familiarity with important clinical parameters for patients under one’s care and when supervising interns on other teams. 3. Demonstrate the ability of quick recognition, assessment and treatment of emergencies, including role as code leader. 4. Demonstrate the ability to recognize and manage “new” clinical problems, i.e. those scenarios not previously encountered. 5. Continue to perform procedures within one’s expertise while safely 15 of 92 supervising interns/students with their procedural skills. 6. Demonstrate the ability to coordinate care between different settings. Interpersonal & 1. Demonstrate the ability to communicate feedback in real time to Communication interns and students on their data gathering skills, clinical assessment, Skills care plans and documentation. 2. Demonstrate progressive development of communication skills in the arena of Bioethics and End of Life Care. 3. Demonstrate the ability to communicate effectively and directly with consultants from within and outside the specialty of internal medicine. Professionalism 1. Demonstrate a high standard of personal honesty and integrity. 2. While exhibiting humanistic qualities in caring for patients, function as a role model to other members of the healthcare team. 3. Demonstrate ability to lead rounds by selecting cases and scenarios for discussion, organizing structure and duration of rounds and helping each member attain their individual educational objectives. 4. Accept reading and teaching assignments as prescribed by attending physicians and chief residents. 5. Respond to administrative requests, pages and email communication in a timely manner. 6. Record >80% attendance at ALL academic conferences and board review with active participation. 7. Adherence to all program policies and requirements. 8. Demonstrate the ability to accept feedback related to any of the competencies and demonstrate change. Systems Based 1. Demonstrate effective leadership skills as team leader and patient Practice advocate in facilitating access to resources and care. 2. Demonstrate willingness to review and discuss all aspects of care, including individual and system related errors. 3. Demonstrate utilization of cost effective “best practices” in all aspects of patient care. Practice Based 1. Demonstrate proficiency in accessing resources and establishing Learning guidelines in the practice of evidence based medicine. 2. Demonstrates the ability to utilize the principles of evidence based medicine in the context of differing clinical scenarios. 3. Demonstrates a commitment to periodic self-assessment. 4. Demonstrates the ability to implement change when constructive feedback is provided. 3. Proficiency Criteria for Graduation: In addition to meeting the junior level proficiency criteria, PGY-3s must demonstrate progression in the competencies as outlined below in order to advance. Residents should use the milestones file on the residency website as a guide to determine if they are meeting current requirements. 16 of 92 Medical Knowledge Patient Care Display mastery of knowledge related to disease prevention and treatment in Internal Medicine. 1. Display mastery of skills related to disease prevention. 2. Demonstrate the ability to function effectively and efficiently in a multitude of settings, from the office to the ICU. 3. Demonstrate a deep appreciation for the psychosocial complexities inherent in the delivery of patient care. 4. Demonstrate the ability to identify and deal effectively with complex ethical issues. Interpersonal & 1. Demonstrate the ability to communicate effectively and directly with Communication consultants from within and outside the specialty of Internal Medicine. Skills 2. Demonstrate the ability to communicate effectively with the referring physicians, third party payors, risk management, etc. 3. Exhibit mastery of concise, accurate and legible note writing. Professionalism 1. Demonstrate a high standard of personal honesty and integrity. 2. While exhibiting humanistic qualities in caring for patients, function as a role model to other members of the healthcare team. 3. Demonstrate a deeper understanding of the importance of the team approach to health care delivery. 4. Demonstrate a continued commitment to community service. 5. Respond to administrative requests, pages and email communication in a timely manner. 6. Record >80% attendance at ALL academic conferences and board review with active participation. 7. Adherence to all program policies and requirements. 8. Demonstrate the ability to accept feedback related to any of the competencies and demonstrate change. Systems Based Demonstrate participation in various forums in the local environment Practice geared at improving systems and quality. Practice Based 1. Display the ability to critically evaluate ones performance and Learning implement methods to enhance outcomes. 2. Display the ability to critically appraise literature. Research, 1. Completion of research project as prescribed by the Residency Procedures, Research Committee. Tests 2. Fulfillment of procedural competency as prescribed by the Residency Procedural Committee. 3. Obtaining EKG certification through an EKG test. 17 of 92 Policy Name: Recommendation Letter Policy Policy Number: 9 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: One of the program’s primary obligations is to provide recommendation letters for future positions. These letters are needed for fellowships, appointments to hospitals’ medical staffs, entrance to board examinations, state licensure, etc. Although it is our intention and desire to write a strong and favorable evaluation for each resident, it should not be assumed to be automatic. Policy: Letters will be composed based on the following areas: 1. Academic excellence, scholarship, clinical competence (medical knowledge, clinical skills, clinical judgment) and actual patient care. 2. Humanistic qualities. 3. Professional attitudes and behavior. 4. Moral and ethical behavior in the clinical setting. 5. Evaluation by peers, attending staff, and other members of the health care team (e.g. nurses). Patient evaluation. 6. Medical record review and timeliness of completion of medical records. 7. Attendance and participation in all program activities such as morning report, noon conference, board review sessions, and Grand Rounds. 8. Ability to be a team player. 9. Research efforts and accomplishments. 10. Community service is not required by the residency program. However, if you volunteer to perform community service, it will be incorporated into recommendation letters. Once the recommendation letter is sent, it is the policy of the Residency Program to issue periodic (every three to six months) follow-up letters to fellowship directors stating the current level of your performance. It is expected that residents demonstrate the same or improved performance after having obtained a fellowship position. This policy will also apply to all future employers. The letter of recommendation will include the program’s observations on each of the above items along with any other pertinent matter. Please do whatever is necessary to help produce a strong testimonial for yourself. 18 of 92 Policy Name: Leave of Absence Policy Policy Number: 10 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: This policy ensures that residents are aware of the sick leave provisions and their possible effects on training completion and board eligibility. Policy: Residents enrolled in the categorical program are allowed sick leave (includes maternity leave) OR vacation of up to 12 weeks over the three years of training in accordance with the leave of absence policies established by the American Board of Internal Medicine, effective June 1999. Residents are required to extend their training to cover any days missed beyond the 12 weeks, in order to be board eligible. With 4 weeks of vacation scheduled yearly, any sick days taken may proportionately shorten future vacation time or extend training beyond the required duration of 36 months. Residents who avail themselves of sick leave in accordance with university and union policies should be aware that this does not necessarily ensure timely ABIM board eligibility. 19 of 92 Policy Name: Schedule Requests Policy Policy Number: 11 Approval by Program Leadership: 7/1/05 Amendment Date: 05/31/09 Purpose: The program recognizes the need for residents to have the opportunity to request specific non-call days off in given months. This policy outlines the uniform policy for granting such requests. Policy: 1. All requests will be decided on a first come, first serve basis. 2. All requests must be made by email to rwjmsimchiefs@gmail.com, in the following format: Service: Month: Day: 3. Residents may only request one (1) day not to be on call per service month. 4. No requests will be honored after a written schedule is distributed unless in the case of extenuating circumstances. 5. Residents are not permitted to submit requests seeking a specific colleague, attending, rotation, or site. 6. Residents will automatically be scheduled such that they are not on call postnight float/overnight call from another service. This will take precedence over other residents' requests for days not to be on call. 7. No days off will be granted on a residents clinic day unless prior approval from the site chief is obtained. 20 of 92 Policy Name: Medical Records Completion Policy- RWJUH Policy Number: 12 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: This policy governs the maintenance of comprehensive, legible, and timely medical records at RWJUH. In order to comply with regulations of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), all discharge summaries must be completed rapidly after a patient’s discharge. Policy: 1. All patients discharged from the Medical Teaching Service (MTS) REQUIRE a discharge summary in Sunrise Clinical Manager. 2. The senior resident on a team has primary responsibility for completion of discharge summaries and will be held responsible for delinquent charts. 3. Discharge summaries should be completed ON THE DAY OF DISCHARGE. 4. In the event that the senior resident is not present on the day of discharge, the intern must complete the discharge summary that day. 5. The residency program will supply Health Information Management (formally known as Medical Records) with a list of all residents’ and interns’ email addresses. The resident will receive emails concerning their outstanding charts. However, it is the primary responsibility of the resident to maintain a personal list of charts that require completion and to complete these in a timely manner. The resident should not wait to be notified by HIM that charts are delinquent. 6. If the residency program becomes aware that a resident has delinquent charts, the resident will be contacted by the Chief Resident. The resident will be given 48 hours to complete the charts. Failure to complete the discharge summary within 48 hours will result in the resident being placed on Academic Warning/Probation as outlined in Policy #25. 7. Suspension of an attending physician secondary to a resident’s failure to dictate discharge summaries will result in the resident being placed on Academic Warning/Probation. 21 of 92 Policy Name: Medical Records Completion Policy - UMCP Policy Number: 13 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: This policy governs the maintenance of comprehensive, legible, and timely medical records at UMCP. In order to comply with regulations of the Joint Commission on the Accreditation of Healthcare Organizations (JCAHO), all discharge summaries must be completed rapidly after a patient’s discharge. Policy: 1. All patients discharged from a Medical Teaching Service (MTS) team require a discharge summary to be completed in QCPR. Exceptions to this policy are patients discharged by private attendings. 2. The senior resident on a team has primary responsibility for completion of discharge summaries and will be held responsible for delinquent charts. 3. Discharge summaries should be completed ON THE DAY OF DISCHARGE. 4. In the event that the senior resident is not present on the day of discharge, the intern must complete the discharge summary that day. 5. Senior residents will maintain a personal list of charts that require discharge summaries during any service month. 6. If the residency program becomes aware that a resident has delinquent charts, the resident will be contacted by the Chief Resident. The resident will be given 48 hours to complete the charts. Failure to complete the discharge summary within 48 hours will result in the resident being placed on Academic Warning/Probation as outlined in Policy #25. 7. Suspension of an attending physician secondary to a resident’s failure to dictate discharge summaries will result in the resident being placed on Academic Warning/Probation. 22 of 92 Policy Name: Moonlighting Policy Policy Number: 14 Approval by Program Leadership: 7/1/05 Amendment Date: 9/24/07 Purpose: The opportunity to moonlight during residency is a privilege. PGY3 residents will be permitted to moonlight exclusively during elective rotations as long as they do NOT interfere with day schedules, pinch hitter list or program needs, if they meet eligibility criteria listed below. Policy: Eligibility Criteria: 1. In-training exam scores ≥ 60th percentile. 2. Superior performance in all areas of clinical competence based on evaluations and contents of the residents’ file. 3. Punctuality, attendance, and participation at all conferences, including Board Review. If a resident’s academic performance declines after being granted moonlighting privileges, the residency program reserves the right to deny continued opportunities for outside employment. Eligibility status will be evaluated on a quarterly basis by the program director. Mandatory duty hour documentation must be submitted when moonlighting and must not exceed the 80 hour maximum work week. A completed application for moonlighting privileges must be submitted to the program for approval. Thereafter, any changes in the outside employment status (different hospital, additional site, etc.) require prompt notification and completion of additional paperwork. It must be noted that seeking outside employment without prior consent form the program director will result in termination, in accordance with university policy. Further information can be obtained by accessing Section 3-2 of the UMDNJRWJ Medical School Graduate Medical Education Policy Manual at http://www2.umdnj.edu/pgmeweb/index.html. 23 of 92 Policy Name: Call Coverage Policy Policy Number: 15 Approval by Program Leadership: 7/1/05 Amendment Date: 5/31/09 Purpose: This policy ensures uniform guidelines for obtaining coverage of on-call responsibilities. Policy: 1. Residents may not arrange for coverage of any call in a given service month unless extenuating circumstances with prior approval from site chief. 2. The service attending must be informed of and agree upon any changes to the call schedule. They must be fully aware of which resident is covering their patients at all times. 3. The covering resident must attend all required program activities and not exceed the ACGME work hour limitation. For example, a resident who covers a night of night float, will still be required to attend their elective/clinic and all conferences the following day. 4. The site chief must grant final approval of any call changes. This will be done via email only. 5. Switching calls among residents on the same rotation is not permitted unless extenuating circumstances with prior approval from site chief. This will only be allowed if there are no other alternatives. 6. Residents may not at any time develop arrangements over the course of the year that would allow them to “bank” compensation days from fellow residents. This applies to all service and elective rotations. For example, a resident MAY NOT arrange to cover multiple residents over the course of the year with the intention of asking for compensation on consecutive days. 7. No resident may take more than one consecutive day off of any rotation without prior approval from the chief residents. 8. A pinch hitter may be used for floor coverage only if another pinch hitter has been found to cover the pinch hitter schedule. This will require prior approval from site chief and all pinch hitters on schedule must be available during their designated weeks. 24 of 92 Policy Name: Communication Policy Policy Number: 16 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: This policy describes the process by which program information will be disseminated. Policy: 1. Each resident is required to identify a primary email account preferably UMDNJ which will be the primary vehicle of communication. 2. All residents should also identify the phone numbers (home and cell), and address to which information should be directed. It is the resident’s responsibility to update his/her contact information. 3. Residents are responsible for checking their designated email address frequently (daily is suggested) as information pertinent to the next day’s events (i.e., cancellation of board review) and to UMDNJ will be communicated this way. 4. Residents are responsible for checking the Angel website monthly for updates on elective manual, syllabus, pinch hitter list, academic calendar, etc. 5. All requests (float days, days not to be on call, call coverage) should be emailed to the chiefs at rwjmsimchiefs@gmail.com. Verbal requests will result in a response of “Email it to us.” This is done to ensure timely responses to requests. 6. Residents must respond promptly (within 10 minutes) to all pages from the chiefs or residency office. These pages will end with either: 732-2357741/7742, 609-497-4484. 7. Residents must not post any patient identifiable or protected information to any social media websites. Additionally residents are reminded to conduct all communication, including electronic, in a professional manner. 25 of 92 Policy Name: Vacation Policy Policy Number: 17 Approval by Program Leadership: 7/1/05 Amendment Date: 5/25/10 Purpose: To ensure that each resident understands the options for scheduling vacation. Policy: There are two vacation options: 1. Two blocks of two weeks. 2. For residents applying for fellowship, they have the following option: one block of two weeks, one block of one week and five float days (applicable to PGY2 residents, PGY3 residents, and PGY1 residents on the ABIM research pathway). If the float days are not needed for interviews, the resident will receive the remaining days as a block of days at the end of his or her third year. This will be granted once the chief resident has a complete list of used float days. 26 of 92 Policy Name: Float and Personal Day Policy Policy Number: 18 Approval by Program Leadership: 7/1/05 Amendment Date: 5/25/10 Purpose: This policy addresses float day and personal day usage throughout the academic year. Policy: Personal days refer to the three personal days each resident is entitled to by contract, and float days refer to the additional five days given to those residents who elected to take only three weeks of scheduled vacation. The scheduling of these days is up to the resident as per the float day usage policy below. Personal days will not be carried over to the next academic year but float days may be based upon the aforementioned criteria in Policy 17. Float Day and Personal Day Usage On Service: Float days may be used on service for interviews only and rare exceptions (e.g. family emergency such as sick relative or childbirth) and as granted by the chief resident for other emergent reasons. A maximum of two float days may be used per service month with a maximum of six days off from work per month including four regular days off. If a resident elects to use a float day on a service month, he/she must find coverage from an appropriate colleague who is not on pinch hitter. All of these changes need to be approved by the site chief resident. Any additional time off may necessitate a leave of absence (see Policy 10: Leave of Absence). A resident may take a maximum of two consecutive days off from work when interviewing. If float days are used on service, proof of interview must be provided. If granted for other emergent reasons additional documentation such as proof of travel must be provided. On Elective: May be used for interviews, USMLE, national conferences for which a resident does not have work being displayed and personal reasons Maximum of one day in a two week elective Maximum of two days in a four week elective Maximum of two consecutive days off, except when taking USMLE Step 3 and COMLEX Level 3 27 of 92 If the resident takes USMLE in a given elective block, he/she is not permitted to take additional personal days. If a resident is interviewing during that year, it is expected that all personal days be reserved for that purpose. If a resident has used more than the allotted float/personal days during interview season AND used days earlier in the year not associated with interviews, a second year resident may be subject to lose vacation days during their third year and a third year resident may need to have remediation of that time prior to graduation. USMLE Step 3 and COMLEX Level 3: Residents will get 3 additional personal days to take the USMLE Step 3 or the COMLEX Level 3 Two days to take the exam and one day either pre-or post test USMLE STEP 3 and COMLEX Level 3 must be taken while on an elective and not on selective when it conflicts with additional clinics. A resident cannot be on pinch hitter and planning to take the USMLE STEP 3 unless coverage as dictated below has been found by the resident taking the exam Procedure for requesting usage of float/personal days a. Notify site chief two weeks in advance. b. Chief resident will review request, grant final approval and send notification via email. c. No request for personal days will be granted during GIM consults elective. If a resident elects to use a float day on GIM consults for interviews, he/she must find coverage from an appropriate colleague who is not on pinch hitter. d. Use of float days to be grouped together as vacation or for other purposes will need approval from the site chief. e. Emergent or urgent use of personal or float days require a phone call to the site chief resident. Please note that a request for personal days is not approved until e-mail notification is received from the chief resident. In way of unexcused absences, if it is confirmed that a resident was not present on any day of an assigned rotation without prior approval from the chief residents, the resident will be placed directly on Academic Warning/Probation and may be grounds for dismissal proceedings. 28 of 92 Policy Name: National Conference Policy Policy Number: 19 Approval by Program Leadership: 7/1/05 Amendment Date: 5/20/10 Purpose: The residency program encourages and rewards residents who are selected to present at national conferences. This policy governs the scheduling of national conference attendance. Policy: If the resident is on elective, they are excused for the conference from elective duties. The program will provide up to three days of professional time to present at the conference, which will not be counted against personal days. If the resident is on service, the program will provide up to three days of professional time to present at the conference. This will entitle the resident to a total of seven days off from work for the month including his or her regular four days off. A resident may not be out for more than three consecutive days during service. The call schedule will be arranged so that no calls are missed. If a call must be missed, the site chief resident will determine who covers that call. It will first fall to back-up but if backup is not available, a pinch hitter may be pulled and no payback required if and only if eight weeks advance notice was given. Clinics will be canceled on a case by case basis determined by the chief resident and program leadership. If a resident is invited to present at the conference, eight weeks advance notice must be given to the chief resident. Residents may not miss clinic to attend a conference where they are not presenting. National conference attendance is permitted only if you are a presenter. Vacation/Personal days should be used if residents choose to attend a national meeting as an attendee. 29 of 92 Policy Name: Pinch Hitter Policy Policy Number: 20 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: This policy governs the usage of the pinch hitter system. Policy: 1. For USMLE Step 3, every attempt should be made to schedule time off during an elective. Each resident is entitled to get three days to take the USMLE Step 3. If a pinch hitter is used, equivalent pay back is required. 2. For COMLEX exams, which are only offered in December and June, every attempt should be made to take the exam while on elective. If this is not possible, and a resident is on service, a pinch hitter will be pulled. Payback is not required as the exam is only offered at specific times. 3. Bereavement leave due to the death of an immediate family member does not require payback. 4. Approved time to present at a national conference during a service month does not require equivalent payback. 5. The pinch hitter list is not written in the order that residents will be pulled, but no resident will be pulled for a second time before others on the list are called. 6. Residents may seek coverage for their time on the pinch hitter list. To switch pinch hitter coverage, the resident on the pinch hitter list must notify the chief residents and provide a number where he/she can be reached. In addition, you must email the chief residents at rwjmsimchiefs@gmail.com and inform them of the switch. 7. Failure to return a call within ten minutes while on pinch hitter will place the resident in the number 1 position on the pinch hitter list for an additional 2 weeks on their next elective. They will also be required to provide equivalent payback to the person pulled in their place. The chief residents will attempt to contact the person on pinch hitter by all contact numbers prior to pinching someone else. 8. Residents assigned to pinch hitter must be able to arrive for clinical duties within ninety (90) minutes of pinch notification by the chief resident. 9. If the chief resident is not notified of any pinch coverage switches, the person originally assigned for pinch hitter will be held responsible for any problems that occur with coverage. 30 of 92 Policy Name: Required Procedure Policy Policy Number: 21 Approval by Program Leadership: 7/1/05 Amendment Date: 7/17/09 Purpose: Residents must know the indications, contraindications, complications, and limitations in designated procedural skills and develop technical proficiency in those designated procedural skills. Documentation of a physician’s procedural experience is a requirement for credentialing with hospitals and healthcare organizations. Policy: In order to perform procedures independently and graduate from the program each categorical resident must complete the following: 1. Take and pass a written exam that contains questions pertaining to techniques, indications, benefits and risks, and alternative options for Central Line Placement, Thoracentesis, Paracentesis, Lumbar Puncture and Arterial Cannulation. 2. The written exam must be completed and submitted in order to be granted credit or supervisory status for any of the above mentioned procedures. 3. Maintain Advanced Cardiac Life Support (ACLS) certification throughout the residency. It is the resident’s responsibility to make sure that all certification and documentation is current and that a copy of their issued card is in their residency file in the residency office. The residency program will reimburse for ACLS course costs. 4. Procedures: Procedure Recommended to graduate Required to perform independently (Technical Proficiency) Obtain arterial blood gas 5 0 Nasogastric Intubation 3 0 Breast Exam 3 0 Pelvic/Pap Exam 5 0 Rectal Exam 5 0 Abdominal Paracentesis 3 2 Lumbar Puncture 5 3 Central Line Placement* 5 3 Thoracentesis 5 3 Arterial Line 2 2 *For Central Line Placement a resident must have been rated competent to perform independently on an internal jugular or subclavian placement 31 of 92 by at least one attending, fellow, or chief resident. Only one of the three required procedures can be a femoral placement. Interns are required to provide documentation of performance of the following procedures in order to advance to the PGY 2 level: 2 arterial lines 2 paracenteses 3 central lines (in any location) The above numbers are merely the minimum requirements. Resident’s personal comfort and skill level should guide the ability to supervise or perform any procedure independently, after the minimum standards established for performing a procedure independently have been met. Documentation is required in the medical record for any invasive procedure performed. Procedure notes must be dated, timed, and signed with the resident’s name and beeper number legibly printed. The procedure note should also include the procedure, the indication for the procedure, the operators, patient consent, the technique and the route used, a brief description of the procedure and complications of the procedure. The RWJ MICU time out form may substitute for a procedure note as long as there is documentation in the chart saying to see time out sheet. Documentation with the residency program is required for advancement. This will be done by submitting procedure slips to the residency office. Once a resident is certified to perform independently or to supervise others, additional procedures and the resident’s role in the procedure (i.e. acting independently or supervising others) should continue to be documented. A monthly report will be generated to all hospitals indicating each resident’s certification status and supervisory abilities. Each resident is strongly advised to maintain a personal ABIM Log Book for their own records. 5. Any resident who sustains a work-related injury while doing a procedure must send an e-mail to Peggy Morgan at morganma@umdnj.edu outlining the following: a. Outline of incident b. Date c. Time d. Hospital site e. Ongoing treatment 32 of 92 Policy Name: Research Requirement Policy Policy Number: 22 Approval by Program Leadership: 7/1/05 Amendment Date: 6/1/09 Purpose: To ensure that residents demonstrate acceptable scholarly activity during their training. The quality of the research performed by each resident will be part of the composition recommendation letters for future positions. Policy: In order to graduate from the program each resident must perform and complete scholarly activity defined as: 1. Completion of either: Hypothesis-based projects leading to new information, comprehensive case reports, literature reviews of clinical and research topics, or Internal Review Board Proposal. The final report of the project could be an abstract, a poster, a paper in a peer review publication, or an oral presentation at a regional meeting, at a national meeting, or at Residency Research Day. 2. Each resident is expected to have made a significant intellectual and practical contribution to the research project. 3. If a resident elects to take a research elective, he or she may only take four weeks consecutively and six weeks total. At the end of each two or four week block of research, he/she will be expected to give a noon conference powerpoint on his/her progress. 4. At graduation the Medicine Residency Certificate with Distinction in Research will be awarded to select residents. The Medical Residency Certificate with Distinction in Research acknowledges original research undertaken during the period of Residency in Medicine at UMDNJ-Robert Wood Johnson Medical School. It is not awarded for research done prior to acceptance to residency and cannot be granted for work credited toward any degree. This work may be carried out in any field appropriate to Internal Medicine where objective, critical inquiry can be made. a. The operation of the program will be supervised by the Committee on Residency and Fellowship Research. This Committee will be the arbiter of the appropriateness of research proposals. Committee members with a scientific or personal conflict with any project will be recused from the review process. b. Both PGY-2 and PGY-3 residents from those residents starting after July 1, 2004 are eligible to apply for the Certificate with Distinction in Research. In each year, applications from residents regardless of their year of training will be considered together. When a resident expresses an interest in participating in the program, the resident will submit a proposal or a letter of intent to apply by December 1st of the PGY-2 or PGY-3 year. 33 of 92 c. Research may be performed at any academic institution or other site where the resident was approved to do research at the time of submission of the application. d. The research project will consist of an original research question or hypothesis that can be tested. For clinical studies, the written report should be written as an article published in Annals of Internal Medicine. Guidelines for preparation of the paper should follow those on the journal's website (www.annals.org) and viewing Authors/Reviewers. For laboratory based research projects, the report should follow the instructions of The Journal of Clinical Investigation (www.jci.org). 1) All research projects are expected to be hypothesis-driven. 2) With few exceptions, the substance of the research should be prospective in nature and be concentrated in an area in which the resident's research sponsor has an area of interest/expertise. 3) The resident will be expected to be involved with all aspects of data generation and documentation. 4) A paper that consists only of a review of the work of others is excluded. e. Final decisions concerning whether or not a paper meets the program's criteria will be made by the Residency and Fellowship Research Committee. f. Residents are required to participate in a yearly Resident and Fellowship Research Day where their research experience is shared with their fellow residents. g. Residents will be only be considered if they are in good academic and professional standing with the Department of Medicine and UMDNJRobert Wood Johnson Medical School. h. Criteria for merit of the project: 1) Written report: importance of the questions, originality, scientific validity, written presentation 2) Research Sponsor Information: Completed by the sponsor and provides a brief description of the resident's project and the precise role the resident played in the project. If other individuals participated in the design of the project, collection of data, or analysis of the results, please include their specific contributions. Sponsor should include his/her CV with this report. 3) BIOGRAPHIC SKETCH: On a separate page, provide a summary of your education (beginning with your undergraduate degree) and your previous research experience. Include a list of your publications, if any. 34 of 92 Policy Name: Community Service Policy Policy Number: 23 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: To improve the health status of residents in NJ and to be a positive, recognizable symbol of the RWJ Medicine Residency Program’s commitment to the community. Policy: The involvement of ALL interns, residents & fellows in at least one community service event/year is encouraged. Projects include community education events, health fairs, blood drives, cancer awareness events, mentoring and charity walks/runs. 35 of 92 Policy Name: Continuity Clinic Policy Policy Number: 24 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: To ensure that residents will develop their own office based practice. Residents will provide comprehensive, continuous, coordinated, and timely patient care. They will develop a knowledge base of common out-patient conditions, disease management and preventive medicine. Each resident should develop an understanding of the doctor-patient relationship, and the skill necessary to coordinate, organize, and monitor care in conjunction with other health care providers. Policy: 1. Clinic Assignments: Please refer to the Clinic Assignment Schedule for individual clinic assignments. These assignments will remain in effect for the duration of training in the Residency program. There will be an orientation for all incoming categorical interns & new residents at their assigned clinic site to be determined by the program leadership. Clinic sessions will start the following day or the following Monday if the orientation falls on a Friday for ALL residents. 2. Clinic Attendance and Scheduling: Patients will be booked three months in advance, and last minute changes CANNOT be accommodated. a. In the rare event when there is a change in the resident’s schedule for the purpose of a fellowship interview, that resident is responsible for finding replacement coverage. In case of a true emergency, the clinic staff will attempt to contact patients and cancel their visits. The scheduling chief resident must approve of all changes. b. Residents are not required to report to their clinic during: 1. Night Float rotations: If the first day of night float coincides with the same day as a resident’s clinic day, the resident is expected to attend clinic prior to starting his/her night float shift. If the last morning of night float coincides with a resident’s clinic day, he or she does not need to attend that afternoon. 2. MICU rotations 3. CCU rotations 4. University Holidays and Scheduled Vacation. 36 of 92 c. Please note that Float days, Personal days or Compensation days cannot be taken on clinic days. Rare exceptions may be granted for fellowship interviews (see box below: fellowship interviewing policy). d. It is the sole responsibility of each resident to verify with his/her respective Clinic Scheduler the dates which he/she will not be reporting to their Clinic. Failure to verify the Clinic scheduler of the above-mentioned dates with a six-week minimum advance notice, will require the resident to attend the session(s) in question. e. Authorization for any Clinic cancellation outside of the rules above will require advanced approval by the Scheduling Chief Resident and the Clinic Directors. 3. Pre-clinic Conference: Continuity clinic sessions start with a pre-clinic conference at 1:15pm sharp. For each week, a resident will lead the conference based on a topic from the Hopkins outpatient curriculum (to be distributed separately). In addition, residents may create opportunities to share and answer clinical questions surrounding uncommon presentations in common disease states or unique challenges faced when providing preventive services to special populations 4. In an effort to improve our practice, residents must select patients with hypertension, diabetes and hyperlipidemia to follow over their residency. They will track HgbA1c, LDL and blood pressure longitudinally. 5. Labs or other diagnostic tests ordered: Residents are responsible for following up on patient labs. Residents are expected to check labs within one week after they are performed, and whenever they are back in the clinic. If a resident will be away from clinic, arrangement should be made with the clinic preceptor to check on laboratory and diagnostic test results. When lab tests are ordered, patients should be told that they will be contacted with results within 2-3 weeks (phone or mail), but directed to call the office if they do not receive results within this period. NOTE: This may not be the policy at all sites due to system related differences. Residents must document all correspondence with patients, even regarding normal lab values, so that preceptors know these results have been addressed. In the case of critical lab values, the preceptor and clinic site staff will respond rapidly, most likely before a resident returns to clinic. 37 of 92 Continuity clinic is an important educational experience. If there are any problems or issues with any aspect of continuity clinic, please speak with the clinic preceptor, chief residents, or Program Directors. 6. Missing clinic or canceling clinic without approval by the chief resident is unacceptable and is grounds for dismissal. 7. All residents must complete a minimum of 130 distinct half-day outpatient sessions, devoted to the longitudinal care of the residents’ panel of patients. In order to meet this requirement residents will need to attend additional clinic sessions which will occur on a day different from their regularly assigned clinic day. These extra clinics will be assigned during elective/selective time. The resident is responsible for knowing about and attending these extra clinics. 38 of 92 Policy Name: Policy for Handling of Core Competency and Performance Deficiency Policy Number: 25 Approval by Program Leadership: 7/1/05 Amendment Date: 6/26/09 Purpose: To ensure that residents understand the mechanisms by which an identified academic deficiency(ies) will be addressed. Disciplinary action can be progressive or alternatively, based on the nature of the deficiency, the Program Leadership and Promotions Committee may pursue ANY of the actions described below. Concern Card: A concern card can be put in a trainee's file by any person who comes in contact with the resident on a clinical or academic basis. This includes program directors, chief residents, teaching attendings, private attendings, fellows, fellow residents, other members of the healthcare team or administrative staff. The Program Leadership and Promotions Committee has the authority to make this a permanent part of a resident's record if deemed necessary. Academic Advisement with Plan for Corrective Action: A trainee may be placed on Academic Advisement for failing to meet expectations during training in any competency domain. The corrective action plan will include a problem definition, a specific corrective action plan, and a timeline for demonstrating corrective change. This may include, for example, increased supervision, repetition of rotation, referral for professional help, etc. The corrective action plan devised by the Program Leadership and Promotions Committee will identity person (s) who will be responsible for implementing and monitoring the outcomes. Failure to achieve the stated outcome in the timeline allotted will result in Academic Warning or Dismissal proceedings if deemed necessary. Academic Warning/Probation: Academic Warning is a condition that reflects serious concern on the part of the Program Leadership and Promotions Committee when a trainee has demonstrated behavior consistent with performance deficiencies in any competency domain, has failed to follow policies and procedures outlined by the program (ex: attendance policy,) or has failed to act on the corrective action plan 39 of 92 designed for that resident. Academic Warning is reserved for deficiencies considered significant enough to undermine the training program's expectations and standards. A formal meeting and letter will be issued in such cases with a corrective action plan. The placement of a resident on Academic Warning/Probation will be reported to state licensing bodies, future employers and fellowship directors. A resident will remain on Academic Warning/Probation for a minimum one year period or until the training completion date if that is less than one year. Additional offenses committed while the resident is on Academic Warning/Probation may result in dismissal proceedings. Dismissal: A resident may be dismissed from the training program for the reason or reasons listed below. Reasons for dismissal include, but are not limited to, the following: a. Obtaining unsatisfactory evaluations in any one of the components of clinical competence for three rotations in an academic year. b. Obtaining marginal evaluations in any one of the components of clinical competence for five rotations in an academic year. c. Failure to satisfy the conditions for removal from Academic Warning d. Deliberate falsification of official records or required program information. e. Inability to complete residency requirements. f. Absence of the personal qualifications and attributes deemed necessary to perform the duties of the medical profession. Appeals Process: In accordance with the GME appeals process from RWJMS GME Policy Manual, (1) The house officer may appeal the program director's adverse academic decision to an Ad Hoc Appeal Committee, established as indicated below, or to the residency program's standing Committee on Housestaff Evaluation (or its equivalent). This appeal must be made in writing to the program director within five working days of having received notification of termination or an adverse action. (2) If the house officer submits a timely notice of appeal, the director shall schedule a meeting of the residency program Committee on Housestaff Evaluation or convene the Ad Hoc Appeals Committee. The Ad Hoc Appeals Committee, if created, should consist of [not fewer than five] faculty members of the division, department of the group, or departments responsible for the program. The faculty members selected for this purpose shall be experienced faculty in the area of graduate medical education. The number of members of the Ad Hoc Committee shall be large enough to be representative of the faculty of the division, department or group of departments responsible for the program. The committee considering the house officer's appeal should include at least one house officer. (3) The house officer may request to meet with the Committee in person and be accompanied at the hearing by a faculty member or fellow house 40 of 92 officer who may act as an advisor. If a CIR representative has not previously determined that the matter at issue is academic, the house officer may also be accompanied by a representative of the CIR who shall not participate in the proceedings. (The CIR representative's only role in the hearing is to make a determination whether the matter under discussion is a bona fide issue of academic performance.) The program director will also be present at the hearing at which time he or she shall set forth the circumstances leading to the planned adverse action or the reasons for which the house officer has been dismissed. Following the presentation, the house officer and/or their advisor shall be permitted to set forth whatever information the house officer wishes the Committee to consider as reasons to vacate the decision to endorse the adverse action or to dismiss the house officer. (4) Following the hearing before the Committee, the Committee will immediately confer and, following deliberations, advise the Department Chair in writing of its recommendation and the reasons for that decision of the Chair shall be final. If the Department Chair is the Program Director, the decision of the Committee shall be final. This decision shall be conveyed to the house officer in writing. The Chair shall provide copies of the notice of adverse action or dismissal to the associate or assistant dean responsible for graduate medical education. . 41 of 92 Policy Name: Sick Day Policy Policy Number: 26 Approval by Program Leadership: 7/1/05 Amendment Date: 9/24/07 Purpose: This policy governs absence from work due to illness. Policy: 1. The site chief and elective coordinator must be notified as soon as possible. 2. A physician’s note (not from a resident or fellow) must be provided if a resident is absent from work for more than two consecutive days. There may be circumstances where a physician’s note may be required even if absence is from a single day of work. (ex. Suspected misuse of sick leave policy) 3. In the event that a pinch hitter is used to cover for a resident absent secondary to illness, payback will not be required. However, payback is strongly suggested as a matter of professional courtesy. 42 of 92 Policy Name: University Holiday Policy Policy Number: 27 Approval by Program Leadership: 7/1/05 Amendment Date: 06/25/07 Purpose: This policy addresses pay offered to residents for working on designated university holidays. Policy: 1. Residents or interns working on university holidays will be paid one tenth of their biweekly pay. Those not on call are required to stay until 12:00 NOON or until their work is completed. 2. In the event that the holiday is a pick-up day for the team, both members will come in and will be paid one tenth of their biweekly pay. 3. At the start of each month, when submitting days off, each service team will tell the site chief who will be rounding on a holiday. If a team is not on call or pick-up, only one member of the team may work and receive holiday compensation. 43 of 92 Policy Name: Due Process Policy Policy Number: 28 Approval by Program Leadership: 7/1/05 Amendment Date: 9/24/07 Purpose: This policy describes the process for disputing an academic disciplinary action. Policy: 1. Discuss the action in question with the Program Director, Internal Medicine Residency. 2. In the event that a satisfactory resolution cannot be reached, the resident may appeal to an Ad Hoc Appeals Committee appointed by the Program Director or his/her designee. (refer to GME manual, section on Appeals Process) 44 of 92 Policy Name: RWJUH Service Policy Policy Number: 29 Approval by Program Leadership: 7/1/05 Amendment Date: 7/22/11 Purpose: To expose residents to a wide spectrum of diseases in multiple settings (i.e. MICU, floor, night float and oncology floor). Policy: A. Services It is the responsibility of residents to play an active role in all patient encounters. (Take a thorough history and physical exam, present case to attending, discuss management and document appropriately in the chart.) Residents must follow the policies on progress notes, clinics, dictations, work hours, pinch hitter, evaluation, coverage, sign-out/transitions of care, etc. as mentioned above. 1. FLOOR SERVICE: a. Medical Teaching Service (MTS): 5 general medicine teams consisting of two or more residents each responsible for the care for patients without a primary cardiology presentation or oncology diagnosis. 1) Includes patients without a primary care physician with privileges at RWJUH or patients who receive primary care through RWJMG (not consults). 2) Composed of residents and a service attending (i.e. Program Directors, chief residents or university faculty members) 3) Teams admit every 5th day and begin admitting from 7:00 am (8:00am on weekends/holidays) until 7:30 pm. They may hold patients after 7:30 pm and pass them onto night float for admission. Patients received prior to 7:30 pm will not be admitted by night float; the primary team will stay and finish that admission with the help of night float as needed. Patients admitted by night float will be redistributed to the pickup team the following morning. a) Accept max two admissions per hour from ER but if called to admit then able to give attending name for booking purposes. b) Each intern must not be assigned more than five new patients per admitting day. An additional 2 new patients may be assigned if the on call team has either a sub-intern or psychiatry intern. A further two patients may be assigned if they are in-house transfers from the medical service. c) Each intern must not be assigned more than eight new patients in a 48 hour period. d) Each intern must not be responsible for the ongoing care of more than 10 patients. 45 of 92 e) A supervising resident; when supervising one intern must not be responsible for the ongoing care of more than 14 patients; when supervising more than one intern must not be responsible for the ongoing care of more than 20 patients. f) The supervising resident, must not be responsible for the supervision or admission of more than 10 new patients and 4 transfer patients per admitting day or more than 16 new patients in a 48 hour period. g) Preliminary admission orders to be placed within one hour of call from ER attending h) If attending does not wish to accept patient, the ER attending must be called by the attending or the attending must be notified prior to the resident discussing the case with the ER attending i) Transfers from outside hospitals and from other services must be accepted directly by an attending physician j) No internal medicine housestaff will be provided for patients with stroke/neurological disease only as there is a neurology service except in the MICU. k) No internal medicine housestaff for patients with Family Practice attendings except in the MICU, unless that physician does not admit to RWJUH. l) Anyone under the age of 21 without a primary medicine doctor goes to Pediatrics m) No internal medicine housestaff for pregnant patients with exception in the MICU. All such patients will receive GIM consults if the chief complaint is primarily medicine related. n) Patients with fractures admitted to RWJUH will be admitted either to the orthopedic or General Internal Medicine (GIM) services depending on their comorbidities: i. If the GIM medical attending, after discussion with the medical resident and, if necessary, the orthopedic attending, feels the patient is stable and may proceed to surgery without delay, the patient should go to the orthopedic service and GIM will consult. ii. If the medical attending feels the patient is unstable medically, requires further medical evaluation or optimization before surgery, then the patient should go to the GIM medical service with orthopedics consulting. iii. Any disagreements should be resolved between the GIM medicine and orthopedic attendings directly and should not involve the ER staff or either resident team. o) The senior resident fills out a screening log every time on call. 4) Saturday/Holiday Call: The following call schedule applies for Saturday and holiday calls a) Senior residents will arrive at 8am and work a continuous 24 hour shift until 8am the following morning at which time they will leave. 46 of 92 b) The on-call intern will arrive at 8am and work a 12 hour shift until 8pm. During this time they will admit patients with the supervision of the on-call senior as well as take sign outs and provide cross coverage for the four non-call teams. c) At 8pm the following day’s pickup team’s intern will report and work a 16 hour shift until 12noon the following day. They will admit patients with the on-call senior and provide cross-coverage. Patients admitted from 8pm to 8am will be followed by the pickup team. 5) Pickups: Pickup occurs every 5th day by a team different than the previous day on-call team. a) Redistribution should occur: i. if pickup team’s census will be greater than 14 ii. if there are more than six pickups iii. if non-call teams are at less than six patients b) Order of Redistribution: i. First, subspecialty, then GIM (GIM to GIM teams), and finally service patients c) Redistribution should not be conducted in such a way that gives any other team more new patients than the pickup team unless this cannot be avoided given current census d) The admitting team may pickup a patient if it is a bounceback or all other teams have a census of 14 patients 6) ICU Transfers: a) Transfers from MICU/CCU: i. The day team will write a transfer note if a patient requires housestaff and is anticipated to transfer prior to leaving for the day. The on call ICU intern will notify the appropriate resident when a bed is assigned: #2250- UPCC go to MTS, UCG go to MTS with MTS attending approval of teaching quality, and CINJ or unassigned liquid malignancy patients go to OTS. ii. Whomever is holding 2250/2251 at the time the bed outside of the ICU is assigned takes the patient (regardless of when the patient was put up for transfer) iii. Floor team should see the patient, review the chart/transfer note, write a brief accept note, notify the attending, and change the attending of record (if necessary) with admitting (ext 8602). b) Transfers to MICU/CCU: i. For floor patients with housestaff the MTS/OTS teams act as unit screeners. These residents should stabilize the patient, write a transfer note, place the initial unit orders, and call #2373/2374 (CCU/MICU screener) to get a unit bed assigned. ii. Responsibility remains with floor teams until patient physically in unit or ICU resident takes over (including codes). 7) Sign offs: It is intended that the majority of patients followed by resident teams will be followed from admission through discharge. 47 of 92 When it is necessary to sign-off of a patient, sign-offs will be performed according to the following guidelines: a) Only university group subspeciality patients can be considered for sign-off. b) Indications for Sign-off: i. High Census: A team census greater than 14 (or >10 going into a call day). Complexity of other patients being covered by the team may also be considered. The order of sign-offs will be based on value/appropriateness of patient as a teaching case. For example, a patient awaiting placement will be considered for sign-off before a patient with diagnoses/workup established before patients with investigation/workup in preliminary stages. ii. Physician of record unavailability: Each physician of record has the responsibility to communicate effectively and frequently with the resident staff participating in the care of these patients. iii. Patient refuses to be seen or examined by the resident team. c) When signing off on a patient the resident is responsible to notify the attending of record and the patient’s nurse and to write a note in the chart stating that residents have signed off on the patient’s care. 8) Faculty Admissions: a) Patients without a physician with privileges at RWJUH will be admitted to the medical service team admitting on that day. b) Any subspeciality patients presenting with that same subspeciality complaint followed by a faculty subspeciality attending will be admitted to their service unless otherwise approved by the chief resident 1. If subspeciality attending feels that the patient is sick enough to warrant housestaff coverage, then that can be approved through the chief resident 2. If the chief complaint falls out of the jurisdiction of the subspeciality attending, that patient will be admitted to the medical teaching service. 9) Transitions of Care: a) In an attempt to minimize the number of transitions in patient care, to ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require residents to adhere to the following guideline regarding transitions of care: b) All patients cared for by the Medical Teaching Service must have a written sign out completed using the hospital intranet 48 of 92 system only. Signouts should be kept secure as they contain protected health information. c) Sign out should include the following: a. Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b. A brief description of the reason for admission c. A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d. Any recent procedures or tests d) Sign out must be updated on a daily basis to reflect changes in the patient’s clinical course. e) Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. f) The on-call and coverage schedules for residents and attendings on teaching service is available on the hospital intranet 2. ONCOLOGY TEACHING SERVICE (OTS): a. One team consisting of two residents, one oncology fellow, and an attending CINJ oncologist. The CINJ oncologist attending and oncology fellow assigned to OTS are responsible for the direct supervision of the residents and assist the residents in direct patient care. 1) Leukemia/Lymphoma Service: Responsible for the care of patients with known hematologic malignancies including leukemia, lymphoma, myeloma, etc., admitted for oncology related issues. b. Any CINJ patient with a known liquid malignancy admitted with an oncology-related issue. 1)OTS does not follow: Bone Marrow Transplant patients, patients admitted to the MICU, Private Oncology pts, Hematology service patients (Hematology service patients needing house staff should be admitted to MTS). c.,A resident must not be responsible for the ongoing care of more than 12 patients. The resident must not be responsible for the admission of more than 10 new patients and four transfer patients per admitting day or more than 16 new patients in a 48 hour period. d. The GIM consult resident will cross-cover and admit for liquids from 4:30-8:00 pm Monday through Friday. 1) On days when GIM consult resident is in clinic, one resident from liquids will continue to cover their service and GIM consults after 4:30 until the GIM resident returns. e. On weekends, the on-call liquid resident will cover and admit for liquids as well as do GIM consults. f. On holiday weekends, RWJ GIM will be asked to cover a Sunday call if the holiday involves a Monday or Friday and Saturday overnight call if it involves Thanksgiving. 49 of 92 g. Transitions of Care: a) In an attempt to minimize the number of transitions in patient care, to ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require residents to adhere to the following guideline regarding transitions of care: b) All patients cared for by the Oncology Teaching Service must have a written sign out completed using the hospital intranet system only. Signouts should be kept secure as they contain protected health information. c) Sign out should include the following: a. Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b. A brief description of the reason for admission c. A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d. Any recent procedures or tests d) Sign out must be updated on a daily basis to reflect changes in the patient’s clinical course. e) Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. f) The on-call and coverage schedules for residents and attendings on teaching service is available on the hospital intranet 3. MEDICAL INTENSIVE CARE UNIT SERVICE (MICU): a. One month rotation of four senior residents and two interns. There are two teams, each composed of two residents and one intern. For the first two weeks, one resident from each team and one intern are assigned to day shift and the other two residents are assigned to night shift For the last two weeks the senior residents switch day and night shift responsibilities. Day shift residents are expected to be present from 7am to 7pm. Night shift residents are expected to be present from 6pm-12 noon the following day. 1) MICU patients are defined as those patients admitted to the MICU who have a non-cardiac reason for being admitted to the ICU (i.e. septic shock, GI Bleed, etc) or a UPCC primary attending b. Admission assignment: 1) Back-up will admit for the MICU from 7 am to 12 pm on weekdays and will hold #2374 during this time. 2) One resident will hold #2374 from 12 pm to 6pm daily. 50 of 92 a) This resident will be responsible for leaving the ICU to screen patients if necessary. Residents should encourage their intern to accompany them on screens whenever possible. b) Whoever is on call for the day will hold #2376 from 7am – 6pm c) All admissions will be assigned in a trickle system to each team with caps of 14. 4) Each intern must not be assigned more than five new patients per admitting day: an additional two patients may be assigned if they are in-house transfers from the medical service. 5) Each intern must not be assigned more than eight new patients in a 48 hour period. 6) Each intern must not be responsible for the ongoing care of more than 12 patients. 7) A supervising resident; when supervising one intern must not be responsible for the ongoing care of more than 14 patients; when supervising more than one intern must not be responsible for the ongoing care of more than 24 patients. 8) The supervising resident must not be responsible for the supervision or admission of more than 10 new patients and 4 transfer patients per admitting day or more than 16 new patients in a 48 hour period. 9) In the event that the MICU teams are capped with a total of greater than 28 patients, the CCU team will be responsible for covering MICU patients. Preferentially these patients will be non-UPCC patients. 10) In the event that the CCU team is capped with a total of greater than 14 patients, the MICU may be responsible for covering CCU patients. Preferentially these patients will be non-UCG patients. c. Night shift: 1) Each resident will do two weeks of night shift during their rotation. The MICU night shift resident is responsible for admitting for the MICU, cross-covering MICU patients, and holding beepers #2374/2376. 2) Over a two week period, night shift will be shared by two residents alternating 18 hour shifts from 6pm-12noon the following day. 3) The MICU night shift resident will be expected to attend night-time intensivist rounds, and MICU attending rounds and didactics. 4) The MICU night shift resident will be responsible for the care of any UPCC patients admitted during that shift as well as presenting these patients on attending rounds. d. Weekends/Holidays: 1) One member from each team is off each weekend/holiday day. The other member of the team is responsible for rounding on their patients and ensuring an accurate transition of care to the night shift member. 2) The senior resident will screen for the entire MICU and the intern will act as cross-coverage. 3) On weekends, the MICU night shift is responsible for screening from 7am-12noon in order to allow the day shift to round. 51 of 92 4) On Sunday when the CCU senior resident is off, the MICU senior resident will also be responsible for screening for the CCU. e. Clinic: Residents will be excused from all outpatient clinic responsibilities while on critical care rotations. f. Days off: Each intern gets 4 days off per month. These days are assigned and will be one weekend day per week. Each senior resident will get one weekend day off per week of days shift. While on night shift senior residents get alternating nights off. g. Education: 1) Residents and interns will receive didactics Monday, Tuesday, and Thursday from UPCC attending while in the ICU. 2) Rounds will take place as follows: a) Attending rounds Monday through Friday 10:30 am to 12 pm b) Sign-out rounds from 6pm to 7pm on MICU patients led by residents occurring at bedside c) Interdisciplinary rounds Monday, Wednesday, and Friday from 9:30 am to 10:00 am. h. Intensivists: Every night, critical care physicians are in the MICU to help care for patients and will round with the night shift residents from 9-10 pm. Their role should be to assist in caring for new and existing patients. They may also supervise procedures. It is each resident’s responsibility to notify the attending physician regarding all care that you render to the patient, and to document what has been done, even when assisted by the intensivist. i. ICU Transfers: (See ICU transfer policy above for more details). j. Transitions of Care: a) In an attempt to minimize the number of transitions in patient care, to ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require residents to adhere to the following guideline regarding transitions of care: b) All patients cared for by the MICU Service must have a written sign out completed using the hospital intranet system only. Signouts should be kept secure as they contain protected health information. c) Sign out should include the following: a. Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b. A brief description of the reason for admission c. A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d. Any recent procedures or tests d) Sign out must be updated on a daily basis to reflect changes in the patient’s clinical course. 52 of 92 e) Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. f) The on-call and coverage schedules for residents and attendings on teaching service is available on the hospital intranet 4. CORONARY CARE UNIT SERVICE (CCU): a. Two week rotation of two senior residents and one intern. For the first week one resident and the intern are assigned to days and the other resident is assigned to night shift. The following week the residents switch day and night shift. 1) CCU patients are defined as those patients admitted to the CCU who have a cardiac reason for being admitted to the ICU (i.e. cardiogenic shock, congestive heart failure, arrthymia, etc) or a UCG primary attending b. Admission assignment: 1) Back-up will admit for the CCU from 7 am to 12 pm or until rounds are done daily and hold #2373 during this time. 2) When the CCU resident is on call they will hold beeper #2373 from 12 pm to 7pm on weekdays. When the CCU intern is on call the MICU resident will hold beeper #2373 and will be responsible for screening the CCU. The CCU intern is encouraged to accompany the resident on any screens if possible. 3) Each intern must not be assigned more than five new patients per admitting day: an additional two patients may be assigned if they are in-house transfers from the medical service. 4) Each intern must not be assigned more than eight new patients in a 48 hour period. 5) Each intern must not be responsible for the ongoing care of more than 12 patients. 6) A supervising resident; when supervising one intern must not be responsible for the ongoing care of more than 16 patients 7) In the event that the MICU teams are capped with a total of great than 32 patients, the CCU may be responsible for covering MICU patients. Preferentially these patients will be non-UPCC patients. 8) In the event that the CCU teams are capped with a total of great than 14 patients, the MICU may be responsible for covering CCU patients. Preferentially these patients will be non-UCG patients. c. Day call occurs from 3-7pm split between intern and resident. 1) The CCU resident will be on call twice during the week. The CCU resident on call is responsible admitting for the CCU, cross-covering CCU patients, and holding beepers #2373 & 2375. 2) The CCU intern will be on call three times during the week and is responsible for cross-covering CCU patients, admitting CCU patients 53 of 92 with the MICU day shift resident, and holds beeper #2375. The MICU day shift resident will hold beeper #2373. d. Night shift: 1) Each resident will do one week of night shift during the two week rotation. The CCU night shift resident is responsible for admitting for the CCU, cross-covering CCU patients, and holding beepers #2373/2375. 2) Night shift will consist of Sunday – Friday 7pm-7am. 3) The CCU night shift resident will be expected to attend nighttime intensivist rounds in the MICU. e. Weekends: 1) The CCU resident will be on call for 24 hours on Saturday from 7 am to 7am the following day. The resident is responsible for admitting CCU patients, cross-covering CCU patients, and holding pagers #2373/2375 2) The CCU intern will be on call on Sunday from 7am to 7pm. The intern is responsible for cross-covering CCU patients, admitting CCU patients with the MICU on call resident, and holding pager #2375. f. Days off: 1) Each intern gets two Saturdays off in the two week period 2) The CCU day shift resident will get the Sunday after their 24 hour call off 3) The CCU night shift resident will get one Saturday night off g. Education: 1) The CCU team will round with the attending from 9:30-11:30am Monday through Friday. 2) The CCU team will receive didactics from the UCG fellow 3 x week from 11:30-12 pm. 3) The CCU team will also conduct sign-out rounds at 7pm on CCU patients occurring at bedside to transfer care from day shift to night shift. h. Intensivists: Every night, critical care physicians are in the MICU to help cover patients and will round with the night shift residents from 9-10 pm. Their role should be to assist in caring for new and existing patients. They do not care for CCU patients. They may supervise procedures. It is each resident’s responsibility to notify the attending physician regarding all care that you render to the patient, and to document what has been done, even when assisted by the intensivist. i. ICU Transfers: (See ICU transfer policy above for more details). j. Transitions of Care: a) In an attempt to minimize the number of transitions in patient care, to ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require 54 of 92 b) c) d) e) f) residents to adhere to the following guideline regarding transitions of care: All patients cared for by the CCU Service must have a written sign out completed using the hospital intranet system only. Signouts should be kept secure as they contain protected health information. Sign out should include the following: a. Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b. A brief description of the reason for admission c. A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d. Any recent procedures or tests Sign out must be updated on a daily basis to reflect changes in the patient’s clinical course. Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. The on-call and coverage schedules for residents and attendings on teaching service is available on the hospital intranet 5. NIGHT FLOAT SERVICE: a. Hours: 8pm to 8:30am Sunday through Friday Nights, Saturday and Holidays off b. Two teams of 1 intern and 1 resident 1) Admitting Resident holds pagers 2250 (MTS Admissions) 2) Admitting Intern holds personal pager 3) 2nd Resident holds 2251, 2252 (OTS admissions and coverage, general medicine consults) 4) 2nd Intern holds 2253 (MTS cross-covering) c. BEEPER LIST: 1) #2250: Admits general medicine patients to the 5 MTS teams, code team responder. This resident is responsible for filling out screening log every night. 2) #2251: Admits and cross-covers OTS Liquids team and code team responder. This resident is responsible for filling out an OTS screening log and census sheet every night. 3) #2252: Does all GIM consults. This resident must check with GIM attending on all consults to verify whether the consult should be completed or held overnight. Resident cannot hold a consult overnight without approval from GIM attending. 4) #2253: Cross covers patients on 5 MTS teams and code team responder and is responsible for filling out the census sheet every morning. 55 of 92 d. When a GIM attending is listed as the on-call attending, call the GIM service (908-685-3736) for admissions and patient issues. If the service is unable to contact that attending, have the service call Dr. Carson or Dr. Ferreira directly. e. If issues arise with a patient, call the patient’s attending, NOT the oncall attending except for GIM where the intern should call the service directly. 6. BACK-UP SERVICE: a. Specific responsibilities: 1) Attend board review and other conferences 2) Cross-cover from afternoon sign-outs for MTS until NF begins. 3) Admit for MTS when on call resident in clinic 4) Provide 7am-12 pm MICU/CCU screening on weekdays. All patients will be signed out to teams in real time. 5) Back-up will attend UPCC rounds Monday, Tuesday, and Thursday and UCG rounds Wednesday and Friday unless a patient was admitted for either attending earlier that day in which case s/he should attend those ICU rounds. 6) Assist with procedures, admissions, etc. Back-up should only be asked to help with admissions when a team has three or more patients waiting. 7) Assist interns on days when MTS residents are off as needed for guidance 8) Hold pager #2253 daily and respond to all Code Blue alerts. 7. GENERAL INTERNAL MEDICINE (GIM) CONSULTS: a. Specific responsibilities: 1) Attend board review and other conferences 2) Do new GIM consults from 7:45 am to 7:30 pm 3) Round on all existing GIM patients 4) Cross-cover and admit for liquid oncology from 4:30-8 pm Monday through Friday 5) Take Sunday call for OTS on a Monday or Friday holiday weekend 6) Take Saturday overnight call for OTS on Thanksgiving weekend 7) Hold GIM consult pager # 2252 b. These patients are not cross-covered by house staff at night/weekends. All calls should be referred to GIM answering service. B. Call Schedule There is a call schedule for each academic month that can be located on www.amion.com. The monthly attending coverage schedule can be found on the Angel website. It is the resident’s responsibility to check the call schedule and to know when he/she is either on call or covering for another resident. Each resident must leave his/her pager on until 8pm even if he or she is not on call and respond to pages within 10 minutes. 56 of 92 C. Conference/Clinic Requirements Residents must attend all required educational activities of the program including noon conference, noon report, Business of Medicine, Art of Medicine, Grand Rounds, etc promptly as per the white schedule sheet. All PGY-3 residents on night float, oncology teaching service and floor service are strongly encouraged to attend Board review. Attend weekly continuity clinic as assigned. D. Daily Schedule 1. Weekday: a. Floor service: 7:00-7:45am Board Review for residents 7:00am Sign in rounds in Resident Lounge 9:45 – 11:45am Attending Rounds 12:00 – 1:30pm Noon Report/Core Conference/Journal Club 4:30pm (or later) Sign out to Backup Resident once all work including discharge summaries and procedures are completed 8:00pm On call resident and backup sign out to Night Float in Resident Lounge Additional Conferences: Grand rounds on Wednesday morning @ 8:00 am from September to June, Art of Medicine conferences and Business of Medicine conferences as scheduled b. Oncology Service 7:00-7:45am Board Review for residents 7:00am Sign in rounds in Resident Lounge 9:45 – 11:45am Attending Rounds 12:00 – 1:30pm Noon Report/Core Conference/Journal Club 4:30 pm (or later) Sign out to GIM consult resident once all work including discharge summaries and procedures are completed Additional conferences: As noted above c. Medical Intensive Care Unit service: 7am Sign in rounds in MICU conference room 9:30am- Interdisciplinary rounds 10:30am: MICU didactics 11am-12:15pm: Teaching rounds 6:00-7:00pm Transition of care with MICU night shift 7pm-7am Night shift resident admits and cross-covers MICU d. Coronary Care Unit service: 7am Sign in rounds in MICU conference room 9:30am-11:30am-Teaching rounds 11:30am-12pm: CCU didactics 7pm Transition of care with CCU night shift 7:30 pm-7am Night shift resident admits and cross-covers CCU e. Night Float: 7:00am Sign in rounds in Resident Lounge 57 of 92 7:45am Night Float Rounds/Morning Report- MEB Lobby 8:00pm On call resident and back up sign out to Night Float in Resident Lounge f. Back-up: 7:00am Board Review for residents 7:00am-12 pm Screens for CCU/MICU, Attends UPCC rounds M/T/Th, Attends CCU rounds W/F 12:00 – 1:30pm Noon Report/Core Conference/Journal Club 1:30-4:30pm Follows daily coverage schedule found on white coverage sheets (MTS Floor coverage) 4:30pm (or later) Accepts sign-outs from MTS teams 8:00pm Backup resident signs out to Night Float in Resident Lounge g. GIM Consults: 7:00am Board Review for residents 7:00am-12 pm Round on existing GIM consults 12:00 – 1:30pm Noon Report/Core Conference/Journal Club 1:30-4:30pm New GIM Consults 4:30pm (or later) Accepts sign-outs from liquids oncology teams 4:30-8 pm Cross-covers and admits for liquid oncology 8:00pm Backup resident signs out to Night Float in Resident Lounge 2. Weekend/ Holiday: a. Floor service/Oncology service: 8:00am Sign in rounds in Resident Lounge 12:00pm (or later) Sign out to Resident holding 2253 where all work including discharge summaries and procedures are completed 8:00pm (on Sundays only) the Night Float Residents get sign out rounds in Resident Lounge On weekends and holidays the oncology teaching service covers itself (see white sheet for schedule) b. Medical Intensive Care Unit service: 7:00am Sign in rounds in MICU conference room 6:00-7:00pm Transition of care with MICU night shift 7:00pm-12:00pm Cross-cover and admit for MICU. c. Coronary Care Unit service: 7:00am Sign in rounds in MICU conference room 7:00am-7:00am (on Saturdays only) on call CCU resident admits and cross covers CCU 7:00am-7:00pm (on Sundays only) CCU intern cross covers CCU and admits new CCU patients with MICU resident d. Night Float: 8:00am Saturday morning sign in rounds in Resident Lounge 8:00pm Sunday evening sign out rounds in Resident Lounge e. Backup: Off g. GIM consults: Off except holiday weekends and Thanksgiving (see above for details) 58 of 92 E. Bounce Backs If you have taken care of a patient at any time during the month, and they again require care, they will revert to your team the following morning. An exception to this would be if another team has a low census and wishes to keep the patient with the consent of their attending. F. Beeper Schedule: 2250 Medical Teaching Service (MTS) Admissions 2251 Oncology Teaching Service (OTS) Leukemia/Lymphoma (Liquids) Admissions and Cross Coverage 2252 GIM Consults 2253 MTS Cross Coverage 2373 CCU Screener 2374 MICU Screener 2375 CCU Cross-coverage 2276 MICU Cross Coverage 2250,2251,2253, 2373, 2374, 2375, 2376 are code pagers If at any point a code pager is lost by a resident or intern, that resident or intern is responsible for paying for a new pager for that service. 59 of 92 1. Floor Weekday Coverage: Time 2250 7am On call MTS 4:30pm Resident or Backup Resident when on call resident in clinic from 12:00pm 4:30pmOn call MTS 8pm Resident 8pm – NF Resident 1 7am 2. Floor Weekend Coverage: Pager 2250 8amOn Call MTS 8pm Resident 8pm-8am On Call MTS Resident 3. ICU Weekday Coverage: Time 2373 7am Back-up 12pm 12 pm CCU Day 7pm Resident 7pm – 7am CCU Night Shift Resident 2251 OTS Liquids Resident 2252 GIM Consult Resident 2253 Backup resident or intern when on call Resident or back up in clinic from 12:00pm GIM Consult Resident NF Resident 2 GIM Consult Resident NF Resident 2 Backup 2251 On Call OTS Liquids Resident On Call OTS Liquids Resident 2252 On Call OTS Liquids Resident On Call OTS Liquids Resident 2253 On Call MTS Intern 2374 Back-up 2375 CCU Intern 2376 MICU Intern MICU Resident On call CCU team member CCU Night Shift Resident MICU Intern MICU Night Shift Resident 60 of 92 NF Intern 2 Pickup MTS Intern MICU Night Shift Resident 4. ICU Saturday/Holiday Coverage: Time 2373 2374 7am CCU Resident MICU Night 12pm Shift Resident 12 pm CCU Resident MICU Day 7pm Shift Resident 7pm– CCU Resident MICU Night 7am Shift Resident 4. ICU Sunday Coverage: Time 2373 7am MICU Night Shift 12pm Resident 12pm 7pm 7pm-7am MICU Day Resident CCU Night Shift Resident 2374 MICU Night Shift Resident MICU Day Resident MICU Night Shift Resident 61 of 92 2375 CCU Resident 2376 MICU Intern CCU Resident MICU Intern CCU Resident MICU Night Shift Resident 2375 CCU Intern 2376 MICU Intern CCU Intern MICU Intern CCU Night Shift Resident MICU Night Shift Resident Policy Name: UMCP Service Policy Policy Number: 30 Approval by Program Leadership: 7/1/05 Amendment Date: 7/22/11 Purpose: To expose residents to a wide spectrum of diseases in multiple settings (i.e. floor, and night float). Policy: A. Services It is the responsibility of residents to play an active role in all patient encounters including taking a thorough history and physical exam, presenting case to attending, discussing management and documenting appropriately in the chart. Residents must follow the policies on progress notes, clinics, dictations, work hours, pinch hitter, evaluation, coverage, signouts/transitions of care, etc. as mentioned above. 1. FLOOR SERVICE: Medical Teaching Service (MTS): 5 general medicine teams consisting of one resident and one intern each responsible for the care for non-critically ill patients. 1) Each resident team will be assigned a teaching attending 2) During weekdays teams will be assigned to early call every 5 th day and admit service/pick-a-doc patients from 7am-3pm. Private admissions will be distributed to the non-call teams by the Medical admitting resident (MAR) from 7am-3pm. ICU transfers will be accepted by the pickup team until 3pm 3) During weekdays teams will be assigned to late call every 5th day and admit service/pick-a-doc/private patients/ICU transfers from 3pm-7:30pm. Admissions called for after 7:30pm may be passed on to night float. 4) Early and late call teams will each have a cap of 5 new admissions. Night float team will have a cap of 7 new admissions with the night float intern doing the first 5 admissions and the senior resident doing the extra 2. Once the admission cap is reached all service/pick-a-doc admits will be done by housedoc and distributed to MTS teams the next morning 5) Admitting physicians must call beeper #580 with admissions. 6) Saturday/Holiday Call: The following call schedule applies for Saturday and holiday calls a) Senior residents will arrive at 8am and work a continuous 24 hour shift until 8am the following morning at which time they will leave. b) The on-call intern will arrive at 8am and work a 12 hour shift until 8pm. During this time they will admit patients with the supervision 62 of 92 of the on-call senior as well as take sign outs and provide cross coverage for the four non-call teams. c) At 8pm the following day’s pickup team’s intern will report and work a 16 hour shift until 12noon the following day. They will admit patients with the on-call senior and provide cross-coverage. Patients admitted from 8pm to 8am will be followed by the pickup team. d) There is a cap of 5 new patients from 8am-8pm and another 5 new patients from 8pm-8am. Service/pick-a-doc patients that require admission above this cap will be done by the housedoc as noted above. 7) Pickups: The pick-up team will take patients admitted by night float. a) If more than five patients are admitted overnight, night float resident will redistribute the remainder of pick-ups to the team. b) The pickup team will first pickup until their total census is at least six. The non-call teams will then be given patients to reach a minimum census of six. The night float resident will decide this redistribution. b) If the pick-up team reaches a census of 14, the night float resident will redistribute patients at their discretion. c) All ICU transfers will be taken by the pick-up team until 3pm on weekdays and 12pm on weekends. ICU transfers from 3-7:30pm will be taken by the late call team. 8) Signing off: There can be no signing off of private attending patients unless discussed with and approved by the site chief resident. There is no signing off of service or pick-a-doc patients. 9) ICU transfers: a) Transfers to MICU/CCU: 1) Floor team maintains primary care of patient until the intensivist takes over or the patient moves to ICU. Service attending will discuss case with intensivist prior to transfer. 2) Floor team is responsible for stabilizing the patient and writing the transfer note. 3) If a private patient needs to go to the ICU, the private attending must page the appropriate intensivist or cardiologist. The intensivist or attending cardiologist must accept a patient before they can be transferred to the ICU. b) Transfers from MICU/CCU: 1) All patients leaving the ICU will have housestaff coverage except those private attendings who do not have housestaff privileges. ICU transfers will be accepted by the pick-up team until 3:00, and then by the long call team until 7:30pm. 2) ICU attending will notify floor attending who will then notify #580 3) Floor team responsibility: To call admitting to change attending’s name if necessary, notify attending, see the patient, and write a brief accept note. 63 of 92 10) Non-housestaff to housestaff transfers may only be accepted after evaluation for teaching value by MAR (backup) 11) Bounce Backs: If you have taken care of a patient at any time during the month, and they again require care from a medical teaching service team, they will revert to your team the following morning. An exception to this would be if another team has a low census and wishes to keep the patient. 12) ACGME Limits a) Each intern must not be assigned more than five new patients per admitting day: an additional two patients may be assigned if they are in-house transfers from the medical service. b) Each intern must not be assigned more than eight new patients in a 48 hour period. c) Each intern must not be responsible for the ongoing care of more than 10 patients. d) A supervising resident; when supervising one intern must not be responsible for the ongoing care of more than 14 patients; when supervising more than one intern must not be responsible for the ongoing care of more than 20 patients. e) The supervising resident, when supervising more than one intern, must not be responsible for the supervision or admission of more than ten new patients and four transfer patients per admitting day or more than 14 new patients in a 48 hour period. 13) Discharge Summaries: All patients discharged from a MTS service must have a discharge summary entered in QCPR by the residents. Exceptions to this are patients who are discharged with a private attending. 14) Days off: Four days off allowed per month where the resident cannot take off long call days, pick-up days, and post-call day. The chief resident needs to be notified by the floor resident at the start of the month. 15) Holidays: Only one member of the team should be present on holidays unless on long call or pick-up. Notify the chief resident at the start of each month which member of the team will be present. 16) Transitions of Care: a) In an attempt to minimize the number of transitions in patient care, to ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require residents to adhere to the following guideline regarding transitions of care b) All patients cared for by the Medical Teaching Service must have a written sign out completed using the hospital intranet system only. Signouts should be kept secure as they contain protected health information. c) Sign out should include the following: 64 of 92 a. Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b. A brief description of the reason for admission c. A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d. Any recent procedures or tests d) Sign out must be updated daily to reflect changes in the patient’s clinical course. e) Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. f) The on-call and coverage schedules for residents and attendings on teaching service are available on the hospital intranet. 3. NIGHT FLOAT SERVICE: Two week rotation consisting of one senior resident and one intern. The senior resident is assigned to admit floor patients and help the intern with cross covering duties. The intern is assigned to cross cover and help with floor admissions. a. Hours: 8pm to 8:30am Sunday through Friday Nights. Night float has Saturday night and Holidays off. b. There is a cap of seven new admissions, and two ICU transfers c. Redistribution of overnight admissions is according to night float. See pickup policy above. d. Night float will attend board review (7-7:45am) and night float rounds (88:30 am) daily. 4. BACK-UP SERVICE: a. Specific responsibilities: 1) Attend board review and other conferences 2) Back-up will act in role of MAR between 7am-3pm, and will hold 580 and receive calls on all new admissions. Will give all service and picka-doc admits to early call team. Will give private admits to other teams (except late-call) based on census. At 3pm will give 580 to late-call team. When back up is in clinic, the early call resident will serve MAR role until 3pm. 3) Cross-cover from afternoon sign-outs until night float arrives 4) Assist floor teams with procedures, admissions, etc. 5) Assist interns on days when senior residents are off as needed for guidance 6) Help the long call team with admissions from 12:00 pm– 8 pm. Back-up is only to help admitting team if there are three or more patients waiting. 7) Cross cover the housestaff patients on floors between 4:30pm8:00pm. 65 of 92 9) No Backup on weekends/holidays. B. Call Schedule There is a call schedule for each academic month that can be located on www.amion.com. The coverage schedule can be found on the Angel website. It is the resident’s responsibility to check the call schedule and to know when he/she is either on call or covering for another resident. Please leave your pager on until 8pm even when you are not on call and respond to pages from “609-497-4484”. C. Conference/Clinic Requirements Residents must attend all required educational activities of the program including noon conference, noon report, Grand Rounds, Art of Medicine, Business of Medicine, etc. promptly as per the conference schedule. All PGY-3 and PGY-2 residents on night float, floor service and MICU are strongly encouraged to attend Board Review. Residents must attend weekly continuity clinic and assigned additional clinics (except when post night float call or post-overnight call). D. Daily Schedule 1. Weekday: a. Floor service: 7:00 – 7:45 am Board Review for residents 7:00am Sign in rounds in Resident Lounge 10:45 – 11:45am Attending Rounds 12:00-1:30 pm Noon Report and Noon Conference 4:30pm (or later) Sign out to Backup Resident where all work must be done 8:00pm On call resident and backup signs out to Night Float in Resident Lounge Additional Conferences: Grand Rounds Tuesday from September to June 8:00 am, Art of Medicine/Business of medicine to be detailed in monthly schedule c. Night Float: 7:00am Board Review for residents 7:00am Sign in rounds in Resident Lounge 8:00 – 8:30 am Night Float Rounds 8:00pm Residents sign out to Night Float in Resident Lounge d. Back-up: 7:00 am Board Review 12-1:30 pm Noon Report/Noon Conference 1:30-8:00pm Follows daily coverage schedule found on white coverage sheets (MICU, Floor coverage) 4:30pm (or later) Gets sign-outs from teams 8:00pm Backup resident signs out to Night Float in Resident Lounge 66 of 92 2. Weekend/ Holiday: a. Floor service: 8:00am Sign in rounds in Resident Lounge 12:00pm (or later) Sign out to Resident holding #560 when all work is done 8:00pm (on Sundays only) sign out to Night Float Residents in Resident Lounge c. Night Float: 8:00am Saturday morning sign in rounds in Resident Lounge 8:00pm Sunday evening sign out rounds in Resident Lounge d. Backup: Off F. Beepers: • 580 - Admitting resident (floor/code beeper) • 560 - Floor cross cover (housestaff pts.)/code beeper • 510 – Chief Resident • 400 – house doc • 67 of 92 1. Weekday Schedule: Time 7am - 3pm 580 Backup Resident 560 Early call resident 3pm - 8pm Late call resident (BU resident while on-call resident at clinic) 8pm – 7am Night Float Floor resident Backup resident (Assigned intern from 12:00pm while on-call resident or back-up at clinic) Night Float intern 580 On-call resident 560 On call intern On-call resident Pick-up intern 580 On-call resident 560 On-call intern Night Float Floor resident Night Float intern 2. Saturday/Holiday Schedule: Time 8am – 8pm 8pm – 8am 3. Sunday Schedule: Time 8am – 8pm 8pm – 7am 68 of 92 Policy Name: Elective Policy Policy Number: 31 Approval by Program Leadership: 7/1/05 Amendment Date: 6/9/11 Purpose: Residency electives are designed to expose residents to different medical subspecialties and educational areas that will enhance their medical knowledge and ability to care for patients. This policy governs the activities necessary to maximize the elective experience. Policy: Expectations of a resident on elective: 1. Review pertinent elective material (schedule, goals and objectives) in the elective manual located on the residency website prior to starting the elective. 2. Demonstrate self-directed learning through independent reading about the diseases encountered during the elective. 3. Contact elective director 2-3 days prior to start of elective to confirm schedule 4. Report to the elective on time and maintain a professional demeanor at all times. 5. Attend all required educational activities of the program as per the elective schedule sheet. 6. Attend weekly continuity clinic and additional clinics as scheduled. 7. Play an active role in patient encounters. (Take a thorough history and physical exam, present case to attending, discuss management, and document appropriately in the chart.) 8.Keep personal pager on from 7am to 5pm fully charged and respond immediately to all pages in a timely manner. 9. Contact chief resident and elective director if unable to attend elective (e.g. Float day, personal day, sick day, interview, etc). Of note, any resident who wants to complete an away elective must first submit a proposal including advisor, method of evaluation, goals and objectives, activity, and hours of the week to the chief residents and Program Director for approval. The program leadership will decide whether this elective is appropriate based on previous elective activity. It is expected for the resident to attend weekly continuity clinic unless prior approval from the chief residents. 69 of 92 Policy Name: Evaluation Policy Policy Number: 32 Approval by Program Leadership: 7/1/05 Amendment Date: Purpose: Evaluations are used to assess the academic performance of residents on a continuing basis and to determine whether residents are making satisfactory academic progress. Academic matters include acquisition of knowledge related to the discipline as well as all aspects of the development of clinical and professional skills necessary for effective functioning as a health care professional. Evaluations are also used to help the residency program improve on its ability to train the residents. Policy: All residents are evaluated through a 360° evaluation process. Residents evaluate the Residency Program, hospital sites, clinic, clinical outcomes, attendings, and other residents through the E*value system. Residents will be notified through email that an evaluation is outstanding. Please complete them promptly. Residents may view their own evaluations using E*value. Residents will not be able to view their own evaluation until they have completed all outstanding E*value evaluations. For detailed information on evaluations please see the Evaluation Manual found on the residency website. 70 of 92 Policy Name: Pharmaceutical Industry Interaction Policy Policy Number: 33 Approval by Program Leadership: 7/1/05 Amendment Date: 5/25/10 Purpose: The paramount purpose of our residency is to prepare physicians for a lifetime of practice within their discipline. In the current system of healthcare, physicians will need to develop their own attitudes toward the pharmaceutical industry. Policy: We have decided to restrict interaction of residents during work hours with pharmaceutical representatives under the following conditions: 1) All materials disseminated to residents must be of an educational basis. Books, articles, reference cards, PDA software, grants and such are examples. 2) Interaction between the pharmaceutical industry and housestaff will be prohibited during duty hours. 3) All other pharmaceutical representative access must be approved by the Program Director. 71 of 92 Policy Name: Housestaff Supervision Policy Policy Number: 34 Approval by Program Leadership: 1/11/06 Amendment Date: Purpose: To ensure that residents are directly supervised by board certified physicians at all times. Policy: All medicine housestaff must be under appropriate guidance, education and direct supervision of board certified internists on all ward, critical care, ambulatory medicine and subspecialty medicine rotations. This is effected via direct communication in a timely and professional manner. When rotating through specialties outside the scope of internal medicine, residents must be supervised by board certified attending physicians practicing those specialties. Attending physicians must take primary responsibility for interfacing with the involved housestaff to comply with the educational objectives of the rotation, which include but is not limited to individual patient care management. Failure of an attending physician to comply with this policy may result in the removal of assignment of housestaff for that physician and his/her group. 72 of 92 Policy Name: Subspecialty Fellow and Internal Medicine Resident Interaction Policy Policy Number: 35 Approval by Program Leadership: 1/12/05 Amendment Date: Purpose: To delineate the responsibility of patient care between subspecialty fellows and internal medicine residents. Policy: Medicine residents are responsible for initiating and implementing diagnostic, therapeutic, dispositional and educational plans on all patients on their service, once they have discussed with the attending of record, subspecialist of record or his/her designate (i.e. fellow or nurse practitioner). Medicine resident teams are responsible for the overall day to day patient management, including all order writing. Subspecialty fellows, when involved in the case, assume supervisory responsibility as a “junior attending physician” and will be available on a daily basis to provide guidance as needed. This is to the exclusion of when a resident’s service cap is exceeded (as found in the RWJUH service policy above). In that instance, the subspecialty fellow will assume the responsibility of the day to day patient management for the number of patients that exceeds the resident’s service cap (as found in the RWJUH service policy above). Subspecialty fellows must be available for immediate consultation on any patient, when an initial consultation is requested or when a patient’s status changes. Subspecialty fellows must provide guidance for the performance of procedures, as indicated above in the procedures policy, by the medical residents. 73 of 92 Policy Name: Teaching Service Responsibilities for Medical Teaching Service (MTS), Oncology Teaching Service (OTS), Night Float, GIM Consults and Back-up at RWJUH and UMCP Policy Policy Number: 36 Approval by Program Leadership: 1/19/05 Amendment Date: 5/25/10 Purpose: To ensure that residents understand their responsibilities and expectations when on MTS, CTS, OTS, Night Float, GIM consults and Back-up at RWJUH and UMCP. Policy: A. Expectations of a PGY 1 Resident on Teaching Service: 1. Medical Knowledge a. Educate other members of the team. 1) Follow-up on assigned literature searches 2) Play a supervisory role for the third year medical students a) Teach 3rd year med students on a case by case basis b) REVIEW student progress notes WITH the student and then co-sign c) CRITICALLY evaluate and provide feedback to students on a regular basis d) Discuss differential diagnosis and disease process e) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. 2. Patient Care a. Responsible for all assigned patients. 1) Have knowledge of current medications and daily vital signs. 2) Follow up results of all labs (including trends), diagnostic tests, and consult reports. b. Perform assigned tasks with supervision from senior residents. c. Learn how to formulate a differential diagnosis d. Learn how to analyze and manage clinical problems e. Give appropriate informed consent in a manner patients understand. f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans h. Encourage participation in appropriate disease prevention or screening programs 74 of 92 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Perform full history & physical examinations on new patients and daily progress notes on assigned patients. 1) Write comprehensive, accurate and legible notes c. Dictate discharge summaries on the day of discharge if resident is in clinic or has the day off. d. Present choices and recommendations to patients in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interact with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) h. Understand your personal role within the team and interact appropriately with team members 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 1) Recognize the importance of punctuality and attention to detail c. Acts with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f.. Be eager to learn and show a willingness to learn from colleagues h. Be willing to seek advice of other residents, chief residents, program directors, department chair, attendings and regulatory authorities 5. Systems Based Practice a. Begin to understand the indications for ordering diagnostic tests and calling consults b. Learn to communicate effectively with consultants, nurses, ancillary staff, patients and family members. 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Have respect for colleagues 75 of 92 c. Understand circumstances dictating need for chaperone d. Work as a part of a team. 1) Demonstrate the ability to communicate effectively with other team members 6. Practice Based Learning and Improvement a. Learn how to critically appraise and tailor evidence to the clinical context b. Understand the role of appraisal and of assessment 1) The intern evaluates the resident using E-Value. 2). The intern evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. B. Expectations of a PGY 2 on Teaching Service: 1. Medical Knowledge a. Educate other members of the team. 1) Perform literature searches and bring pertinent articles for discussion 2) Teach practical management to interns and sub-Is 3) Play a supervisory role for the third year medical students a) Select appropriate patients for students b) Ensure that students carry 2-4 patients at ALL times c) REVIEW All student progress notes WITH the student and then co-sign d) CRITICALLY evaluate and provide feedback to students on a regular basis e) Discuss differential diagnosis and disease process f) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. c. Identify symptom patterns and the physiological basis of physical signs. d. Understand how to prioritize patients/clinical tasks and utilizing the appropriate decision making capacity in the clinical investigation and management of these tasks. 2. Patient Care a. Assume supervisory responsibility for all patients on the team (you have to know all patients on your team!). b. Effectively lead the team 1) Delegate tasks appropriately among the members of the team. 2) Organize and lead rounds effectively including work rounds WITH the intern. 3) Manage time appropriately. 4) Foster teamwork. 76 of 92 c. Identify and synthesize problems and learn how to formulate a differential diagnosis d. Analyze and manage clinical problems e. Give appropriate informed consent in a manner patients understand. f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans h. Encourage participation in a appropriate disease prevention or screening programs i. Recognize critically ill patients and when in-patient care is not required 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Write accurate, legible and meaningful notes and other documentation.. c. Dictate discharge summaries on the day of discharge. d. Present choices and recommendations to patients in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interacts with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 1) Recognizes the importance of punctuality and attention to detail c. Recognize the impact of physical problems on psychological and social well being d. Act with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f. Has realistic expectations of tasks to be completed by self and others g. Be eager to learn and show a willingness to learn from colleagues 77 of 92 h. Be willing to seek advice of chief residents, program directors, department chair and regulatory authorities 5. Systems Based Practice a. Communicate effectively with consultants, nurses, ancillary staff, patients and family members. 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Recognize the benefits of prompt communication with primary care and timely dictation 3) Have respect for colleagues b. Order diagnostic tests and consults appropriately. c. Understand circumstances dictating need for chaperone d Work as a part of a team. 1) Demonstrate ability to communicate effectively with other team members e. Identify local resources for assistance 1) Demonstrate the ability to access and refer patients to tools that aid in patient education of disease, treatment and outcomes f. Involve other health care providers as appropriate 6. Practice Based Learning and Improvement a. Actions should reflect learning from previous experiences 1) Tailor evidence to the clinical context 2) Critical appraisal of evidence b. Understands the role of appraisal and of assessment 1) The resident evaluates the intern using E-Value. 2). The resident evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. C. Expectations of a PGY 3 on Teaching Service: 1. Medical Knowledge a. Educate other members of the team. 1) Perform literature searches and bring pertinent articles for discussion 2) Teach practical management to interns and sub-Is 3) Play a supervisory role for the third year medical students a) Select appropriate patients for students b) Ensure that students carry 2-4 patients at ALL times c) REVIEW All student progress notes WITH the student and then cosign d) CRITICALLY evaluate and provide feedback to students on a regular basis e) Discuss differential diagnosis and disease process 78 of 92 f) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. c. Identify symptom patterns and the physiological basis of physical signs. d. Understand how to prioritize patients/clinical tasks and utilizing the appropriate decision making capacity in the clinical investigation and management of these tasks. 2. Patient Care a. Assume supervisory responsibility for all patients on the team (you have to know all patients on your team!). b. Effectively lead the team 1) Delegate tasks appropriately among the members of the team. 2) Organize and lead rounds effectively including work rounds WITH the intern. 3) Manage time appropriately. 4) Foster teamwork. c. Identify and synthesize problems and learn how to formulate a differential diagnosis d. Analyze and manage clinical problems e. Give appropriate informed consent in a manner patients understand. f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans h. Encourage participation in a appropriate disease prevention or screening programs i. Recognize critically ill patients and when in-patient care is not required 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Write accurate, legible and meaningful notes and other documentation.. c. Dictate discharge summaries on the day of discharge. d. Present choices and recommendations to patients in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interacts with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) 79 of 92 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 1) Recognizes the importance of punctuality and attention to detail c. Recognize the impact of physical problems on psychological and social well being d. Act with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f. Has realistic expectations of tasks to be completed by self and others g. Be eager to learn and show a willingness to learn from colleagues h. Be willing to seek advice of chief residents, program directors, department chair and regulatory authorities 5. Systems Based Practice a. Communicate effectively with consultants, nurses, ancillary staff, patients and family members. 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Recognize the benefits of prompt communication with primary care and timely dictation 3) Have respect for colleagues b. Order diagnostic tests and consults appropriately. c. Understand circumstances dictating need for chaperone d Work as a part of a team. 1) Demonstrate ability to communicate effectively with other team members e. Identify local resources for assistance 1) Demonstrate the ability to access and refer patients to tools that aid in patient education of disease, treatment and outcomes f. Involve other health care providers as appropriate 6. Practice Based Learning and Improvement a. Actions should reflect learning from previous experiences 1) Tailor evidence to the clinical context 2) Critical appraisal of evidence b. Understands the role of appraisal and of assessment 1) The resident evaluates the intern using E-Value. 2). The resident evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 80 of 92 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. 81 of 92 Policy Name: Teaching Service Responsibilities for Medical Intensive Care Unit Service (ICU) at RWJUH Policy Policy Number: 37 Approval by Program Leadership: 1/19/05 Amendment Date: 5/25/10 Purpose: To ensure that residents understand their responsibilities and expectations when on ICU at RWJUH. Policy: A. Expectations of a PGY-1 on ICU Teaching Service 1. Medical Knowledge a. Educate other members of the team. 1) Follow-up on assigned literature searches 2) Play a supervisory role for the third year medical students a) Teach 3rd year med students on a case by case basis b) REVIEW student progress notes WITH the student and then co-sign c) CRITICALLY evaluate and provide feedback to students on a regular basis d) Discuss differential diagnosis and disease process e) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. c. Adhere to ICU rounding and conference schedule. d. Review with attending, fellow and residents all deaths that occur during the month. e. To learn the basic tenets of stabilization of critically ill patients. f. To become proficient in various procedures, particularly central line placement and ACLS 2. Patient Care a. Responsible for all assigned patients. 1) Have knowledge of current medications and daily vital signs. 2) Follow up results of all labs (including trends), diagnostic tests, and consult reports. b. Perform assigned tasks and procedures with supervision from senior residents, fellows and intensivists. c. Learn how to formulate a differential diagnosis d. Learn how to analyze and manage clinical problems 1) To recognize changes in clinical status of patients from stable to unstable and vice-versa e. Give appropriate informed consent in a manner patients understand. 82 of 92 f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Perform full history & physical examinations on new patients and daily progress notes on assigned patients. 1) Write comprehensive, accurate and legible notes c. Dictate discharge summaries on the day of discharge if resident is in clinic or has the day off. d. Present choices and recommendations to patients and families in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s and family’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interact with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) h. Understand your personal role within the team and interact appropriately with team members 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 1) Recognize the importance of punctuality and attention to detail c. Act with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f. Be eager to learn and show a willingness to learn from colleagues h. Be willing to seek advice of other residents, chief residents, program directors, department chair, attendings and regulatory authorities 5. Systems Based Practice a. Begin to understand the indications for ordering diagnostic tests and calling consults 83 of 92 b. Learn to communicate effectively with consultants, nurses, ancillary staff, patients and family members. 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Have respect for colleagues 3) To learn to work within a multidisciplinary team to provide care to a critically ill patient. c. Understand circumstances dictating a need for a chaperone d. Work as a part of a team. 1) Demonstrate the ability to communicate effectively with other team members 6. Practice Based Learning and Improvement a. Learn how to critically appraise and tailor evidence to the clinical context b. Understand the role of appraisal and of assessment 1) The intern evaluates the resident using E-Value. 2). The intern evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. B. Expectations of a PGY 2 on ICU Teaching Service: 1. Medical Knowledge a. Educate other members of the team. 1) Perform literature searches and bring pertinent articles for discussion 2) Teach practical management to interns and sub-Is 3) Play a supervisory role for the third year medical students a) Select appropriate patients for students b) Ensure that students carry 2-4 patients at ALL times c) REVIEW All student progress notes WITH the student and then co-sign d) CRITICALLY evaluate and provide feedback to students on a regular basis e) Discuss differential diagnosis and disease process f) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. c. Identify symptom patterns and the physiological basis of physical signs. d. Understand how to prioritize patients/clinical tasks and utilizing the appropriate decision making capacity in the clinical investigation and management of these tasks. e. Adhere to ICU rounding and conference schedule. f. Review all deaths that occur during the month. g. To recognize changes in clinical status of patients from stable to unstable and vice-versa. 84 of 92 h. To expose residents to patients with unstable, life-threatening medical illnesses. i. To learn the basic tenets of stabilization of critically ill patients j. To become proficient in various procedures, particularly central line placement and ACLS. 2. Patient Care a. Assume supervisory responsibility for all patients on the team (you have to know all patients on your team!). b. Effectively lead the team 1) Delegate tasks appropriately among the members of the team. 2) Organize and lead rounds effectively including work rounds WITH the intern. 3) Manage time appropriately. 4) Foster teamwork. c. Identify and synthesize problems and learn how to formulate a differential diagnosis d. Analyze and manage clinical problems e. Give appropriate informed consent in a manner patients understand. f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans h. Recognize critically ill patients and when in-patient care is not required 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Write accurate, legible and meaningful notes and other documentation.. c. Dictate discharge summaries on the day of discharge. d. Present choices and recommendations to patients in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interacts with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 85 of 92 1) Recognizes the importance of punctuality and attention to detail c. Recognize the impact of physical problems on psychological and social well being d. Act with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f. Has realistic expectations of tasks to be completed by self and others g. Be eager to learn and show a willingness to learn from colleagues h. Be willing to seek advice of chief residents, program directors, department chair and regulatory authorities 5. Systems Based Practice a. Communicate effectively with consultants, nurses, ancillary staff, patients and family members. 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Recognize the benefits of prompt communication with primary care and timely dictation 3) Have respect for colleagues 4) To learn to work within a multidisciplinary team to provide care to a critically ill patient. b. Order diagnostic tests and consults appropriately. c. Understand circumstances dictating need for chaperone d. Work as a part of a team. 1) Demonstrate ability to communicate effectively with other team members e. Identify local resources for assistance 1) Demonstrate the ability to access and refer patients to tools that aid in patient education of disease, treatment and outcomes f. Involve other health care providers as appropriate 6. Practice Based Learning and Improvement a. Actions should reflect learning from previous experiences 1) Tailor evidence to the clinical context 2) Critical appraisal of evidence b. Understands the role of appraisal and of assessment 1) The resident evaluates the intern using E-Value. 2). The resident evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. 86 of 92 C. Expectations of a PGY 3 on ICU Teaching Service: 1. Medical Knowledge a. Educate other members of the team. 1) Perform literature searches and bring pertinent articles for discussion 2) Teach practical management to interns and sub-Is 3) Play a supervisory role for the third year medical students a) Select appropriate patients for students b) Ensure that students carry 2-4 patients at ALL times c) REVIEW All student progress notes WITH the student and then cosign d) CRITICALLY evaluate and provide feedback to students on a regular basis e) Discuss differential diagnosis and disease process f) PLEASE contact Dr. Kim or Dr. Walker with any questions/problems regarding students b. Demonstrate enthusiasm for learning through independent reading. c. Identify symptom patterns and the physiological basis of physical signs. d. Understand how to prioritize patients/clinical tasks and utilizing the appropriate decision making capacity in the clinical investigation and management of these tasks. e. Adhere to ICU rounding and conference schedule. f. Review all deaths that occur during the month. g. To recognize changes in clinical status of patients from stable to unstable and vice-versa. h. To expose residents to patients with unstable, life-threatening medical illnesses. i. To learn the basic tenets of stabilization of critically ill patients j. To become proficient in various procedures, particularly central line placement and ACLS. 2. Patient Care a. Assume supervisory responsibility for all patients on the team (you have to know all patients on your team!). b. Effectively lead the team 1) Delegate tasks appropriately among the members of the team. 2) Organize and lead rounds effectively including work rounds WITH the intern. 3) Manage time appropriately. 4) Foster teamwork. c. Identify and synthesize problems and learn how to formulate a differential diagnosis d. Analyze and manage clinical problems e. Give appropriate informed consent in a manner patients understand. 87 of 92 f. Ensure satisfactory completion of reasonable tasks at the end of the shift/day with appropriate signouts and transfer of care. g. Involve patients in developing mutually acceptable investigation and treatment plans h. Recognize critically ill patients and when in-patient care is not required 3. Interpersonal and Communication Skills a. Relay organized oral case presentations. b. Write accurate, legible and meaningful notes and other documentation.. c. Dictate discharge summaries on the day of discharge. d. Present choices and recommendations to patients in an appropriate manner to ensure informed consent 1) Avoid jargon and use familiar language 2) Use interpreters appropriately 3) Give clear information and feedback to patients and share information with relatives when appropriate 4) Importance of patient confidentiality 5) Respect the patient’s choice(s) and wish(es) 6) Act with empathy and sensitivity e. Deal with dissatisfied and difficult patients/relatives f. Effectively interacts with health care providers in the care of each patient g. Hand over the care of the patient safely (signouts) 4. Professionalism a. Answer pages in a timely fashion. b. Maintain a professional demeanor at all times. 1) Recognizes the importance of punctuality and attention to detail c. Recognize the impact of physical problems on psychological and social well being d. Act with empathy, honesty and sensitivity towards the patient 1) Maintain awareness of patient dignity, confidentiality and cultural/ethnic issues 2) Recognize the importance of: involving patients in decisions, offering choices and respecting patient’s views 3) Adopt a non-discriminatory attitude to all patients and recognizes the patient’s needs as an individual e. Demonstrate timely documentation and chart completion f. Has realistic expectations of tasks to be completed by self and others g. Be eager to learn and show a willingness to learn from colleagues h. Be willing to seek advice of chief residents, program directors, department chair and regulatory authorities 5. Systems Based Practice a. Communicate effectively with consultants, nurses, ancillary staff, patients and family members. 88 of 92 1) Ensure that notes are accessible to all members of the team and patients under certain circumstances 2) Recognize the benefits of prompt communication with primary care and timely dictation 3) Have respect for colleagues 4) To learn to work within a multidisciplinary team to provide care to a critically ill patient. b. Order diagnostic tests and consults appropriately. c. Understand circumstances dictating need for chaperone d. Work as a part of a team. 1) Demonstrate ability to communicate effectively with other team members e. Identify local resources for assistance 1) Demonstrate the ability to access and refer patients to tools that aid in patient education of disease, treatment and outcomes f. Involve other health care providers as appropriate 6. Practice Based Learning and Improvement a. Actions should reflect learning from previous experiences 1) Tailor evidence to the clinical context 2) Critical appraisal of evidence b. Understands the role of appraisal and of assessment 1) The resident evaluates the intern using E-Value. 2). The resident evaluates the attending, using E-Value, on the basis of teaching interest and effectiveness, medical knowledge, physical exam teaching skills, emphasis on cost-effectiveness, and degree of availability. 3) Demonstrate improvement using feedback c. Random chart audits and mini-CEXs will be performed. 89 of 92 Policy Name: Academic Travel Process Policy Policy Number: 38 Approval by Program Leadership: 6/1/07 Purpose: This policy addresses the process each resident must follow prior to traveling to a regional or national conference. Policy: The following steps must be taken before attending an academic conference at which a resident is presenting: 1. Prior to accepting an invitation to present at an academic conference, the resident must obtain approval by Dr. Sharma. 2. 8-10 weeks prior to travel, the resident needs to fill out the Travel Approval form and return it to Kim Inzano. Along with the form, all documentation for the trip should be provided including the conference itinerary, title of resident’s presentation, hotel arrangements and flight plans. The approval form can be obtained from Kim in the Residency Office (phone# 732-2357742, fax#732-235-7427) 3. The Residency Office will forward the approval form along with supporting documents to Jean Feeney in the Ethics Office. The Ethics Office generally takes about 4 weeks to give approval. 4. Once approval is obtained, Kim Inzano will notify the resident. At which time, the resident must fill out the Travel Advance form and submit it to Kim along with any other supporting documents needed. On this form, question #3, asking if the resident will be staying at the conference designated hotel, must be checked yes or no. If yes, the university will pay for the cost of the hotel. If no, the university will only pay $100 per diem. If the resident is not staying at the conference designated hotel and the cost will be more than $100/day, he or she must send a memo to Dr. Kostis at the time of filling out this form stating the cost and the justification for staying at the non-conference designated hotel. For question #4, the resident should enter the university allowance for meals which is equivalent to $45/day. Again, if anything more than that amount is entered, a memo must be sent to Dr. Kostis with justification for the amount entered. 5. If the above timeline is followed properly, a check will be issued for up to 90% of the projected cost of the trip prior to travel. The remaining 10% will be reimbursed upon the resident’s return. 6. If there is a delay in approval, a check advance will not be issued. Instead, the resident will be reimbursed upon his or her return. 7. After returning, the resident must fill out a travel expense report detailing all expenses for which he or she would like to be reimbursed. All receipts must accompany this form. 90 of 92 For a more detailed explanation of the university policy please click the link below: http://www.umdnj.edu/oppmweb/Policies/HTML/financial/00-01-50-10_00.html Expenses will not be reimbursed if you fail to comply with the university policies. Policy Name: Transitions of Care Policy Number: 39 Approval by Program Leadership: 05/17/2012 Amendment Date: n/a Purpose: To ensure and monitor effective, structured handover processes to facilitate both continuity of care and patient safety, and to ensure that residents are competent in communicating with team members in the handover process, we require residents to adhere to the following guidelines regarding transitions of care: Policy: Transitions of Care: 1) In an attempt to minimize the number of transitions in patient care, the residency program has a structured nightfloat (general medical floors) and night shift (Intensive Care Units) system. 2) All patients cared for by the Medical Teaching Service must have a written sign out completed using the hospital intranet system only. Signouts should be kept secure as they contain protected health information. 3) Sign out should include the following: a) Patient name, attending physician, consultants, drug allergies/adverse reactions and code status. b) A brief description of the reason for admission c) A list of active problems and the treatment plan, as well as any anticipated issues and possible solutions d) Any recent procedures or tests 4) Sign out must be updated on a daily basis to reflect changes in the patient’s clinical course. 5) Transitions of care must be done face-to-face between the outgoing and incoming resident in compliance with all HIPAA regulations. 6) All interns will be introduced to the process of signouts during the Clinical Skills Initiative rotation in July-August of the academic year with periodic overviews during monthly orientation. 7) To assess competency in communication related to transitions of care, sign out “mini CEX’s” will be performed by the senior resident or attending at random and feedback provided. 8) The on-call and coverage schedule for residents and attendings is available on the hospital intranet. 91 of 92 92 of 92