Dear (Senator): - American Society of Diagnostic and Interventional
advertisement

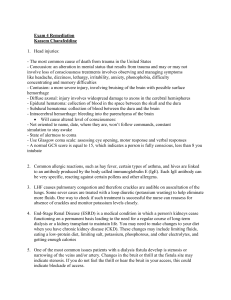
Dear (Senator): For years patients with End Stage Renal Disease (ESRD) receiving dialysis in the United States have had the highest mortality rate in the world. Patients on hemodialysis require a mechanism to get blood from their bodies, into the dialysis machine and back. To accomplish this surgically created conduits called grafts, catheters and fistulas are created. In the US a much higher proportion of patients have grafts and catheters placed rather than fistulas. Fistulas are recognized to be superior and to be associated with a sharply lower mortality rate. To this end all major organizations dealing with ESRD have funded and promoted programs to urge and facilitate the augmentation of fistula prevalence in the US. These supporting organizations include the American Society of Nephrology, the Renal Physicians Association, the National Kidney Foundation, the Fistula First Initiative, the American Society of Diagnostic and Interventional Nephrology. One of the most important accomplishments of these efforts has been the emergence of specialty centers or Access Centers, which deal exclusively with diagnosis and management of problems occurring in dialysis access. The majority of these Access Centers are operated by nephrologists, the specialty physicians exclusively charged with the management of dialysis patients. The centers are operated largely as extensions of the physicians office practices and capitalized by them. Prior to the establishment of this effort and these centers, the national prevalence of fistulas was 20 %. With the acceleration of this effort has been a national rise in the prevalence of fistulas of 10 % with many of the largest practices in the US achieving a rate of 60 %. As a partner in this effort, CMS has recently facilitated reimbursement for these centers resulting in nephrologists around the country to own or partner as owners of Access Centers. Thus in the foreseeable future the majority of ESRD patients in the country will have access to these centers. Unfortunately, the House version of the Children’s Health and Medicare Protection Act of 2007 (H.R. 3162) has provisions in it which will force the closure of many of these centers and prohibit all but the largest practices in the country from establishing and operating them. Severe limitation of access to these centers for ESRD patients will undoubtedly result. The effort to promote fistula creation will be severely impacted. This legislation includes language promoting a "fix" to the sustainable growth rate (SGR) method of calculating physician reimbursement that would cause a major loss of access for Medicare beneficiaries to many types of minimally invasive therapies which are used in the maintenance of dialysis vascular access. We believe that the legislative repair being proposed would stymie the development of targeted, less-invasive and more cost-effective therapies by creating financial disincentives for such treatments. This current piece of legislation does not recognize the difference between older, more invasive, less targeted therapies (whether major surgeries or minor procedures) and the newer, less invasive, highly targeted therapies that have promoted the increase in fistula prevalence. This legislation divides physician services into different categories - and thus physicians; enacting 6 different conversion factors based on these categories or "buckets". The proposed buckets and projected changes in reimbursement (not including an adjustment for inflation) are as follows: 1:Primary and preventive 49% 2:Other E/M -5% 3:Surgery 8% includes only 10-day and 90-day "major" surgery 4:Other procedures -21% includes all 0-day global, minimally invasive surgeries 5:Anesthesia 37% 6:Imaging -21% *with adjustment for inflation, both "other procedures" and "imaging" are expected to result in a 40% decrease in reimbursement for these buckets. The long-term SGR "fix" being proposed is not sufficiently well-constructed, and its true ramifications are incompletely evaluated. Our great concern is that the Congress is "incentivizing" open surgery (without regard to its effectiveness, total costs and patient benefits) over minimally invasive alternative treatments (again without consideration of the differences among the myriad services included in this category). A subcommittee has attached this "added" piece of legislation, which we do not believe is capable of standing by itself, to a matter of critical importance for the children of our nation. While it is difficult to argue against improving the health of our children, this legislation would severely and negatively impact the access to health care for all patients with ESRD in the United States. This section has been included in the version of this legislation in the House of Representatives but not the Senate. Should it pass we urge you to work to eliminate it from the conference bill.