Tableofcontents
advertisement

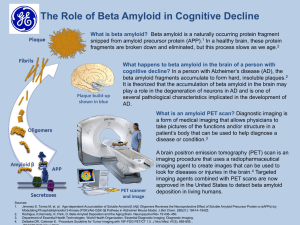
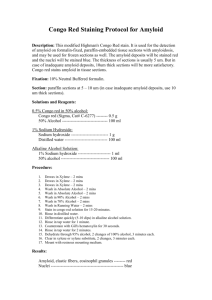
TABLE OF CONTENTS Acknowledgements i Abbreviations ii Abstract iv Conference proceedings x Foreword xi CHAPTER 1: INTRODUCTION 1.1 Diabetes 1 1.2 Structure of the IAPP gene 5 1.3 Biosynthesis of IAPP 7 1.4 Functions of IAPP 8 1.5 Amyloid formation 9 1.6 Fibril structure 13 1.7 Species-specific differences in the sequence of IAPP 15 1.8 Structural models for IAPP amyloid 17 1.9 What prevents IAPP from forming amyloid normally? 22 1.10 Why does IAPP amyloid form in Type 2 diabetes? 23 1.11 Defence against amyloidosis 26 1.12 Clusterin 28 CHAPTER 2: MATERIALS AND METHODS 2.1 MATERIALS 31 2.1.1 Buffers and solutions 33 2.1.2 Protein and antibodies 34 2.1.3 Bacterial culture media 34 2.1.4 Bacterial strains 34 2.2 METHODS 35 2.2.1 Agarose gel electrophoresis 35 2.2.2 Preparation of competent E. coli cells 35 2.2.3 Transformation of E. coli 35 2.2.4 Purification of pET 32/trx-proIAPP plasmid 36 2.2.6 SDS-PAGE 37 (a) Sample preparation 37 (b) Tris-glycine SDS-PAGE 37 (c) Tris-tricine SDS-PAGE 38 2.2.7 Cell lysis protocols for the purification under native conditions (a) Lysis by sonication in the absence of detergents 38 (b) Cell lysis by incubation with 1% Triton X-100 in the presence of PMSF 39 (c) Cell lysis by sonication in the presence of Triton X-100 and/or sarcosyl with protease inhibitors 39 2.2.8 Purification of trx-proIAPP under denaturing conditions using Ni-NTA chromatography (a) Purification in 6 M urea 39 (b) Purification 6 M GuHCl using Ni-NTA chromatography and refolding by dilution 40 (c) Purification in 6 M GuHCl by Ni-NTA chromatography and refolding on the Ni-NTA column 41 2.2.9 RP-HPLC protocols (a) Purification of trx-proIAPP 41 (b) Purification of proIAPP from trx-tag 42 2.2.10 Enterokinase cleavage conditions (a) Optimization trials 42 (b) Optimized enterokinase cleavage conditions 43 2.2.11 Electrospray mass spectrometry 43 2.2.12 Purification of proIAPP from trx-tag using Ni-NTA chromatography 43 2.2.13 Removal of buffer salts and reconcentration of proIAPP using a Strata-X column 43 2.2.14 Reconstitution of proIAPP lyophilisate 44 2.2.15 Circular dichroism spectropolarimetry 44 2.2.16 Fluorescence assays (a) ThT assays 45 (b) Bis-ANS assays 46 2.2.17 Congo Red Spectral Assay 47 2.2.18 Clusterin purification 47 2.2.19 Transmission electron microscopy aggregation assay 48 2.2.20 TEM and immunogold labelling of clusterin 48 2.2.21 Quantitation of clusterin binding to proIAPP by a direct ELISA 49 2.2.22 Quantitation of clusterin binding to proIAPP by competition ELISA 50 2.2.23 Bicinchoninic acid assay 51 2.2.24 Zone electrophoresis and amido black staining and immunoblotting for clusterin 52 2.2.25 Dot blotting 53 2.2.26 General culture conditions for RIN-m5f cells 54 2.2.27 Cytotoxicity of proIAPP measured by MTS 54 2.2.28 Controls for cytotoxicity assays 55 2.2.29 The effect of adding clusterin to proIAPP at different stages of amyloid formation on cytotoxicity 55 2.2.30 The cytotoxicity of proIAPP species formed in the presence and absence of clusterin 56 2.2.31 ProIAPP binding to heparin-agarose beads 56 2.2.32 FITC-labelling of heparin 57 2.2.33 Measurement of the FITC-heparin associated with fibrillar proIAPP 58 CHAPTER 3: OPTIMIZATION OF ProIAPP PURIFICATION 3.1 INTRODUCTION 59 3.2 RESULTS 60 3.2.1 Previous methods for proIAPP purification 60 3.2.2 Overexpression of trx-proIAPP in E. coli BL21 cells 60 3.2.3 Attempts to solubilise trx-proIAPP 61 3.2.4 Purification of trx-proIAPP in 6 M urea using Ni-NTA chromatography 3.2.5 Further purification of trx-proIAPP by RP-HPLC 65 66 3.2.6 Purification of trx-proIAPP in 6 M GuHCl using Ni-NTA chromatography and refolding by dilution 68 3.2.7 Purification of trx-proIAPP in 6 M GuHCl by Ni-NTA chromatography and refolding on the Ni-NTA column 70 3.2.8 Optimization of enterokinase cleavage conditions 71 3.2.9 Purification of proIAPP from trx-tag by RP-HPLC 74 3.2.10 Purification of proIAPP from trx-tag using Ni-NTA chromatography 76 3.2.11 Removal of buffer salts and re-concentration of proIAPP using a Strata-X column 3.5 DISCUSSION 77 79 CHAPTER 4: ProIAPP AMYLOID FORMATION 4.1 INTRODUCTION 83 4.2 RESULTS 4.2.1 Secondary structure of proIAPP 85 4.2.2 Ageing of proIAPP followed by far-UV-CD 89 4.2.3 Kinetics of proIAPP amyloid formation 91 4.2.4 The effect of macromolecular crowding 94 4.2.5 The effect of ionic strength on proIAPP amyloid formation 96 4.2.6 SDS-PAGE analysis of proIAPP amyloid formation 97 4.2.7 Binding of Congo Red to proIAPP fibrils 100 4.2.8 Transmission electron microscopy of proIAPP fibrils 101 4.2.9 Binding of bis-ANS to proIAPP during amyloid formation 104 4.3 DISCUSSION 108 4.3.1 Structure of native proIAPP 108 4.3.2 Formation of amyloid from proIAPP 108 4.3.3 Structural changes of proIAPP during amyloid formation 110 CHAPTER 5: THE EFFECT OF CLUSTERIN ON ProIAPP AMYLOID FORMATION AND CYTOTOXICITY 5.1 CYTOTOXICITY ASSOCIATED WITH AMYLOID FORMATION 112 5.1.1 The effect of IAPP amyloid formation on -cell destruction 112 5.1.2 Amyloidogenic intermediates are the toxic species 113 5.1.3 The ion channel hypothesis 113 5.1.4 The role of Ca2+ in cytotoxicity 115 5.1.5 Modulators of pore formation 116 5.1.6 The oxidative stress hypothesis 117 5.1.7 Association of ROS with Ca2+ influx 119 5.1.8 Cell death may occur by apoptosis or necrosis 120 5.2 THE ROLE OF CHAPERONES IN AMYLOID DISEASES 120 5.2.1 Clusterin and Alzheimer’s disease 120 5.2.2 Clusterin and other amyloidoses 123 5.2.3 Clusterin and Type 2 diabetes 124 5.2.4 Aims of this study 124 5.3 RESULTS 5.3.1 The effect of clusterin on amyloid formation measured by ThT assays 126 5.3.2 Analysis of proIAPP and clusterin mixtures by transmission electron microscopy 128 5.3.3 The binding of clusterin to freshly redissolved proIAPP measured by direct ELISA 131 5.3.4 The binding of clusterin to freshly redissolved proIAPP by competition ELISA 133 5.3.5 The binding of clusterin to different denatured proteins in the presence of proIAPP at pH 7.4 137 5.3.6 The binding of clusterin to different denatured proteins in the presence of proIAPP at pH 5.5 141 5.3.7 Time course of binding of clusterin to denatured lysozyme in the presence of proIAPP 144 5.3.8 The effect of clusterin on proIAPP amyloid formation monitored by CD spectropolarimetry 5.3.9 The formation of complexes between clusterin and proIAPP 147 148 5.3.10 Dot-blotting for clusterin in soluble and insoluble fractions of proIAPP and clusterin mixtures 5.3.11 Binding of clusterin to mature proIAPP fibrils 153 158 5.3.12 Clusterin bound to proIAPP fibrils detected by immunoelectron microscopy 160 5.4 THE EFFECTS OF CLUSTERIN ON ProIAPP CYTOTOXICITY 5.4.1 The experimental design of cytotoxicity experiments 163 5.4.2 Cytotoxicity of different proIAPP species to a RIN-m5f cells 165 5.4.3 The concentration-dependence of proIAPP cytotoxicity 168 5.4.4 The effect of clusterin on proIAPP cytotoxicity 168 5.4.5 The cytotoxicity of proIAPP species formed in the presence of clusterin 170 5.5 DISCUSSION 5.5.1 The effects of clusterin on proIAPP amyloid formation 174 (a) The inhibition of amyloid formation 174 (b) ELISA measurements of the binding of clusterin to proIAPP 174 (c) Zone electrophoresis analysis 175 (d) CD analysis 176 (e) The interaction between clusterin and soluble proIAPP species 176 (f) The binding of clusterin to insoluble proIAPP species 178 5.5.2 The effects of clusterin on proIAPP-mediated cytotoxicity 180 5.5.3 The role of clusterin in Type 2 diabetes 182 CHAPTER 6: THE EFFECTS OF GLYCOSAMINOGLYCANS ON ProIAPP AMYLOID FORMATION 6.1 INTRODUCTION 6.1.1 The localization of proteoglycans to amyloid deposits 183 6.1.2 The accumulation of proteoglycans in amyloid diseases 184 6.1.3 The role of proteoglycans in amyloid formation 185 6.1.4 GAGs may increase the stability of amyloid 186 6.1.5 Conformational changes induced by GAGs 187 6.1.6 Determinants of GAG binding to amyloidogenic peptides 188 6.1.7 The effect of GAGs on the rate of amyloid formation in vitro 191 6.1.8 GAGs and proIAPP 192 6.1.9 Aims of this study 194 6.2 RESULTS 6.2.1 The effect of GAGs on proIAPP amyloid formation 196 6.2.2 The effect of GAGs on the secondary structure of proIAPP 198 6.2.3 The concentration-dependence of heparin-induced conformational changes in proIAPP 201 6.2.4 The concentration-dependence of heparin-induced amyloid formation at pH 7.4 and 5.5 6.2.5 The mechanism of the heparin enhancement of ThT fluorescence 203 206 6.2.6 Metal cation dependence of heparin-induced amyloid formation 208 6.2.7 The effect of heparins of different molecular weights on formation of amyloid from proIAPP 210 6.2.8 The effect of heparin disaccharides on heparin-induced proIAPP amyloid formation 213 6.2.9 The effect of heparin on the exposed hydrophobic surface of proIAPP measured by bis-ANS fluorescence 216 6.2.10 Changes in the fluorescence of bis-ANS bound to proIAPP during heparin-induced proIAPP amyloid formation 218 6.2.11 The binding of soluble proIAPP to heparin-agarose 221 (a) The binding of proIAPP to heparin-agarose in 10 mM sodium phosphate, pH 7.4 (b) The binding of proIAPP to heparin-agarose in PBS, pH 7.4 222 223 6.2.12 Conformational changes of proIAPP induced by heparin in 10 mM sodium phosphate, 150 mM NaF, pH 7.4. 6.2.13 Incorporation of FITC-heparin into proIAPP fibrils 224 227 6.3 DISCUSSION 6.3.1 The effect of different GAGs on proIAPP amyloid formation 230 6.3.2 The minimal subunit of heparin necessary for proIAPP binding 231 6.3.3 The effect of buffers of differing ionic strength on heparin-induced conformational changes in proIAPP 6.3.4 The effect of heparin on the final ThT fluorescence of proIAPP amyloid CHAPTER 7: REFERENCES 232 234 237