De-Novo Malignancies Post Heart Transplantation
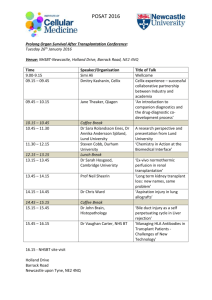
advertisement

De-Novo Malignancies Post Heart Transplantation: A Review of the Literature on the Mechanisms, Types, and Causes of the Malignancies. William Evans* and Anthony Kodzo-Grey Venyo*^ North Manchester General Hospital Department of Urology Manchester United Kingdom Correspondence to: Mr Anthony Kodzo-Grey Venyo MB ChB FRCS(Ed) FRCSI FGCS Urol LLM North Manchester General Hospital Department of Urology Manchester United Kingdom ABSTRACT Background: Heart transplantation is a gold standard treatment for patients with endstage heart disease. With the use of potent immunosuppressive agents and effective post-transplant management of heart transplant recipients, the survival rate of the patients and graft survival have significantly improved. One of the identified complications of heart transplantation is the development of post-transplant malignancy. Objective: To review the literature on De Novo malignancies which develop in heart transplant recipients following cardiac-transplantation. Results: The reported incidence of malignancy following heart transplantation varies hugely between studies. There are conflicting findings with regard to the commonest type of malignancy. Cancers in HT recipients also have slightly differing characteristics compared to their equivalents in the general population. Namely, they have a preponderance for extralymphatic sites in PTLD and aggressive nature (SCC). Reported incidence of malignancy following HT varies hugely between studies. There are conflicting findings with regard to the commonest type of malignancy. Some authors estimated that skin cancers were the commonest type followed by PTLD. However, a small study by other authors found PTLD to be most common. Aetiological causes for malignancy seem strongly dependent on the side effects of immunosuppressives which likely act to inhibit the immune system’s response to earlier malignant changes in cells. Viruses such as HPV, EBV, and HHV-8, play an important role in the development of cancer in HT recipients. The mechanisms by which HPV and EBV induce the proliferation of cells are comparatively well understood compared to HHV-8. However, the role of immunosuppressives in this process is not well understood but there is some evidence that withdrawal of immune therapy can induce remission of KS implying that the drugs play a pivotal role. In Kaposis sarcoma Human Herpes Virus - 8 is reported to play an important role in the immunosuppressed state. The review discussed the limited evidence which suggests a role for CD8 T-cells and CD-4 regulatory T-cells in this process. Conclusions: Types of cancers that have been reported following heart transplantation include: cancers of the skin and these cancers tend to be more aggressive tumours; blood borne cancers; lymphoproliferative disorders; kaposis sarcoma. Viruses such as HPV and HHV-8 play an important role in the development of cancer in Heart transplant recipients. The mechanisms by which HPV and EBV induce the proliferation of cells is comparatively well understood compared to HHV-8. However, the role of immunosuppressives in this process is not well understood. There is some evidence that withdrawal of immune therapy can induce remission of KS implying that the drugs play a pivotal role. Much further work is needed in understanding the immune systems role in neoplasia, the role of the cancer causing viruses mentioned and the development newer immunosuppressive therapies. Key Words: Heart-Transplantation; immunosuppression; skin cancers; lymphoproliferative disorders; kaposis sarcoma; squamous cell carcinoma. INTRODUCTION Recipients of organ transplants are more likely to develop malignancies than age matched controls in the general population. However, this is attributed to a higher number of certain, specific malignancies, as opposed to the common cancers (lung, breast, prostate, colon and invasive uterine cervical carcinomas) [1]. This review focuses mainly on the studies related specifically to heart transplant recipients, drawing upon some evidence from the better understood transplant procedures, in particular kidney. A number of worldwide records such as the Israel Penn international tumour transplant registry (IPITTR), Spanish National transplant Organization (ONT) and the Australia and New Zealand Dialysis and Transplant registry (ANZDATA) currently record incidence of various complications following these procedures including those of ensuing malignacies. As with the other major solid organ transplants a number of factors are related to the development of neoplasias following heart-transplantation (HT). Penn et al [1-7] estimated from the IPITTR that skin cancers accounted for 40% of all tumours following organ transplantation, the percentages of other malignancies found were as follows: lymphatic cancers 11%, Kaposis sarcoma (KS), kidney and cervix 4% each, vulva and perineum 3% each. In heart transplant recipients the three most prevalent cancers are believed to be skin tumours, lymphoproliferative disorders and KS. Other less common forms reported malignancies being uterine, cervix, vulva, scrotum, colon, stomach, kidney and biliary tract [8]. This review mainly focuses on the 3 most prevalent types. LITERATURE REVIEW Aetiology (Mechanism, Types, and Causes) Mechanisms of cancer formation: role of immunosuppressive therapy The reasons for the increased risk of malignancies developing after heart-transplantation are complex and unclear but broadly speaking immunosuppression is believed to be largely responsible. Improvements in transplant techniques and longer life expectancy have increased exposure to immunosuppressive drugs. Early drug therapies began with corticosteroids, azathioprine, anti-thymocyte globulin, anti-lymphocyte globulin and then more latterly calcineurin inhibitors such as ciclosporin. These now extend to newer mono clonal antibodies such as basiliximab and daclizumab. These agents are frequently used in combination but no one drug or class of drugs have been linked more strongly to tumour growth. For instance it has been shown in two studies [9], [10] that there is little difference between tumour rate and type in patients treated with cyclosporin and those treated with tacrolimus based regimes. Nor is there considerable difference between those who received azathioprine compared to cyclosporine based regimes [11]. However, one study did find a significantly lower rate of malignancy in mammalian target of rapamycin (mTOR) inhibitor-based immunosuppressive protocols [12]. There is much debate concerning carcinogenesis in the immunosuppressed, some of which centres around other immuno-depleted states such as severe HIV/AIDS. A coherent theory of cancer immunosurveilance was first proposed by Burnet and Thomas [13] as a concept of immunological control and then developed further as they began to address the question of why transplant recipients were more prone to cancer [14], [15]. However, it was earlier still in 1909 that a concept of the immune system looking for and irradicating errant, malignant cells was suggested [16]. Despite widespread criticism, the immunosurveilance theory was largely supported by two subsequent mouse model studies [17], [18]. In 1971 Burnet et al. [14] went further still suggesting sentinel thymus dependant cells as the critical mechanism. However, it was felt that this was an oversimplification of the immune system’s role and within the last 10 years was incorporated into a newer ‘immunoediting hypothesis’ [19], [20]. This newer model consists of three states ‘Elimination’, Equilibrium’ and ‘Escape’. Elimination includes the original concept of immunosurveilance but now accepts that both innate and adaptive lymphocytes have a role to play in this process. Dunn et al [21] explained how the immune system responds to ‘danger signals’, chemicals such as interferon-γ (IFN- γ) and perforin which are released by cells undergoing tumorigenesis. Studies in mouse models have supported this. Specific gene knockouts responsible for immune complexes thought to be involved in immunosurveilance, such as recombinant activating gene 2 (RAG-2) have been shown to greatly increase frequency of tumours [22]. Studies have identified specific cells responsible for immunosurveillance. These include natural killer and natural killer T cells [23, 24, 25] and γδ T cells, αβ T cells [26], [27], [28]. Following on from this process, equilibrium is defined by Dunn et al [19] as a state in which tumour growth is restricted in a balance between tumour growth and immune response. Escape is when the growth finally evades this restriction. The main mechanism by which the common immunosuppressant drugs work is by inhibiting T cell activity. Corticosteroids have a broad range of actions. They inhibit macrophage and monocyte function and have anti-inflammatory effects. They also activate cytoplasmic gluco-corticoid receptors which inhibit the transcription of genes. This affects both the production and function of lymphocytes and reduces the production of cytokines such as IL1, IL-2, IL-6, IFN- γ and TNF-α [29]. Calcineurin inhibitors work slightly differently but on many of the same cytokines. Their mechanisms are well outlined by Shibasaki et al. [30]. Ordinarily T cell activation following binding to transplanted organs cell surface proteins triggers a calcium dependant intracellular signalling mechanism that activates calcineurin, a calcium/calmodulindependent phosphatase (PP2B). Calcineurin dephosphorylates ‘Nuclear factor of activated T-cells cytoplasmic 1’ (NFATC1). This allows translocation into the nucleus where it causes transcription factors to bind and synthesise cytokines. Calcineurin inhibitors bind proteins involved in translocation, FKBP5 (tacrolimus) and cyclophilin (cyclosporine). This prevents synthesis of IL-1, IL-2, IL-6, IFN- γ and TNF-α that would normally occur. Like Tacrolimus mTOR inhibitors also target FKBP5 but do not work by calcineurin inhibition. mTOR is a serine/threonine protein kinase which controls multiple downstream pathways responsible for synthesis of a number of various proteins [31]. Critically here it inhibits protein kinase B which prevents progression of the cell cycle in T cells. The one factor that many of the immunosuppressive drugs have in common is that they inhibit IL-2. This cytokine is itself the target of mono-clonal antibody preperations. The drugs basiliximab and daclizumab bind the alpha chain of IL-2 on activated T-cells [32], [33]. IL-2 is normally released by the T-cells to facilitate the growth and differentiation of cytotoxic Tcells [34], [35]. At the same time IL-2 receptors are upregulated. The interaction between the two leads to the production a proliferation of antigen specific clones, once a critical number of receptors have been activated [36], [37]. IL-2 can also cause B-cells to release immunoglobulins and encourage production and differentiation of natural killer cells [38]. Although there is evidence that cancer risk is greatly increased by immunosuppressive therapy in the absence of viruses, these pathogens behave opportunistically during immunosupression and enhance malignancy risk further. The roles of different viruses vary greatly between cancer types. However, the most common cancers post transplantation are those thought to be caused by viruses [39]. Cancers of the skin The frequency of all skin cancers particularly Squamous cell carcinomas is increased in those receiving any form of transplant [40]. The IPITTR and the subsequent findings of Penn et al. [2], [3], [4], [5] found that in the general population basal cell carcinomas (BCC) are five times more common than squamous cell carcinoma (SCC). In transplant patients the proportion of SCC is greater than BCC [41], [42], [43] and the growth is 40-250 times more common than in the general population despite BCC itself being ten times more common [44]. The risk of malignant melanoma is 5 times higher.[45] Prevalence is high in HT recipients in particular with one follow-up study reporting that 46.4% of patients had some form of skin cancer 15 years after procedure [46]. Euvrard et al. [47] compared the rates of malignant and premalignant epithelial tumours in heart and renal transplant patients and found that rates in HT were twofold greater. Post-transplant cancers tend to be more aggressive and present sooner in a patient’s lifetime. The CTTR found that nearly 6% of skin cancers in transplant patients had metastasised to a lymph node. Of these 17% were from malignant melanomas and 73% from SCCs [2], [3], [4], [5], [7]. Ultra-violet (UV) light is well known to be carcinogenic to skin in the absence of immunosuppressives. It is thought that UV light also plays an additional, localised immunosuppressive role reducing the number of the dendritic Langerhans cells in the epidermis which present antigen and control proliferation of human papillomavirus (HPV). Mechanisms of carcinogenesis surrounding HPV are not well understood due to the fact they are endemic in many without causing cancer. Despite this the E6 and E7 oncogenes have been identified as capable of binding to and having a direct inhibitory effect on the cell cycle regulators p53 and Rb respectively [48] Warts secondary to HPV have been found in a number of studies to be linked to and likely develop into SCC [3], [5], [7], [49], [50]. Particularly HPV types 5 and 8 which were found by Stockfleth et al. to increase the risk of SCC development [51].The study did however find that in a group of specimens with BCC there was not a significantly increased prevalence of HPV DNA between those who had received organ transplants and those who were not immunosuppressed (50% vs 48%). Macgregor et al [52]found that sunlight played a critical role in the development of skin cancers in transplant patients independent of HPV with 75 % of gene mutations in nonmelanoma skin cancers in this group showing damage consistent of UV irradiation. They did however find no relationship between HPV status and presence of p53 mutation. Certain Human leukocyte antigen types have been shown to play a protective role against viral and non viral induced tumours. It is has been observed in the past that HLA mismatching in renal transplant recipients increases risk of SCC, independent of the higher levels of immunosuppressive therapy required [53]. A study specifically on Australian heart transplant recipients found that HLA-DR7 was a protective factor whereas HLA-DR homozygosity was associated with skin cancer overall. HLA-A1 and HLA-A11 were protective in the development of bowens disease. Studies in non cardiac transplant patients have implicated HLA- B27 and HLA-DR7 as increasing the risk of skin cancers yet HLA-A11 was found to be protective [54]. Blood borne cancers: post transplant lymphoproliferative disorders Lymphoid neoplasia following solid organ and allogenic bone transplant are categorised as post transplant lymphoproliferative disorder (PTLD). This is an umbrella term for a broad range of subtype diseases. Much debate has been focussed on the exact classification of PTLD but the most commonly used system is that of the world health organisation (WHO) divides it into 3 categories [55]. The three categories include early lesions, polymorphic PTLD and monomorphic PTLD. Early lesions tend to be more benign typically exhibiting plasmacytic hyperplasia. Polymorphic PTLD can be further categorised into polyclonal and monoclonal most of which is B cell in origin and most commonly includes large B-cell lymphoma but can extend to Burkitts and Burkitts type lymphoma and plasma cell myeloma (56). Monomorphic types are histologically the same as one of the major types of lymphoma usually non-hodgkins lymphoma of B-cell origin [55]. Compared to lymphomas in non-transplant recipients PTLDs are more aggressive less responsive to therapy and more likely to invade extra-nodal tissue [57], [58], [59], [60]. Analysis of IPITTR results found that 53% of PTLDs involved multiple organs or sites [3], [ 4], [5]. Epstein Barr virus (EBV) plays a significant role in the development of PTLDs and approximately 90-95% of PTLDs have been found to contain traces of the virus [61],[ 62]. PTLD is the most common form of post transplant malignancy in children [63], [64], [65], [66]. This is thought to be due to their lower chance of being exposed to EBV over time and subsequent immune naivety compared to their adult counterparts. [56] Another major factor is if the host is EBV sero-negative and receives a graft from a seropositive donor [67], [68]. EBV, a member of the herpes family infects and immortalises Bcells. Infection in the immune-competent individual precipitates a response in T-cells which controls the proliferation of the infected B-cells. The EBV genome then lies dormant in these stable cells. Furthermore EBV associated genes such as LMP1 and LMP2BCRF 1 and BARF 1 proteins allow infected cells to avoid immune detection and apoptosis [69]. Therefore the EBV seronegative host will also receive some infected B-cells present in the graft. Where the T-cell control is absent or inhibited hyperplasia or malignancy can then occur. For instance if a host is exposed to high levels of immunosuppression then this can suppress the CD8 cytotoxic T-cell function hence treatment for PTLD usually involves withdrawal/reduction of immunotherapy. Alternatively if an individual develops a primary EBV infection post transplant they may be unable to mount a full immune response. Younger age and presence of cytomegalovirus have also been identified as risk factors [70]. With regard to the presentations of PTLD post cardiac transplant there is comparatively little literature. Common tissues affected in paediatric HT recipients have been sited as gastrointestinal tract and respiratory system along with cervical lymph nodes [7]. Penn highlights [1] that although in the general population lymphoma is frequently confined to the lymph nodes, it was found in the IPITTR and further work [3], [ 4], [ 5], [7], [72], [73], [74] that in 70% of cases . Post-transplantation lymphoproliferative disorders ( PTLD) occurred in extra-nodal sites, namely: liver (25%), lungs (21%), CNS (21%), intestines (19%), kidneys (18%) and spleen (12%). The author also mentions how PTLD was found to be more common in heart and lung transplant recipients compared to renal as withdrawal of immunotherapy and resumption of dialysis is an option. With heart and lung transplants more intensive immunosuppressive therapies were often required and could not be withdrawn. Kaposis sarcoma (KS) KS is a tumour better known in HIV/AIDS caused by human herpes virus 8 (HHV8) which is also associated with the lymphoproliferative disorders multicentric Castleman's disease and primary effusion lymphoma. It is a systemic disease which can remain as cutaneous lesions or spread internally and is thought to originate from lymphatic endothelial cells which form distinctive ‘spindle cells’. There are 4 main types of the disease: that in iatrogenically immunosuppressed patients, AIDS-related KS, Classic KS in men of jewish/mediteranean descent and African endemic KS. The disease was found to affect 0.52% of European organ transplant recipients in a French study of 7923 patients [39]. With prevalence of KS following heart transplant (0.41%) being the third highest after liver (1.24%) and kidney (0.45%). Like HPV, HHV-8 is a member of the herpesviridae family and as such can exist in either a latent or lytic reactivation state. The initial innate response to infection is initiated by cytokines released from infected host cells however in KS deregulation of genes involved in this pathway lead to a dysfunctional response [75], [76], [77]. The type I IFN group of cytokines, are examples of cytokines involved in such a reaction to viral infection. HHV affects the IFN-regulatory factor (IRF) family of transcription factors which bind relevant DNA and promote synthesis of type I IFN and related components. HHV encodes 4 genes homologous to IRFs which are responsive to viruses [78, 79] thus helping to evade the immune response. The virus infects and causes proliferation of endothelial and B-lymphocyte cells. As well as the above traits, HHV-8 encodes genes homologous to those found in the host cell which are responsible for cellular replication, inflammation and angiogenesis [80]. The immune response to HHV-8 in preventing KS in the healthy individual is poorly understood. It is thought to involve HHV-8 specific CD-8 T-cells and CD-4 regulatory T-cells [81], [82]. The exact mechanism by which immunosuppressive drugs potentiate the replication of HHV-8 and KS is similarly unclear but it is thought to involve an interaction at this level. This is supported by the fact that for PTLD the withdrawal of immunosuppressives is the usual treatment. With regard to the distribution of KS in transplant patients on the IPITTR, Penn found [83, 84] that 60% had non visceral disease (of these 98% were skin lesions and 2% mouth/oropharygeal) and that 40% had visceral disease (27% of which had no skin involvement). Visceral involvement, mostly affected mainly GI tract, lungs and lymph nodes. In fact KS is named after Moritz Kaposi who first observed the death of a man with multiple pigmented skin lesions from GI bleeding. Autopsy found multiple lesions in the GI tract and lungs. Here time of onset from lesions to death was 15 months. In transplant recipients [85] average time from transplant to development of KS is 15-30 months [86]. One study found that of 1425 patients who underwent kidney transplants 16 developed KS [87]. Of these 16, 5 had involvement of the GI tract as well as skin lesions and 4 had disseminated disease. Despite encouraging results for immunosuppression withdrawal and chemotherapy in cutaneous KS the authors maintain that prognosis remains poor if visceral disease occurs [87]. Within the GI tract KS has been reported within the mesentery [88], appendix [89] and rectum [90]. A number of case studies have observed the metastasis of disseminated KS into the central nervous system [91]. DISCUSSION Significant Studies looking at prevalence of malignancies and their outcome following various therapies have been undertaken specifically in HT patients. These give us accurate insight into prevalence of neoplasia that may be unique to this procedure and the efficacy of drugs and regimes in preventing these growths. Chen PL et al [92] looked at 78 post HT patients who had received standard calcineurin inhibitor based triple therapy. They found that 8 patients developed neoplasia after HT, (6 adults, 2 children) and that 4 of these were in the first year. They found PTLD to be the most common malignancy and that it was positively associated with younger age. The 2 children who had malignancy had PTLD, both developed the disease within 1 year of procedure. They found only 1 incident of skin cancer (SCC) which they attributed to the ethnicity of their sample. A large Spanish study [93] of 3393 HT patients found that 50% of cancers post transplant affected the skin but that these had a generally high 5 year survival rate of 74%. 10% of cancers were lymphomas and these had a much poorer prognosis (20% 5 year survival). They noted considerable success in the treatment of skin cancers if mycophenolate mofetil was given within 3 months of procedure, independent of a number of factors such as prior smoking status, treatment with tacrolimus, age and sex. Prophylactic use of acyclovir was also found to be highly effective, halving the risk of lymphoma independent of other therapies. A smaller study [94] of 211 HT recipients found an overall incidence of malignancy of 30.8%. Interestingly they did find that significantly fewer malignancies occurred in patients receiving an mTOR-inhibitor (P < .0001). In patients who had developed visceral neoplasia withdrawal of calcineurin inhibitors improved prognosis. Independent risk factors for neoplasia were ischemic cardiomyopathy prior to HT, increasing age at time of procedure and gender (males). Roithmaier et al [95] looked at 907 heart-lung transplant recipients and compared the prevalences of cancer post operatively to those in the general population of the same region. They found PTLD to be the most common with a 26.2 fold increased risk in transplant recipients. This was followed by head and neck cancers (21.0 fold increase) then lung cancer (9.3 fold increase). They found that 424 of the recipients died with median survival post transplantation of 8.6 years. They found a greater proportion of those who died were male (67% compared to 33% female). A study of 474 patients [96] who had received triple immunosuppression with cyclosporin A, azathioprine, steroids and prophylactic antilymphocyte therapy following HT found that 55 (11.6%) developed neoplasia. 55% were solid tumours (of these 39% affected the lung), 20% Non-hodgkins lymphoma, 11% KS , skin 9%, sarcomas/myelomas (undifferentiated) 5%. KS was the most rapid onset malignancy post procedure (12.7±16.8 months). Again age at time of transplantation was positively associated with risk of neoplasia as was azathioprine dose, however number of previous rejections, dosing of cyclosporine and prednisolone were not. The group did find that different types of prophylactic immunoglobulins produced differing rates of malignancy. On the basis of the studies a number of themes can be deduced. It is important that hearttransplant (HT) recipients should not be lost to follow-up. This was suggested by Chen et al [91] who also recommended 6-12 monthly abdominal and chest CT imaging with 12 monthly scans thereafter. This seems prudent given the high rates of malignancy recorded. Many of the positive risk factors (age, previous smoking status, sex) are non modifiable. However there are some encouraging results from the use of the newer mTOR-inhibitors and further examination of prophylactic immunoglobulins. CONCLUSIONS Cancers in HT recipients also have slightly differing characteristics compared to their equivalents in the general population. Namely, they have a preponderance for extralymphatic sites in PTLD [57], [58], [59], [60), and aggressive nature (SCC) [2], [3], [4], [5], [7]. Reported incidence of malignancy following HT varies hugely between studies. There are conflicting findings with regard to the commonest type of malignancy. Whereas Hereros [8] et al. estimated that skin cancers were the commonest type followed by PTLD a small study by Chen [92] et al. found PTLD to be most common. Aetiological causes for malignancy seem strongly dependant on the side effects of immunosuppressives [29] which likely act to inhibit the immune system’s response to earlier malignant changes in cells [19],[ 20]. This is an exciting emerging field within immunology and is an added challenge as length of survival and subsequent duration of immunosuppressive exposure is increased. Viruses such as HPV [51], EBV [61], [62], and HHV-8 [78], [79], [80], play an important role in the development of cancer in HT recipients. The mechanisms by which HPV and EBV induce the proliferation of cells is comparatively well understood compared to HHV-8. However the role of immunosuppressives in this process is not well understood but there is some evidence [86] that withdrawal of immune therapy can induce remission of KS implying that the drugs play a pivotal role. Much further work is needed in understanding the immune systems role in neoplasia, the role of the cancer causing viruses mentioned and the development newer immunosuppressive therapies. REFERENCES 1. Penn I, Post-transplant malignancy: The role of immunosuppression. Drug Saf. 2000; 23: 101 – 113 2. Penn I, Hammond W, Brettschneider L, et al. Malignant lymphomas in transplantation patients. Transplant Proc. 1969; 1: 106 -112. 3. Penn I, Why do immunosuppressed patients develop cancer? Crit Rev.Oncog. 1989; 1(1): 27 - 52. 4. Penn I, The problem of cancer in organ transplant recipients: an overview. Transplant Sci. 1994; 4(1): 23 - 32. 5. Penn I, Malignancy after immunosuppressive therapy: how can the risk be reduced? Clin Immunother 1995; 9: 207-218. 6. Penn I, Posttransplant malignancies. Transplant Proc. 1999; 31 (1-2): 1260 - 1262. 7. Penn I, De novo cancers in organ allograft recipients. Curr Opin. Organ Transplant. 1995; 3: 188 -196 8. Herreros J, Flórez S, Echevarría JR, Fernández AL, Pardo Mindán FJ. Lymphoproliferative disease and cancer in the transplant patient. Rev Esp Cardiol. 1995; 48 (7):129 -134. 9. Wiesner RH, A long term comparison of tacrolimus (FK506) versus cyclosporine in liver transplantation: a report of the United States FK506 Study Group. Transplantation. 1998; 66: 493-499. 10. Jonas S, Rayes N, Neumann U, et al. De novo malignancies after liver transplantation using tacrolimus-based protocols or cyclosporine-based quadruple immunosuppression with an interleukin-2 receptor antibody or antithymocyte globulin. Cancer. 1997; 80: 1141 - 1150 11. Penn I, Cancers in cyclosporine-treated versus azathioprine treated patients. Transplant Proc. 1996; 28: 876 - 878. 12. Wimmer D, Rentsch M, Crispin A, et al. The janus face of immunosuppression – de novo malignancy after renal transplantation: the experience of the Transplantation Center Munich. Kidney International .2007; 71: 1271–1278. 13. Burnet FM, Cancer—A Biological Approach: I. The Processes Of Control. II. The Significance of Somatic Mutation. Brit. Med. Jour. 1957; 1 (5022): 779–786. 14. Burnet FM, Immunological surveillance in neoplasia. Transplant Rev. 1971; 7: 3–25. 15. Thomas L, On immunosurveillance in human cancer. Biol Med. 1982; 55: 329 – 333 16. Ehrlich P Ueber den jetzigen stand der karzinomforschung. Ned Tijdschr Geneeskd. 1909; 5: 73 –290 17. Prehn RT, Main JM. Immunity to methylcholanthrene-induced sarcomas. J. Natl Cancer Inst. 1957; 18:769 – 778. 18. Old LJ, Boyse EA, Immunology of experimental tumors. Annu Rev Med. 1964; 15:167 – 186 19. Dunn GP, Old L J, Schreiber R D. The Three Es of Cancer Immunoediting. Annu. Rev. Immunol. 2004; 22: 329 –360 20. Dunn G P, Bruce A T, Ikeda H, et al. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002 3(11): 991-998. 21. Dunn GP, Old LJ, Schreiber RD, The Immunobiology of Cancer Immunosurveillance and Immunoediting. Immunity 2004; 21: 137 – 148. 22. Shankaran V, Ikeda H, Bruce AT, et al, IFN and lymphocytes prevent primary tumour development and shape tumour immunogenicity. Nature 2001; 410: 1107–1111. 23. Smyth MJ, Thia KY, Street SE, et al, Differential tumor surveillance by natural killer (NK) and NKT cells. J. Exp. Med. 2000; 191: 661 – 668 24. Smyth MJ, Crowe NY, Godfrey DI, NK cells and NKT cells collaborate in host protection from methylcholanthrene-induced fibrosarcoma. Int. Immunol.2001; 13: 459–463. 25. Hayakawa Y, Rovero S, Forni G, and Smyth M J, Suppression of chemical and oncogene dependent carcinogenesis. Proc. Natl. Acad. Sci.2003; 3 (2): 9464 – 9469. 26. Girardi M, Glusac E, Filler RB, et al, The distinct contri butions of murine T cell receptor (TCR)and TCRT cells to different stages of chemically induced skin cancer. J. Exp. Med.2003; 198: 747–755. 27. Girardi M, Oppenheim DE, Steele CR, et al, Regulation of Cutaneous Malignancy by γδ T Cells. Science 2001; 294: 605 - 609. 28. Gao Y, Yang W, Pan M, et al. T cells provide an early source of interferon in tumor immunity. J. Exp. Med. 2001; 198: 433 – 442 29. Taylor AL, Watson CJE , Bradley JA, Immunosuppressive agents in solid organ transplantation: Mechanisms of action and therapeutic efficacy. Critical Reviews in Oncology/Hematology 2005; 56: 23 – 46. 30. Shibasaki F, Hallin U, Uchino H, Calcineurin as a multifunctional regulator. J Biochem. 2002; 131(1): 1 – 15. 31. Hay N, Sonenberg N, Upstream and downstream of mTOR. Genes & Dev. 2004; 18: 19261945. 32. Kapic E, Becic F, Kusturica J, Med Arh. Basiliximab, mechanism of action and pharmacological properties. 2004; 58(6): 373 - 376. 33. Rose JW, Burns JB, Bjorklund J, et al, Daclizumab phase II trial in relapsing and remitting multiple sclerosis MRI and clinical results. Neurology.2007; 69 (8): 785–789. 34. Cantrell DA, Smith KA, The interleukin-2 T-cell system: a new cell growth model. Science.1984; 224 (4655): 1312–1316. 35. Smith KA , Interleukin-2: inception, impact, and implications. Science.1988; 240 (4856): 1169–1176. 36. Beadling CB, Smith KA, DNA array analysis of interleukin-2-regulated immediate/early genes. Med. Immunol. 2002; 1 (1):2. 37. Stern J, Smith KA, Interleukin-2 induction of T-cell G1 progression and c-myb expression. Science. 1986; 233 (4760): 203–206. 38. Waldmann TA, Tagaya Y , The multifaceted regulation of interleukin-15 expression and the role of this cytokine in NK cell differentiation and host response to intracellular pathogens. Annu. Rev. Immunol. 1999; 17: 19 – 49 39. Farge D, Kaposi's sarcoma in organ transplant recipients. The Collaborative Transplantation Research Group of Ile de France. The European Journal of Medicine 1993; 2(6): 339 - 343. 40. Euvrard S, Kanitakis J, Pouteil-Noble C, et al, Skin cancers in organ transplant recipients. Ann Transplant. 1997; 2: 28 - 32 41. Lampros TD, Cobanoglu A, Parker F, et al, Squamous and basal cell carcinoma in heart transplant recipients. J. Heart Lung Transplant. 1998; 6: 586 – 591 42. Ong CS, Keogh AM, Kossard S, et al, Skin cancer in Australian heart transplant recipients. J Am Acad Dermatol. 1999; 40: 27 – 34 43. Barr BBB, Benton EC, McLaren K, et al, Human papilloma virus infection and skin cancer in renal allograft recipients. Lancet. 1989; 1: 124 – 129 44. Hartevelt MM, Bouwes-Bavinck JN, Koote AM, et al, Incidence of skin cancer after renal transplantation in the Netherlands. Transplantation 1990; 49 (3): 506 - 509. 45. Sheil AGR, Skin cancer in renal transplant recipients. Transplant Sci. 1994; 4: 42. 46. Brewer JD, Colegio OR, Phillips PK, et al, Incidence of and risk factors for skin cancer after heart transplant. Arch Dermatol. 2009; 145(12): 1391 - 1396. 47. Euvrard S, Kanitakis J, Pouteil-Noble C, et al, Comparative epidemiologic study of premalignant and malignant epithelial cutaneous lesions developing after kidney and heart transplantation. J Am Acc.Dermatol.1995; 33: 222 – 229. 48. Molho-Pessacha V, Lotemb M, Viral Carcinogenesis in Skin Cancer Tur E (ed): Environmental Factors in Skin Diseases. Curr Probl Dermatol. 2007; 35: 39 – 51 49. Barr BB, Benton EC, McLaren K, et al, Papillomavirus infection and skin cancer in renal allograft recipients. Lancet 1989; 2 (8656): 224 - 225. 50. Glover MT, Niranjan N, Kwan JTC, et al, Non-melanoma skin cancer in renal transplant recipients: the extent of the problem and a strategy for management. Br J Plast Surg. 1994; 47: 86 - 89. 51. Stockfleth E, Nindl I, Sterry W, et al, Human papillomaviruses in transplant-associated skin cancers. Dermatol Surg. 2004; 30(4): 604 - 609. 52. McGregor JM, Berkhout RJM, Rozycka M, et al. Mutations implicate sunlight in posttransplant skin cancer irrespective of human papillomavirus status. Oncogene. 1997; 15: 1737 - 1740 53. Bouwes Bavinck JN, Vermeer BJ, van der Woude et al, Relation between skin cancer and HLA antigens in renal-transplant recipients. N Engl J Med. 1991;325(12): 843 - 848. 54. Festenstein H, Garrido F, MHC antigens and malignancy. Nature.1986; 322: 502 - 523. 55. Harris NL, Jaffe ES, Diebold J et al, The World Health Organization classification of neoplastic diseases of the haematopoietic and lymphoid tissues: report of the Clinical Advisory Committee Meeting, Airlie House, Virginia, November 1997. Histopathology 2000; 361: 69 – 86. 56. LaCasce AS, Post-Transplant Lymphoproliferative Disorders. The Oncologist 2006; 11 (6) 674-680. 57. Nalesnik MA, Clinicopathologic characteristics of post-transplant lymphoproliferative disorders. Recent Results Cancer Res. 2002; 159: 9 – 18 58. Penn I, Occurrence of cancers in immunosuppressed organ transplant recipients. Clin Transpl. 1998; 10: 147 – 158 59. Morrison VA, Dunn DL, Manivel JC, et al, Clinical characteristics of post-transplant lymphoproliferative disorders. Am. J. Med. 1994; 97: 14 –24. 60. Opelz G, Do¨hler B, Lymphomas After Solid Organ Transplantation: A Collaborative Transplant Study Report. American Journal of Transplantation 2003; 4: 222 – 230. 61. Lennard L, Thomas M, Harrington C, et al. Skin cancer in renal transplant patients is associated with increased concentrationsof 6-thioguanine nucleotide in red blood cells. Br J Dermatol.1985; 113: 723 - 729. 62. Hanto DW, Classification of Epstein-Barr virus-associated posttransplant lymphoproliferative diseases: implications for understanding their pathogenesis and developing rational treatment strategies. Ann. Rev. Med 1995; 46: 381 - 394. 63. Boubenider S, Hiesse C, Goupy C, et al, Incidence and consequences of posttransplantation lymphoproliferative disorders. J Nephrol. 1997; 10 (3):136 – 145. 64. Feng S, Buell JF, Chari RS, et al, Tumors and transplantation: the 2003 third annual ASTS state-of-the-art winter symposium Am J Transplant. 2003; 3 (12):1481 –1487. 65. Ho M, Jaffe R,Miller G, et al, The frequency of Epstein-Barr virus infection and associated lymphoproliferative syndrome after transplantation and its manifestations in children. Transplantation 1988; 45: 719 -27. 66. Walker RC, Marshall WF, Strickler JG et al, Pretransplantation assessment of the risk of lymphoproliferative disorder. Clin Infect Dis. 1995;20:1346 –1353. 67. Smets F, Sokal E M, Epstein-Baar virus-related lymphoproliferation in children after liver transplantation: Role of immunity, diagnosis, and management. Pediatric Transplantation 2002; 6: 280 – 287 68. Newell K A, Alonso E M, Whitington P F, et al, Post-transplant lymphoproliferative disease in pediatric liver transplantation. Interplay between primary Epstein-Barr virus and immunosuppression. Transplantation1996; 62: 370 – 375. 69. Cohen JI, Epstein–Barr virus infection. New Engl J Med. 2000; 343: 481 –492. 70. Loren A W, Porter D L, Stadtmauer E A, Tsai D E, Post-transplant lymphoproliferative disorder: a review. Bone Marrow Transplantation 2003; 31: 145–155. 71. Ohta H, Fukushima N, Ozono K, Pediatric post-transplant lymphoproliferative disorder after cardiac transplantation. Int J Hematol. 2009; 90(2):127 - 136. 72. Penn I, Immunosuppressive agents, immunodeficiency states and malignancy. In: Lieberman R,Mukherjee A, editors. Principles of drug development in transplantation and autoimmunity 1996: 93-102. 73. Penn I, The role of immunosuppression in lymphoma formation. Springer Semin Immunopathol. 1998; 20 (3-4): 343-55. 74. Penn I, Porat G. Central nervous system lymphomas in organ allograft recipients. Transplantation 1995; 59: 240 -244 75. Rahim Rezaee SA, Cunningham C, Davison AJ, Blackbourn DJ, Kaposi's sarcomaassociated herpes virus immune modulation: an overview. Journal of General Virology 2006; 87: 1781 –1804. 76. Nicholas J, Human herpesvirus-8-encoded signalling ligands and receptors. J. Biomed Sci. 2003; 10: 475 –489. 77. Milligan S, Robinson M, O'Donnell E, Blackbourn DJ, Inflammatory cytokines inhibit Kaposi's sarcoma-associated herpes virus lytic gene transcription in in vitro-infected endothelial cells. J. Virol. 2004;78: 2591–2596. 78. Neipel F, Albrecht J-C, Fleckenstein B, Cell-homologous genes in the Kaposi's sarcomaassociated rhadinovirus human herpesvirus 8: determinants of its pathogenicity? J Virol. 1997; 71: 4187 – 4192 79. Russo J J, Bohenzky R A, Chien M-C, et al, Nucleotide sequence of the Kaposi sarcomaassociated herpesvirus (HHV8). Proc. Natl. Acad Sci 1996; 93: 14862–14867. 80. Moore P, Chang Y, Kaposi’s sarcoma-associated herpesvirus. In: Knipe DM, Howley PM, Griffin DE, et al, eds. Fields’ Virology. 4th ed. Philadelphia, PA: Lippincott, Williams & Wilkins; 2001; 2803-2833. 81. Lepone L, Rappocciolo G, Piazza P, et al, CD4 regulatory T cells Control CD8 T cell responses to human Herpesvirus 8 lytic and latency proteins. Infectious Agents and Cancer 2012; 7(1):1507-1516. 82. Wang QJ, Jenkins FJ, Jacobson LP. CD8+ cytotoxic T lymphocyte responses to lytic proteins of human herpes virus 8 in human immunodeficiency virus type 1-infected and uninfected individuals. J Infect Dis. 2000 Sep; 182(3): 928 - 932. 83. Penn I, Sarcomas in organ allograft recipients. Transplantation 1995; 6O: 1485 -1491. 84. Penn I, Kaposi’s sarcoma in transplant recipients. Transplantation.1997; 64: 669-673. 85. Kaposi M, Idiopathic multiple pigmented sarcoma of the skin. CA Cancer J. Clin. 1982; 32: 342 -347 86. Sarid R, Olsen SJ, Moore PS, Kaposi's sarcoma-associated herpesvirus: epidemiology, virology, and molecular biology. Adv. Virus Res. 1999; 52: 139 - 232 87. Moray G, Basaran O, Yagmurdur MC, Immunosuppressive therapy and Kaposi's sarcoma after kidney transplantation. Transplantation Proceedings 2004; 36 (1):168 -170. 88. Aprosio N, Batzenschlager A, Hamid M, et al, Kaposi disease with mesenteric localization (article in French). Presse Med. 1984; 13: 504. 89. Meyer-Rochow GY, Lee KM, Smeeton IW, Shaw JH,Primary Kaposi sarcoma of the appendix: a rare cause of appendicitis. ANZ. J Surg 2007; 77: 402 - 403. 90. Elizalde JI, Escorsell A, García-Pugés A, et al, Isolated rectal Kaposi sarcoma (article in Spanish). Rev Esp Enferm Dig 1993; 84: 399 - 4 01. 91. Gorin FA, Bale JF Jr, Halks-Miller M, Schwartz RA, Kaposi's sarcoma metastatic to the CNS. Arch Neurol. 1985; 42(2): 162 - 165. 92. Chen PL, Chang HH, Chen IM, et al, Malignancy after heart transplantation. J Chin Med Assoc. 2009; 72(11): 588 - 593. 93. Crespo-Leiro MG, Alonso-Pulpón L, Vázquez de Prada JA, et al, Malignancy after heart transplantation: incidence, prognosis and risk factors. Am J Transplant. 2008; 8(5): 1031-9. 94. Doesch AO, Müller S, Konstandin M, et al, Malignancies after heart transplantation: incidence, risk factors, and effects of calcineurin inhibitor withdrawal. Transplant Proc. 2010; 42(9): 3694-3699. 95. Roithmaier S, Haydon AM, Loi S, Incidence of Malignancies in Heart and/or Lung Transplant Recipients: A Single-Institution Experience. The Journal of Heart and Lung Transplantation. 2007; 26(8): 845-849. 96. Rinaldi R, Pellegrini C, D'Armini AM, Neoplastic disease after heart transplantation: single center experience. Eur J Cardiothorac Surg. 2001; 19 (5): 696-701. .