2006-12-03 Beyond Mammography
advertisement

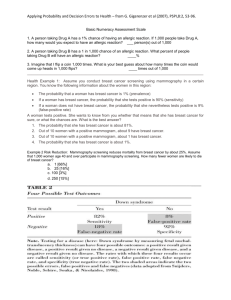
Preventive Medicine Column December 3, 2006 Beyond Mammography My wife, of course, gets timely mammography screening. For one thing, she is an intelligent and wellinformed woman in her 40s for whom annual mammogram is clearly recommended. For another, her husband is a Preventive Medicine specialist, who would look pretty silly if his immediate family didn’t practice what he spent his life preaching. And perhaps most compelling, her mother has been treatedsuccessfully, thank goodness- for the condition. But while Catherine gets her annual mammogram, that doesn’t mean she is particularly happy to do so. She has made it abundantly clear to me that the procedure is a nuisance at best, downright painful at worst. And more than once, ‘questionable’ spots on her mammogram have caused us both anxiety and sleepless nights while waiting for follow-up tests to prove that nothing, in fact, was wrong. So it’s good news for my family as well as yours that advances in breast cancer screening are clearly visible on the horizon. Last week, at the annual meeting of the Radiological Society of North America in Chicago, a technique called Cone Beam Brest Computed Tomography (CBBT) was presented. Unlike the conventional mammogram, this technique does not need to compress the breast against x-ray film (the part my wife, and every woman, objects to), but rather obtains multiple images from different angles and superimposes them. The preliminary data presented at the recent meeting suggest that CBBT performs at least as well as mammography, but that is based on a small sample of healthy women. How the test will perform in a more diverse population remains to be seen, so it’s not yet ready for prime time. But it is a harbinger of advances to come in the not-too-distant future. And it’s not the only one. Computers have been used to enhance the interpretation of mammograms. This falls short, of course, of replacing mammography, but improving the accuracy of the testing is an important goal in its own right, and computer assisted interpretation of mammograms shows some promise in this regard. While clearly shown to save lives- reducing the risk of breast cancer death by roughly 30%conventional mammography does suffer from important inaccuracies. In a seminal paper published nearly 10 years ago in the New England Journal of Medicine, Dr. Joanne Elmore, formerly a Yale colleague and now at the University of Washington in Seattle, showed that mammography produced nearly 13 false positive readings for every true positive. The accuracy of mammography has improved since, partly due to the work of Dr. Elmore and her colleagues, but false positives (thinking breast cancer is present when it is not), and to a lesser extent false negatives (overlooking actual breast cancer) do still occur. High resolution ultrasound has been tested as an alternative to mammogram. Ultrasound has traditionally been used for confirmatory testing when a mammogram image is suspicious. Using ultrasound as the primary screening technique, which offers the advantage of avoiding radiation, looked promising in a recent trial in Germany. Other imaging techniques that might compete with mammography are under evaluation as well. These include thermography, which measures temperature and is useful because the high growth rate of tumors makes them warmer than the surrounding tissue. MRI scans are now used to evaluate breast tissue once an abnormality is suspected, but might be useful as an initial screening test. Other tests under investigation as alternatives, or in some cases additions, to conventional mammography include digitally enhanced mammograms; 3-demensional ultrasound; positron emission tomography, which measures the metabolic activity of tissues; blood tests for proteins that leak from cancer cells; and even direct aspiration of ductal cells from the breast for microscopic examination. A quest for reliable alternatives to mammography has been on-going for decades. At this point, it seems clear that breast cancer screening will, at last, be going beyond mammograms soon. But thus far, mammograms remain the industry standard for early detection of a disease that effects over 180,000 women each year in the US, claiming some 40,000 lives. While waiting for screening tests that combine marvelous accuracy with perfect comfort and convenience, we should not make perfect the enemy of good. Mammography, colonosocopy, and other cancer screening tests are imperfect, but nonetheless can save your life. While waiting for the better tests of tomorrow to arrive, check with you doctor to be sure you get the important tests we have available today. -fin David L. Katz, MD, MPH, FACPM, FACP; Director, Prevention Research Center, Yale University School of Medicine; Medical Contributor, ABC News: www.davidkatzmd.com New Breast Scanner Rivals Mammograms And it works without flattening the breast, researchers say By Amanda Gardner HealthDay Reporter MONDAY, Nov. 27 (HealthDay News) -- A new imaging system has the promise of equaling or surpassing mammography in detecting breast cancer. And it does it without squeezing the breast in a vice. But the device is not thoroughly proven, and experts are urging caution in interpreting the findings. "I'm enthusiastic. This sounds like something that's very helpful, but there have been a large number of technologies that each promise to take over mammography, but each time that proves not to be the case," said Dr. Joshua Kalowitz, chief of breast imaging at Maimonides Cancer Center in New York City. The technology featured in this study, the Cone Beam Breast Computed Tomography (CBBCT) scanner, has primarily been tested only in healthy women and may not be able to pick up tiny abnormalities because of the resolution, Kalowitz added. Preliminary results from a pilot study of the technique were to be presented Monday at the Radiological Society of North America's annual meeting, in Chicago. Regular or film mammography is currently the gold standard for breast cancer detection. The challenge has been to find ways to detect malignancies at ever earlier stages, when they have a better chance of being cured. The problem with mammography is that breasts, particularly in younger women, tend to be very dense, with much of that density captured in a mammogram. "A mammogram is limited because the density of the tissue above and below the area we're interested in may block our view," Kalowitz explained. "If something is smack in the middle of dense tissue, we may not be able to see it." The CBBCT scanner takes a number of pictures of the breast from various angles then merges them into one 3-dimensional image. The system was developed by a professor at the University of Rochester, which holds several patents on the technology. The university licensed the technology to Koning Corporation to make, use and sell the scanners. The National Cancer Institute, along with private investors, helped fund the development of the scanner. This pilot study used the CBBCT scanner to image 20 volunteers who had had normal mammograms, as well as a group of women who had had abnormalities detected during a physical exam or who had had suspicious mammograms. The goal of the study was simply to see how well the CBBCT could image the breast The CBBCT proved itself at least as good as conventional mammogram in imaging the breast, the authors concluded. The system also has the advantage of being more comfortable. The woman lies on her stomach on a cushioned exam table with a cutout in the middle. She suspends her breasts one at a time through the cutout while the CBBCT takes 300 images in the space of about 10 seconds. The radiation dose is comparable to that of mammography. Unlike conventional mammography, the CBBCT system clearly displays tissue around the ribs and outer breast near the armpits. The pilot study will continue until 60 participants have been imaged. A larger trial is planned for next year. Koning Corp. hopes to have a commercial scanner on the market as soon as the U.S. Food and Drug Administration approves the device. But other technologies may be further along, Kalowitz said. "There's a lot of new stuff on the horizon," he said. "Five years from now, we'll be in a lot better shape, but right now, we have to see which ones will end up being the best." Other research being presented at the Radiological Society meeting found that a new ultrasound technique called "elasticity imaging" allows doctors to accurately differentiate malignant and benign breast lesions. An estimated 213,000 U.S. women will be found to have invasive breast cancer in 2006, and about 40,970 women will die from the disease this year. Right now, there are slightly more than 2 million American women who have been treated for breast cancer, according to the American Cancer Society. More information Visit the National Cancer Institute for more on breast cancer screening. SOURCES: Joshua Kalowitz, M.D., chief of breast imaging, Maimonides Cancer Center, New York City; Nov. 27, 2006, presentation, Radiological Society of North America annual meeting, Chicago 1: AJR Am J Roentgenol. 2006 Dec;187(6):1475-82. Testing the effect of computer-assisted detection on interpretive performance in screening mammography. Taplin SH, Rutter CM, Lehman CD. Group Health Cooperative, Center for Health Studies, Seattle, WA 98101, USA. OBJECTIVE: The objective of our study was to test whether the use of computer-assisted detection (CAD) improves sensitivity at no cost to specificity for the detection of breast cancer and enables more accurate assessment of fatty breast tissue compared with dense breast tissue. MATERIALS AND METHODS: We created a stratified random sample of screening mammograms weighted with difficult cases split evenly among women with fatty breast tissue and those with dense breast tissue: 114 patients were cancer-free, 114 had cancer 1 year after screening, and 113 had cancer 13-24 months after screening. In test settings 6 months apart, 19 community radiologists interpreted 341 bilateral screening mammograms with and without CAD. We compared the sensitivity and specificity using regression models adjusting for repeated measures. RESULTS: CAD assistance did not affect overall sensitivity (cancer by 1 year: 63.2% without CAD and 62.0% with CAD; cancer in 13-24 months: 33.5% without CAD and 32.3% with CAD), but its effect differed for visible masses that were marked by CAD compared with those that were not marked by CAD (hereafter referred to as "unmarked"). CAD was associated with improved sensitivity for marked visible cancers and decreased sensitivity for unmarked visible masses; the sensitivities without and with CAD, respectively, were as follows: marked cancer by 1 year, 82.7% versus 83.1%; marked cancer in 13-24 months, 44.2% versus 57.9%; unmarked cancer by 1 year, 37.4% versus 30.1%; unmarked cancer in 13-24 months, 29.7% versus 23.0% (p < 0.03 for both interactions between assistance and CAD marking for cancer by 1 year and cancer in 13-24 months). CAD marked 77% (70/91) of the visible cancers by 1 year and 67.3% (37/55) of the visible cancers in 13-24 months. CAD marked more visible calcified lesions (86%) than masses and asymmetric densities (67%) (p < 0.05). Overall specificity was 72% without and 75% with CAD (p < 0.02). CAD had a greater effect on both specificity (p < 0.02) and sensitivity (p < 0.03) among radiologists who interpret more than 50 mammograms per week. The results were the same for fatty breast tissue and dense breast tissue. CONCLUSION: In this experiment, CAD increased interpretive specificity but did not affect sensitivity because visible noncalcified lesions that went unmarked by CAD were less likely to be assessed as abnormal by radiologists. Breast density did not affect CAD's performance. Publication Types: Research Support, N.I.H., Extramural PMID: 17114540 [PubMed - in process] 2: Anticancer Res. 2006 Sep-Oct;26(5B):3943-55. Non-palpable breast lesions in asymptomatic women: diagnostic value of initial ultrasonography and comparison with mammography. Ohlinger R, Heyer H, Thomas A, Paepke S, Warm H, Klug U, Frese H, Schulz K, Schimming A, Schwesinger G, Kohler G, Wodny M, Kohlmann T, Grunwald S. Department of Gynecology and Obstetrics, Ernst-Moritz-Arndt-University, Greifswald, Germany. ralf.ohlinger@uni-greifswald.de AIM: This prospective double-blind study was designed to assess (i) if primary breast screening by ultrasonography is capable of detecting breast cancer independent of tissue density and (ii) if the rate of unnecessary biopsies remains acceptable when diagnostics are based on ultrasonography. PATIENTS AND METHODS: Bilateral breast ultrasonography was performed in 448 asymptomatic women as the initial diagnostic method. Sonograms were interpreted using a set of standardized diagnostic criteria. Subsequently, mammograms were obtained. The radiologists reading the mammograms were blinded to the sonographic results. RESULTS: Overall, 3 non-palpable breast cancers were detected by ultrasound and mammography. All 3 ultrasonographically detected breast cancers were smaller than 1 cm (0.7, 0.7, 0.6 cm). All 3 carcinomas were correctly detected by both methods. For ultrasonography, the false positive rate was 1.1% (n=5) and for mammography 0.6% (n=3). When both methods were combined, the rate of unnecessary open biopsies was 1.6% (n=7). The ratio of benign to malignant lesions was 3.7/1. CONCLUSION: Without prior mammography, primary high-resolution breast ultrasonography is capable of detecting non-palpable breast carcinomas in asymptomatic women at an early stage. The rate of unnecessary open biopsies is low and the ratio of benign to malignant biopsies acceptable. PMID: 17094426 [PubMed - in process] 3: Radiol Manage. 2004 Jul-Aug;26(4):16-24; quiz 25-7. Emerging technologies in breast cancer detection. Smith AP, Hall PA, Marcello DM. Hologic Inc, Bedford, MA, USA. asmith@hologic.com While screening mammography is recognized as the most effective method for early detection of breast cancer, this modality has limitations that are the driving force behind efforts to refine existing mammography technologies and develop new ones offering improved detection of breast cancer. Full-field digital mammography (FFDM) systems use digital detectors to convert x-ray photons to digital signals for display on high-resolution monitors. These systems offer capabilities not provided by conventional film-screen mammography. Contrast-enhanced mammography utilizes the basic biological principle that aggressive cancers are associated with increased vascularity. Iodinated contrast agents--the same used in computed tomography (CT) examinations--are administered through an injection in a vein usually in the arm. They distribute throughout the blood system, and x-ray imaging shows increased contrast in areas where they concentrate. Tomosynthesis acquisition involves acquiring multiple images of a stationary compressed breast at different angles during a short scan. The individual images are then reconstructed into a 3D series of thin high-resolution slices. The slices can be displayed individually or in a dynamic cine mode. The individual slices reduce tissue overlap and structure noise relative to standard 2D projection mammography, with a total dose comparable to that required for standard screening mammography. Initial efforts are underway to develop prototype systems to achieve high-resolution, whole-breast 3D ultrasound images that are co-registered with digital mammograms. This technology has the potential to improve specificity in breast imaging studies, particularly in dense breasts. Computer-aided detection (CAD) programs are intended to help radiologists identify suspicious lesions that may otherwise be overlooked. CAD software works similarly to a spellchecker and has the potential to increase the detection of cancer Magnetic resonanace imaging (MRI) is a generally accepted diagnostic procedure for a number of breast related indications. Its greatest strength is that it is very sensitive to tumors. If a suspected area does not exhibit contrast agent uptake, the probability that it is malignant is very small. Conversely, its specificity is poorer. If the area does show enhancement, it may or may not be a tumor. Further imaging or biopsy may be needed to resolve the question. Ultrasound holds promise as a method for detection of cancers in women with dense breast tissue, which is often problematic with conventional film-screen mammography. Ultrasound has also assumed an important role in breast imaging, as an adjunct to diagnostic mammography for biopsy guidance, palpable mass evaluation, and serial evaluation of benign masses. PMID: 15377106 [PubMed - indexed for MEDLINE] 4: Mol Diagn. 2003;7(1):49-55. Breast cancer: new technologies for risk assessment and diagnosis. Wright T, McGechan A. Adis International Inc., Yardley, Pennsylvania 19067, USA. innovation@adis.com In the US, one in every eight women will develop breast cancer in her lifetime. Despite the advances made in treating breast cancer, the causal mechanisms underlying this disease have yet to be fully elucidated; 85% of breast cancer cases occur sporadically without any known genetic mutation. Too little is known about the pathogenesis of breast cancer for primary prevention to be feasible in the near- to mid-term. Secondary prevention through screening offers an alternative that has been widely adopted. For decades, breast selfexamination has been touted as a technique for the early identification of breast cancer. However, it has been recently suggested that this technique is a waste of time and resources for both doctors and patients. Mammography finds breast cancer earlier than breast self-examination, and will reduce the risk of death from breast cancer by approximately 30% in women over 50 years old. Mammography is limited in that cancer, like breast tissue, appears white on the x-ray; therefore lesions may be difficult to detect in women with very dense breasts, and a tumor may not cast a significant shadow until it is quite large. Some cancers are so aggressive that they can spread quickly, before routine screening can detect them. Despite these limitations, mammography is still viewed as the best tool currently available for screening and early diagnosis. Improved methods to detect and diagnose breast cancer early, when it is most curable, are required if a significant impact on morbidity and mortality from breast cancer is to be made. Various new and innovative technologies are being investigated for improving the early detection and diagnosis of breast cancer. About 85% of breast cancers begin in the milk ductal system of the breast. As cancer develops in the breast, abnormalities occur, including atypical hyperplasia, ductal carcinoma in situ, and invasive breast carcinoma. Thus, the early screening of ductal cells can provide a parallel benefit to the 'Pap' smear, which is used virtually universally to identify the abnormal cells that can lead to cervical cancer. Two technologies to monitor for atypical ductal epithelial cells are Cytyc Corporation's FirstCyte Ductal Lavage system and Nastech Pharmaceutical Company's Mammary Aspiration Cytology Test. Matritech, Inc. is searching for biomarkers linked to breast cancer. Researchers at Matritech have detected the presence of nuclear matrix protein (NMP) in the blood of women at the early stage of breast cancer, which is absent in the blood of healthy women, as well as those with fibroadenoma, a benign breast disease. NMP66 has been selected as a marker for further development and clinical trials of a test for use in the detection and monitoring of women with, or at risk for, breast cancer have been initiated. Technologies developed by the US Department of Defense are under investigation as breast cancer screening. Advanced Image Enhancement, Inc. has licensed naval sonar technology for digital image enhancement of mammograms. New thermography applications are also being investigated in two separate projects sponsored by the US Department of Defense using military thermal surveillance tools adapted for cancer detection. Both are enhancements of older thermal imaging technology based on the principle that heat equates to unwanted activity, in the case of breast cancer, abnormal cell proliferation. Publication Types: Review PMID: 14529321 [PubMed - indexed for MEDLINE] 5: Ann Oncol. 2004;15 Suppl 1:I18-I26. Comment in: Ann Oncol. 2004;15 Suppl 1:I5-I6. An overview of the status of imaging screening technology for breast cancer. Smith JA, Andreopoulou E. Department of Medicine, New York University School of Medicine and New York University Cancer Institute, New York, NY 10016, USA. smithj01@med.nyu.edu With breast cancer incidence rates showing no signs of abating, advances in risk stratification and increasing awareness of cancer control, there is interest in expanding the breast imaging arsenal. Mammography is still the standard of care, and a recent meta-analysis of seven large studies supports its value as a screening tool. There is, however, clear need for improved sensitivity and specificity. Imaging of function, metabolism and molecular activity in breast tissue is of potential benefit in addressing these issues. In this article we provide an overview of the current methods of imaging in breast cancer, including mammography, ultrasound, digital mammography, magnetic resonance, positron emission tomography and magnetic resonance spectroscopy. Screening and surveillance should, ideally, be tailored to an individual's cancer risk and breast tissue. Current evidence questions the recent move toward magnetic resonance imaging as a single or multimodality strategy for breast cancer screening. In a high-risk group, the cost effectiveness of technical innovations may be justified. Copyright 2004 European Society for Medical Oncology Publication Types: Review PMID: 15280183 [PubMed - indexed for MEDLINE] 6: Clin Breast Cancer. 2003 Apr;4(1):63-70. Digital mammography: a review of technical development and clinical applications. Shah AJ, Wang J, Yamada T, Fajardo LL. Department of Radiology, University of Iowa Carver School of Medicine, Iowa City, Iowa, USA. For detecting and diagnosing breast cancer at its earliest stage, mammography is the most sensitive technique currently available and is therefore the method of choice. Screen-film mammography has been used successfully as a screening test for breast cancer for > 2 decades. However, conventional mammography has substantial limitations and, therefore, digital mammography systems have been developed to improve image quality and overcome the limitations of screenfilm technique limitations. Herein we discuss the differences between screen-film and digital mammography systems and the processes related to digital mammography that differ from conventional mammography, including detector technology, digital image formation, image processing, image display, and image archival. Finally, we review the results from currently available clinical trials regarding the performance of digital mammography and discuss clinical implications such as cost-effectiveness. Publication Types: Review PMID: 12744760 [PubMed - indexed for MEDLINE] 7: Obstet Gynecol Clin North Am. 1987 Sep;14(3):651-65. Nonmammographic breast imaging techniques. Current status and future developments. Kopans DB. Department of Radiology, Massachusetts General Hospital, Boston. X-ray mammography (film/screen or Xerox) is the only breast imaging technique with proven efficacy for screening. Ultrasound has a limited diagnostic capability for cyst/solid differentiation. All other modalities should be considered experimental or of no proven benefit for breast evaluation. Publication Types: Review PMID: 3323969 [PubMed - indexed for MEDLINE] 1: N Engl J Med. 1998 Apr 16;338(16):1089-96. Comment in: N Engl J N Engl J N Engl J N Engl J N Engl J N Engl J N Engl J N Engl J Med. Med. Med. Med. Med. Med. Med. Med. 1998 1998 1998 1998 1998 1998 1998 1998 Apr Aug Aug Aug Aug Aug Aug Aug 16;338(16):1145-6. 20;339(8):560-1; author reply 563. 20;339(8):560; author reply 563. 20;339(8):561-2; author reply 563. 20;339(8):561; author reply 563. 20;339(8):562-4. 20;339(8):562; author reply 563. 20;339(8):562; author reply 563. Ten-year risk of false positive screening mammograms and clinical breast examinations. Elmore JG, Barton MB, Moceri VM, Polk S, Arena PJ, Fletcher SW. Department of Medicine, University of Washington School of Medicine, Seattle 98195-6429, USA. BACKGROUND: The cumulative risk of a false positive result from a breastcancer screening test is unknown. METHODS: We performed a 10-year retrospective cohort study of breast-cancer screening and diagnostic evaluations among 2400 women who were 40 to 69 years old at study entry. Mammograms or clinical breast examinations that were interpreted as indeterminate, aroused a suspicion of cancer, or prompted recommendations for additional workup in women in whom breast cancer was not diagnosed within the next year were considered to be false positive tests. RESULTS: A total of 9762 screening mammograms and 10,905 screening clinical breast examinations were performed, for a median of 4 mammograms and 5 clinical breast examinations per woman over the 10-year period. Of the women who were screened, 23.8 percent had at least one false positive mammogram, 13.4 percent had at least one false positive breast examination, and 31.7 percent had at least one false positive result for either test. The estimated cumulative risk of a false positive result was 49.1 percent (95 percent confidence interval, 40.3 to 64.1 percent) after 10 mammograms and 22.3 percent (95 percent confidence interval, 19.2 to 27.5 percent) after 10 clinical breast examinations. The false positive tests led to 870 outpatient appointments, 539 diagnostic mammograms, 186 ultrasound examinations, 188 biopsies, and 1 hospitalization. We estimate that among women who do not have breast cancer, 18.6 percent (95 percent confidence interval, 9.8 to 41.2 percent) will undergo a biopsy after 10 mammograms, and 6.2 percent (95 percent confidence interval, 3.7 to 11.2 percent) after 10 clinical breast examinations. For every 100 dollars spent for screening, an additional 33 dollars was spent to evaluate the false positive results. CONCLUSIONS: Over 10 years, one third of women screened had an abnormal test result that required additional evaluation, even though no breast cancer was present. Techniques are needed to decrease false positive results while maintaining high sensitivity. Physicians should educate women about the risk of a false positive result from a screening test for breast cancer. PMID: 9545356 [PubMed - indexed for MEDLINE] Related Links Effect of false-positive mammograms on interval breast cancer screening in a health maintenance organization. [Ann Intern Med. 1999] PMID:10391809 Predicting the cumulative risk of false-positive mammograms. [J Natl Cancer Inst. 2000] PMID:11036111 Screening mammography for frail older women: what are the burdens? [J Gen Intern Med. 2001] PMID:11722693 Effect of estrogen replacement therapy on the specificity and sensitivity of screening mammography. [J Natl Cancer Inst. 1996] PMID:8627640 Physician predictors of mammographic accuracy. [J Natl Cancer Inst. 2005] PMID:15741572