First Year
advertisement

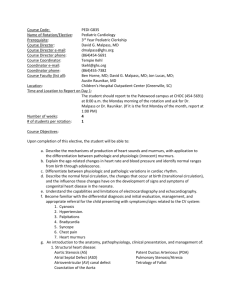
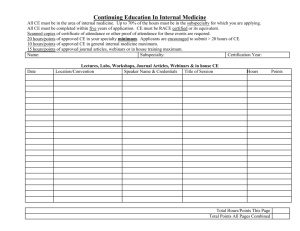
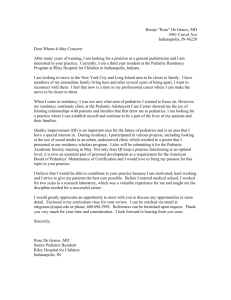
DESCRIPTION OF THE TRAINING PROGRAM IN PEDIATRIC CARDIOLOGY (revised 6/2006) (University of Miami/Jackson Memorial Hospital, Miami, FL) BACKGROUND The Division of Pediatric Cardiology is an integral part of the Department of Pediatrics. It obtained divisional status in June 1973. University of Miami/Jackson Memorial Medical Center (Overview) UM/JMH medical center is the sponsoring institution with responsibility for the pediatric residency program and the program in pediatric cardiology. The medical center is a 1500 bed tertiary care facility which serves as a regional and international referral center for patients requiring complex and sophisticated medical care. There is a transcultural and socially diverse group of patients providing a unique exposure for the pediatric cardiology resident. The Transplant Center is one of the major transplant centers in the nation and performs a large volume of solid organ transplants including heart and lung. The Children’s Hospital Center (part of the UM/JMH center) is a facility with 253 beds dedicated to Pediatrics, including 66 to newborn intensive care, 60 intermediate and 100 to normal newborns. There are 21 beds dedicated to pediatric intensive care. The new pediatric intensive care unit (1/2 completed) will have a total of 30 beds with 10 dedicated to cardiovascular patients. The pediatric emergency room services over 29,000 patients yearly. PROGRAM GOALS (General) The educational mission of the Pediatric Cardiology Training Program is to provide subspecialty residents with broad clinical experience, factual knowledge, technical skills, and clinical judgment to effectively manage patients from fetal life to adulthood for congenital and acquired heart disease to enhance their skills and to promote their involvement in research. This is achieved by a progressive delegation of increasing responsibility in the clinical area, non-invasive laboratories and invasive laboratories; delegation of teaching roles; and exposure and participation in research. The trainees will receive didactic instruction, clinical exposure to patients with mild and serious heart disease in both surgical and medical settings and assignments for didactic teaching and research projects. This experience is enhanced by incorporation of support services, social, ethical and preventive aspects. General description of each year of training First Year: The subspecialty resident receives 2 months of clinical inpatient service and 1 month of cardiac ICU. It includes responsibilities for medical and surgical patients as well as consultations. There are 2 months of non-invasive experience which includes treadmill and other stress studies and tilt studies. There are 3 months of rotation in imaging which includes twodimensional, color flow imaging, spectral Doppler, M-Mode and contrast echo, as well as transesophageal echo and stress echocardiography. This may also include fetal echo. There are 2 months cardiac catheterization/electrophysiology and 1 month of protected research. Second Year: Two months of clinical service and 1 month of cardiac ICU and 2 months of rotation in imaging. There are 2 months of cardiac catheterization/electrophysiology, 1 month non-invasive and 3 months of protected research time. Third Year: There are 2 months of clinical inpatient service, 1 month rotation in imaging, 2 months of cardiac catheterization and 6 months of protected research time. Summary of Content of Pediatric Cardiology Subspecialty Training Program First Year Second Year Third Year 1. Clinical: a. Frequency of night call b. Number of clinical rounds 10 months* Every 3-4th night 7 per week for 3 mo. 9 months** Every 4-5th night 7 per week for 3 mo 5 months*** Every 5th night 7 per week for 3 mo 2. Research: a. Clinical b. Laboratory c. Frequency of night call 1 month 2-3 months 5-6 months Every 3-4th night Every 3-4th night Every 4-5th night NOTE: In-house call coverage is shared by all cardiac fellows. The “service fellow” does not normally have in-house call. During the months when cardiac ICU coverage is provided by the Pediatric Critical Care fellow, there are several days when the service fellow will take “back-up” call from home. In addition, fellows on other rotations rotate with the service fellow on backup call. Otherwise, the in-house call person takes the night call from 5:30 pm to 7:00 am on week days and from 7:30 am to 7:30 am on weekend days. Summary of Clinical Inpatient experience Our daily pediatric cardiology census consists of 6-10 patients in addition to the consult service of 6-10 patients daily. Medical and surgical patients are cared for in the general pediatric areas, the critical care unit and the newborn intensive care unit. There are 16 semi-private rooming-in beds equipped with state-of-the-art remote monitoring. Annual number of inpatient visits was 4000. Operating rooms are specifically designed for management of infants and children with congenital , acquired heart disease and transplant. Each pre-operative patient is evaluated by a team consisting of a cardiovascular surgeon, attending pediatric cardiologist, subspecialty resident, and anesthesiologist. The Cardiology subspecialty resident is responsible for the evaluation of the patient along with the cardiac surgical resident and is further responsible for the review of the past history, non-invasive studies, cardiac catheterization and angiographic data. Each patient is reviewed at a formal CV conference. The surgical experience includes a total of 2 months of concentration on surgical patients where responsibilities include observation in the operating room and performance of transesophageal echocardiograms and experience in the critical care unit for management of post-operative patients in conjunction with the surgical and cardiac intensive team. The subspecialty residents are also responsible for pre-operative evaluation, operative observation and post-operative follow-up of cardiac transplant patients. They are expected to be familiar with the various immune suppressive agents and proper management. The pediatric heart transplant program was established in 1991. It is complimented by a strong Division of Transplantation with extensive immunologic support. For those inpatients for whom consultations have been provided, it is expected that the resident will follow these patients closely and be familiar with the various underlying problems that impact the cardiac status, for example: neonates with persistent fetal circulation, diaphragmatic hernia, hyaline membrane disease; pulmonary patients with chronic lung disease and asthma, nephrology patients with hypertensive heart disease, end-stage renal disease and lupus erythematosis; hematological patients with sickle cell anemia, leukemia, and drug induced cardiomyopathy; gastroenterology patients, post liver transplant and infectious disease patients with AIDS cardiomyopathy and endocarditis. All of these patients are the responsibility of the subspecialty resident in conjunction with faculty oversight. The neonatal intensive care unit is a busy service where a special unit is identified for babies with cardiac disease. The responsibility for the evaluation and management of these babies rests upon the cardiac resident and neonatal resident with faculty supervision. These infants are followed regularly by the cardiology service along with the neonatal service for decisions regarding management and care. The subspecialty resident is responsible for all consultations on the newborn unit. Supervision: Every patient is reviewed and examined by a faculty member after the evaluation or conjointly with the evaluation by the resident. Our consultation and follow-up visits are recorded on specially designed consultation and progress forms divided for entries by the subspecialty resident and the faculty member. Rounds: There are daily rounds with the faculty member and the hours vary from 2 to 6 depending upon the census. Logs: Hospital accreditation committees often require a log of patients evaluation and diagnosis. At least 1 month of such encounters should be entered into a database for future reference. Summary of Clinical outpatient experiences There are approximately 4000 outpatient visits yearly. Residents are required to attend, evaluate and manage outpatients in the following clinics: weekly general cardiac clinic at Jackson Memorial Hospital and weekly State supported clinic. All of the subspecialty residents attend the general cardiac clinic. Each is responsible for one state supported clinic monthly. The resident is assigned to the same State supported clinic monthly. These outpatient experiences are throughout the year and provide for longitudinal follow-up. For patients who have been followed in the hospital, there is an appointment system and a database system maintained in our Division, which allows channeling of these patients to the specific subspecialty resident. All of the residents are supervised by faculty and each patient is evaluated by the faculty member with appropriate chart documentation. Residents are responsible for consulting on patients in the emergency room and this accounts for approximately 60 consultations per year. The emergency department is located in our primary teaching hospital, Jackson Memorial Hospital. There is faculty oversight on location for 90% of the patients seen in the Emergency room with faculty oversight off location for 10% (phone, fax of EKG, etc). Additionally, those residents who are rotating on the non-invasive service have the opportunity and responsibility to attend the arrhythmia and pacemaker clinic weekly where approximately 200 children with pacemakers and defibrillators are followed. This is primarily a learning experience for the fellows initially, but, as experience is gained in the use of pacemakers and defibrillators, more responsibility is given to the trainees. All clinics are with faculty oversight. CONFERENCES PEDIATRIC CARDIOLOGY SUBSPECIALTY PROGRAM Conference R/O Frequency 1. Specific cardiac defects/Journal Club R W 2. EP/EKG R 3. Cardiovascular Conference R 4. Echocardiographic Conference Person(s) responsible for conducting conference Hospital 1, 2, 3 Fellow Presentations 1 Fellows Quizzed 1 W Presents Cases and Hemodynamics 1 R W Fellows Quizzed 1 5. Pathology/M & M R M Observers & Q/A 1 6. Guest/Special Problems R 2xM Open Questions 1 7. Pediatric Grand Rounds O W Open Questions 1 8. Pediatric Staff Conference O 3xM Open Questions 1 9. Pediatric Mortality/Morbidity O M Open Questions 1 10. Embryology Course O Y Attends Formal Course 1 11. Research Seminar R Y Presentation & Exhibition 1 12. Scholarship Oversight R Report Progress 1 13. Research Lectures R M Participation Q/A 1 14. Modified Clinical Scientist Training Program R W Participation Q/A 1 2xM M R = Required O = Optional LIBRARY FACILITIES UM/JMH: Internet access for literature searches is available within the resident’s office, located within the divisional office. In addition, the Louis B. Calder Memorial Medical Library is located on the medical complex, with access to all hospital and university employees. The hours of operations for the library are: Monday - Thursday, 7:30am - 12:00 am Friday, 7:30am - 8:00pm Saturday, 8:00am - 8pm Sunday, 12:00pm - 12:00am This library is a full service library, with interlibrary loan and document delivery services available. In addition, there is an extensive collection of textbooks, journals, and audiovisual materials. Computer workstations with internet access are available. Teaching Staff (Interaction with Subspecialty Resident): a. Evaluation of subspecialty residents: Interaction with the faculty member on various rotations for informal discussions and suggestions throughout the duration of the various rotations (example, cardiac catheterization, non-invasive, service). An evaluation is provided at the end of the rotation, a copy of which is kept in the record and a copy is given to the trainee. The Division Director is available for discussion in addition to the other faculty members. There are twice yearly formal assessments by all faculty members and the Division Director meets with each fellow on a twice yearly basis for discussion of these evaluations. The residents and Division Director discuss the reviews and these are signed by the resident. These records are retained on file. Logs of numbers of catheterizations, echocardiograms, consultations, tilt studies, stress studies, etc. are reviewed. It is required that these logs be updated on a regular basis. There is a yearly in-training examination and all residents are expected to take the exam. There is an exit summary and interview prior to the termination of the training period. This exit summary includes highlights of the training period as well as a review of the various procedures performed. Comments are solicited regarding the strengths and weaknesses of the progress. WELCOME LETTER FROM DIRECTOR Date: Dear Dr. : It is with great pleasure that we offer you a Pediatric Cardiology Fellowship position in the Department of Pediatrics, Division of Pediatric Cardiology for the academic year beginning July 1, 200_ and ending June 30, 200_. You will be designated as a PGY-4 earning a corresponding stipend of $ . This offer is contingent upon the completion of satisfactory reference check, background check, employee physical and alcohol/drug testing as well as proof of a medical/osteopathic doctorate degree, proper immigration status/work visas/permits, if applicable, and proper licensing by the State of Florida. As a Pediatric Cardiology Fellow, the terms and conditions of your fellowship are detailed in the Collective Bargaining Agreement with the Committee of Interns and Residents, the Jackson Health System (JHS) Administrative Policy and Procedure Manual, and the Residents and Active Academic Attending Responsibilities manual. Enclosed is a copy of the JHS policy on Sexual Harassment and a copy of the Residents and Active Academic Attending Responsibilities. The Collective Bargaining Agreement and the JHS Administrative Policy and Procedure Manual may be reviewed online at http://www.um-jmh.org/chapter.cfm?id=69. We hope you find this offer to be satisfactory and await confirmation of your acceptance. Please sign and return this letter as acceptance of this conditional offer of employment. Sincerely, Gerard A. Kaiser, M.D. Executive Vice President Chief Medical Officer By my signature below, I accept this offer of employment as it has been described in this letter and enclosures. I understand that if the reference check, background check, physical examination or alcohol/drug test produce an unsatisfactory result, or if I do not produce proof of my medical/osteopathic degree, appropriate immigration status/work visa/permit or proper licensing with the State of Florida, that this offer will be revoked. _______________________ Signature ____________________ Date CONTACT INFORMATION: Grace S. Wolff, M.D. Director, Pediatric Cardiology Training Program University of Miami Miller School of Medicine Diane L. McMullen Training Program Coordinator Pediatric Cardiology Mailing Address: P.O. Box 016960 (R-76) Miami, FL 33101 Street Address: 1611 N.W 12th Avenue Holtz Center, Room 5043 Miami, FL 33136 Telephone: FAX: E-mail: 305-585-6683 305-324-6012 gwolff@med.miami.edu dmcmulle@med.miami.edu Department of Pediatrics WebSite: http://pediatrics.med.miami.edu/ POLICIES AND PROCEDURES DIVISION OF PEDIATRIC CARDIOLOGY 1. Selection of Candidates All applications are reviewed by several faculty members and ranked for interview. The majority of the faculty members interview each candidate and rank these candidates. A meeting is held and the ranking is reviewed and selection in rank order is identified and submitted to the National Residency Matching Program (NRMP). 2. Training Requirements We follow those outlined by the American Board of Pediatrics for Sub-Specialty Certification. GENERAL ELIGIBILITY CRITERIA FOR CERTIFICATION IN THE PEDIATRIC SUBSPECIALTIES (AMERICAN BOARD OF PEDIATRICS 2006) In addition to the training requirements, which are specific to each of the pediatric subspecialties, the following are required of candidates seeking certification in the pediatric subspecialties of adolescent medicine, cardiology, critical care medicine, developmental-behavioral pediatrics, emergency medicine, endocrinology, gastroenterology, hematology-oncology, infectious diseases, neonatal-perinatal medicine, nephrology, pulmonology, and rheumatology. Each candidate must be familiar with specific subspecialty training requirements as well as the policies stated in the current Booklet of Information. Certification by the American Board of Pediatrics (ABP) An applicant must be currently certified in general pediatrics to be accepted for a pediatric subspecialty certifying examination. Applicants whose time-limited certification will expire before the examination must complete the requirements for maintenance of certification at least 5 months before the examination date. Licensure An applicant must have a valid (current), unrestricted license to practice medicine in one of the states, districts, or territories of the United States or a province of Canada in which he or she practices or have unrestricted privileges to practice medicine in the US Armed Forces. If licenses are held in more than one jurisdiction, all licenses held by a physician should meet this requirement. An applicant who is practicing the subspecialty abroad exclusively may be exempted from this license requirement upon presentation of proof of licensure in the country in which he or she practices. Candidates who practice or plan to practice abroad exclusively must submit a letter, in addition to the licensure, stating this fact. A copy of the license must accompany the application material. POLICIESAND PROCEDURES (continued) DIVISION OF PEDIATRIC CARDIOLOGY Verification of Training An applicant will be asked to list the program(s) where fellowship training occurred as well as the name(s) of the program director(s). The ABP will provide a Verification of Competence Form to the program director(s) for completion. (Note: For new subspecialties, alternatives to the usual training requirements, such as practice experience, will be acceptable as criteria for admission to the examination. Candidates should refer to the specific subspecialty eligibility criteria for details.) The role of the program director in the certification process is to verify completion of training, evaluate clinical competence including professionalism, and provide evidence of the trainee's meaningful accomplishment in research or scholarly activity. An applicant must have the Verification Form(s) on file at the ABP in order to be admitted to the subspecialty examination. If an applicant's training is not verified or if the applicant receives an unsatisfactory evaluation in any of the competences (with the exception of professionalism alone), the applicant will be required to complete an additional period of subspecialty fellowship training before reapplying. The director of the program where the additional training occurred must complete a separate Verification of Competence Form. If the unsatisfactory evaluation is in professionalism only, the applicant will be required to complete an additional period of fellowship training or, at the program director's recommendation and at the ABP's discretion, a period of observation may be required in lieu of additional training. A plan for remediation must be submitted for review and approval by the ABP. The specific requirements for each rotation are found under Core Curriculum (Orientation booklet). The guidelines for procedure numbers are also included in the section (Training Requirements JACC 46:1380, 2005).