Microsoft Word - PRT Report
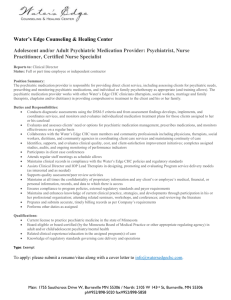
advertisement
Report of the CPNP Taskforce on Psychiatric Pharmacy Accreditation Standards Recommended Structure of Residency Programs in Psychiatric Pharmacy CPNP acknowledges the continued evolution of pharmacy practice and the importance of having adequately educated and trained pharmacists to fulfill the vision of pharmacists being health care professionals that have a primary responsibility for patient pharmacotherapy outcomes. This is particularly important in psychiatric pharmacy where medications are not only a core component of overall mental health care, but inappropriate medication use leads to poor outcomes for individuals with psychiatric disorders. Increasingly, the biological basis for the etiology and pathophysiology of psychiatric disorders is being elucidated, and this is leading to more sophisticated and often times more invasive means of treatment. Furthermore, it is increasingly important for psychiatric pharmacists to have in-depth knowledge and skills not only in the treatment of psychiatric disorders, but in medical disorders that occur concurrently with psychiatric disorders, and in monitoring and intervening with medication adverse effects affecting multiple body organ systems. With these points in mind, CPNP supports a long-term vision of psychiatric pharmacy residencies being two-year programs that integrate accomplishing the goals and objectives for PGY-1 pharmacy practice residencies with those of PGY-2 residencies in psychiatric pharmacy. This may or may not be accomplished at the same institution. However, in the short-term this goal may not be achievable in all mental health environments that are capable of providing exemplary training in psychiatric pharmacy practice. Many mental health practice settings are isolated from health care environments that provide primary or specialty medical services. Thus, while these practice settings may have the psychiatric pharmacists and other professionals necessary to provide excellent psychiatric pharmacy services and mental health care, they may not have the practice environment and health care professionals to meet the goals and objectives for PGY-1 pharmacy practice residencies. In other practice settings, either financial considerations or other logistical concerns may not allow the provision of integrated PGY-1/PGY-2 residency programs in the immediate or near future. CPNP recommends that the ASHP Commission on Credentialing accredit psychiatric pharmacy programs as: PGY-2 psychiatric pharmacy 1-year residencies that meet the core educational outcomes described below, and PGY-1/PGY-2 integrated 2-year programs that meet PGY-1 pharmacy practice educational outcomes as well as the educational outcomes for psychiatric pharmacy residencies listed below Core Educational Outcomes for a PGY-2 Psychiatric Pharmacy Residency Program Provide evidence based pharmacotherapy for individuals with psychiatric and neuropsychiatric disorders across various patient populations. 1. Demonstrate knowledge regarding the pathophysiology, pathogenesis, epidemiology, and diagnostic criteria of psychiatric disorders. 2. Discuss and apply knowledge regarding psychotropic medications, including pharmacodynamics, pharmacokinetics, indications, dosage, monitoring, clinical outcomes, drug interactions, and adverse effects. 3. Discuss and apply knowledge regarding nonpharmacologic therapies and their role in the treatment of psychiatric disorders. 4. Demonstrate proficiency in critically evaluating research evidence in the literature and applying this information to direct patient care. 5. Evaluate a patient's clinical status including performing a history, mental status assessment, utilization of clinical rating tools, and assessment of medical problems. 6. Identify medication specific problems in individual patients. 7. Recommend, implement, monitor, and provide appropriate follow-up on a pharmacotherapeutic plan in patients with psychiatric disorders with or without co-occurring medical disorders or other psychiatric disorders. 8. Effectively communicate with health care professionals, patients, and families both verbally and in writing. 9. Identify and incorporate cultural, genetic, economic, and other significant factors into the pharmacotherapeutic care of patients. 10. Use informatics systems in the provision of patient care. 11. Identify barriers that interfere with patient adherence to treatment, and formulate plans to overcome these barriers. 12. Discuss important ethical issues with regard to the provision of care to psychiatrically ill patients and demonstrate application of these principles in professional practice. Evaluate and improve the medication use process in mental health systems 13. Evaluate a therapeutic class of psychotropic medications for inclusion of a new medication on a formulary or treatment guideline. 14. Evaluate and discuss different drug distribution systems in the cost effective and safe delivery of medications to patients with psychiatric disorders. 15. Develop, implement, and evaluate medication use criteria for patients with psychiatric disorders. 16. Use informatics systems in the efficient and safe delivery of medications to patients, including their use in medication monitoring, and in detecting adverse events and medication errors, and in medication use evaluation. Exercise exemplary leadership and clinical management skills in psychiatric health systems 17. Demonstrate working knowledge of the effects of accreditation, statutory, regulatory, legal, ethical, and safety requirements on mental health care and psychiatric pharmacy practice. 18. Effectively work as a member of a team to develop, improve, or implement a new service or policy in a mental health care setting. 19. Participate in professional organizations, committees, and meetings that are of importance to psychiatric pharmacy and the pharmacotherapeutic care of individuals with psychiatric disorders. Participation should be at several levels (local, regional, and national) when appropriate opportunities are available. Demonstrate project management skills in a mental health setting 20. Initiate, design, implement, evaluate, and complete a practice-related project involving psychiatric pharmacy, present this project at a meeting relevant to psychiatric pharmacy, and submit the findings for consideration of publication. 21. Discuss important ethical issues with regard to conducting human research in mentally ill patient populations, including Good Clinical Practice, IRB policies and procedures, HIPAA, and applicable state mental health statutes and rules. Provide effective education to health care providers, students, trainees, and consumers 22. Design or revise patient or family medication education materials for persons with psychiatric disorders. 23. Effectively prepare educational programming directed at students, trainees, and health system staff. 24. Conduct individual and group patient and family or caregiver education. 25. Successfully mentor or supervise pharmacy students or other trainees in the mental health system.