Microscopic Features of Kidney
advertisement

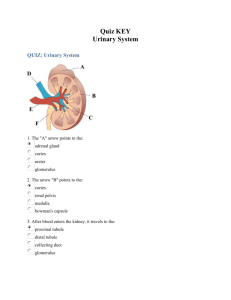
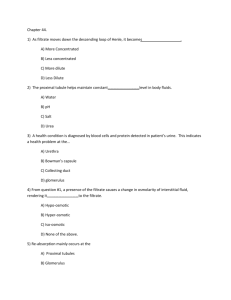
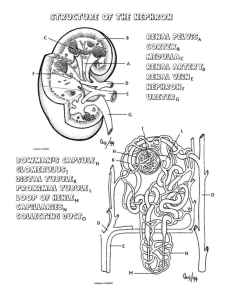
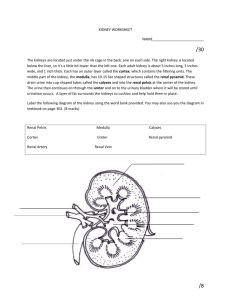
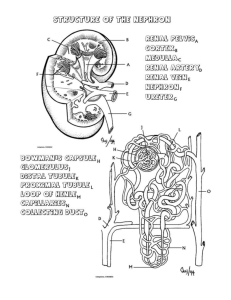
LEARNING OBJECTIVES/ LECTURE OUTLINES (Microscopic features of kidney) • Identify the cortex, medulla, calyces, pyramids, renal papillae and ureter in a diagrams or section of a kidney. • Explain with labeled diagrams the organization of a renal corpuscle. • Specify the kidney components involved in producing urinary filtrate and state the role of each component. • Name the major parts of a nephron. • Recognize the proximal and distal convoluted tubules and thin-walled parts of loops of Henle in section. • State where juxtaglomerular cells are located and discuss their significance. Describe the sequence of the blood vessels supplying the kidney beginning with the renal artery and ending with the renal vein Kidneys are reddish brown paired organs, situated along the posterior abdominal wall. They are covered by thin capsule, which is easily removed The cut surface shows outer cortex and internal medulla. Inside the medulla there is renal sinus containing cup shaped major and minor calycies The renal medulla consists of pale, striated, conical renal pyramids. Their bases are peripheral while their apices converging to the renal sinus where they project into minor . Each pyramid is capped by cortical tissue to form renal lobe. The renal cortex is subcapsular; it also extends towards the renal sinus as renal columns. The medullary tissue extends into the cortex as medullary rays. Cortex close to the medulla is sometimes termed juxtamedullary cortex. Microscopic Features • Kidney is composed of many tortuous closely packed uriniferous tubules, bound by little connective tissue in which run blood , lymphatics and nerves. • Each uriniferous tubule consists of two embryologically distinct parts. 1. The secreting Nephrons which elaborate urine and 2. Collecting tubule which convey urine to the calyceal system. Kidney and Urineferous Tubule • Each kidney consists of about 1,000,000 nephrons, • The nephrons begins as double walled epithelial cup (Bowman’s capsule), which surrounds a tuft of capillaries, the glomerulus. • Bowman’s capsule and the glomerulus together form the renal or Malpigian corpuscle. Bowman’s capsule consists of two simple epithelial layers; an inner or visceral layer covering the glomerulus and an outer parietal layer. The region where the vessels enter or leave the glomerulus is the ‘vascular pole of the corpuscle. ‘Urinary pole’ of the corpuscle is roughly opposite the vascular pole; here the parietal layer of Bowman’s capsule becomes continuous with proximal tubule. The Nephron and Renal Corpuscle The cells of the visceral epithelium are specialized, called ‘podocytes’. The nucleus and surrounding cytoplasm protrude into the capsular space and rests on the processes that extend from the cell body, branching one or more times to form a series of slender processes on basal The terminal processes or pedicles interdigitate with the pedicles of neighboring podocytes; leaving a series of slits between them. Parietal Layer of Bowman’s capsule Parietal layer of bowman’s capsule is lined by simple squamous epithelium. This layer becomes continuous with the lining of proximal convoluted tubule. Tubular Part of Nephron The tubular portion of nephrons is composed of Both proximal and distal tubules have a convoluted portion and a straight portion. The straight portion of the proximal tubule and distal tubule together with the thin segment are arranged in a hairpin loop extending a variable distance into the medulla. These three segments together are called The convoluted portion of the distal tubule joins the arched collecting tubule which begins system of the ducts or ‘ collecting tubules’. The proximal tubule is the longest section of the nephron (about 14 mm). The convoluted part of the proximal tubules coils close to the glomerulus in the cortex. The diameter of proximal tubules is ~65 µm. Their walls are formed by a low columnar epithelium. The eosinophilic cells of the epithelium have a wide brush border They almost completely reabsorb substances of nutritional value from the glomerular filtrate (glucose, amino acids, protein, vitamins etc). In the proximal tubules the volume of the glomerular filtrate is reduced by about 75%. Sodium ions are actively resorbed from the glomerular filtrate. They are followed by passively diffusing chloride ions and the osmotic absorption of water. The straight portion of the proximal tubule descends towards the medulla. The straight portion of the proximal tubule merges with the intermediate tubule the thin segment of the A flattened, only ~1-2 µm high epithelium (simple squamous) forms the intermediate tubule, which is The diameter of the distal tubule expands to ~35 µm. The distal tubule, is formed by low cuboidal cells without a brush border. Basal infoldings and all the cell organelles are present. Function of Distal convoluted tubule Epithelial cells in distal tubules cells transport chloride (active) and sodium ions (passive) into the surrounding peritubular space. Cells in the distal tubules are sensitive to the hormone aldosterone. Juxta-glomerular Complex The distal tubule contacts the glomerulus forming a specialized section of tubular epithelium, the macula At the point of contact with the glomerulus, the distal tubule is always in close contact with the efferent and afferent arterioles of the glomerulus. The juxtaglomerular cells surround the afferent arteriole (they are modified smooth muscle cells), which produce and secrete renin. Third component of the juxtaglomerular complex is extra-glomerular mesangial cells Renin activates angiotensinogen, a precursor found in the blood stream, leading to the formation of Angiotensin I is converted to angiotensin II. Angiotensin II is the most potent vasoconstrictor known. Renin also stimulates the secretion of aldosterone Blood supply of kidney Renal artery is a branch of abdominal aorta. Near the hilum it divides into anterior & posterior branches. These branches further divide into segmental arteries‡ apical upper, middle lower & posterior. 1. Interlobar arteries 2. Arcuate arteries 3. Interlobular arteries 4. Afferent arteriole 6. Efferent arteriole Cortical and medullary capillaries →interlobular vein →arcuate vein→renal vein The minor calyces merge to form major calyces within the kidney. Major calyces in turn merge to form the renal pelvis (still within the kidney). The urine flows through these structures to the ureter and is channeled to the bladder. The basic structure of all these components is the same. There are three layers in the wall: The mucosa is lined with a transitional epithelium, the epithelium is virtually impenetrable to any components of the urine. Part of Wall of Ureter 1. The lamina propria of the mucosa consists mainly of dense connective tissue, with many bundles of coarse collagenous fibers. 2. The muscularis usually consists of an inner longitudinal and outer circular layer of smooth In lower parts of the ureter and the bladder an additional outer longitudinal layer of muscles is added to Outermost layer is adventitia, as throughout its course it lies retroperitoneally. Part of Wall of Ureter a) Transitional epithelium b) Lamina propria 3) Serosa/adventitia Transitional epithelium 3---6 layers of cells, Basal: cuboidal/low columnar, Intermediate layer: Polygonal Superficial: Umbrella shaped may be binucleate Plasmalemma; unusually thick due to membrane internalization Impermeable, with occluding junction When the epithelium is stretched, as when the bladder is full of urine, the epithelium is only three or four cells in thickness, and the superficial cells become squamous. The superficial cells of the transitional epithelium have a special membrane of thick plates separated by narrow bands of thinner membrane. When the bladder contracts, the membrane folds along the thinner regions, and the thicker plates invaginate to form fusiform cytoplasmic vesicles. These vesicles represent a reservoir of these thick plates that can be stored in the cytoplasm of the cells of the empty bladder and used to cover the increased cell surface in the full bladder. Lamina propria consists of connective tissue, vessels n nerves. Muscle layer (detrusor muscle) consists of inner and outer longitudinal layers of smooth muscles and The urethra is a tube that carries the urine from the bladder to the exterior Towards the neck of bladder the smooth muscle fibers form the internal urethral sphincter, which leads The female urethra is a tube 4-5 cm long, lined with stratified squamous epithelium and areas of Pseudostratified columnar epithelium. • In females, mucosa is surrounded by a layers of circular smooth muscle. • The mid part of the female urethra is also surrounded by an external striated voluntary In male, three divisions: 1. Prostatic urethra, 2. Membranous urethra, 3. Spongy or penile urethra. In males urethra also discharges semen 1- Prostatic Part of Urethra In the dorsal and distal part of the prostatic urethra, there is an elevation, the verumontanum (from Latin, meaning mountain ridge), that protrudes into its interior. A closed tube called the prostatic utricle opens into the tip of the verumontanum; this tube has no The ejaculatory ducts open on the sides of the verumontanum. The seminal fluid enters the proximal urethra through these ducts to be stored just before ejaculation. The prostatic urethra is lined with transitional epithelium 2- Membranous Urethra The membranous urethra extends for only 1 cm and is lined with stratified or pseudostratified columnar Surrounding this part of the urethra is a sphincter of striated muscle, the external sphincter of the 3-Penile or Spongy Urethra The Penile or spongy part of the urethra is located in the corpus spongiosum of the penis. The urethral lumen dilates distally, forming the fossa navicularis. The epithelium of this portion of the urethra is mostly pseudostratified columnar, with stratified Littre's glands are mucous glands found along the entire length of the urethra but mostly in the spongy The secretory portions of some of these glands are directly linked to the epithelial lining of the urethra; others have excretory ducts. Their function is lubrication of urethra. Image of urinary system