Notes - Austin Community College
advertisement

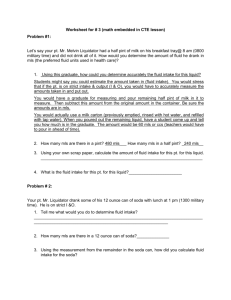
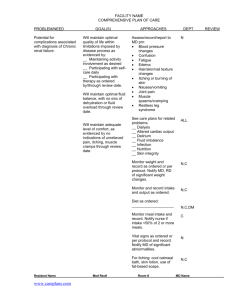
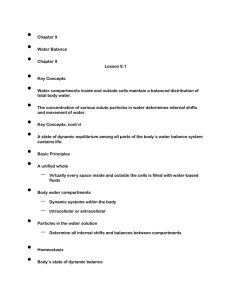
Notes Intake and Output / Height and Weight Intake and Output: Intake and output and a record of the patient’s daily weight are valuable in diagnosing fluid and electrolyte imbalances and in calculating fluid replacement needs easily. Patients who are rapidly losing weight are losing body fluid; patients who are rapidly gaining weight are retaining fluid. Generally, intake and output are measured for at-risk patient’s. Patient’s who are at-risk for fluid and electrolyte imbalances include those: dependent on other to meet their food and fluid needs (elderly, handicapped), NPO with intravenous infusions with severe trauma or burns, chronic diseases such as congestive heart failure, diabetes, cancer postoperative patients on diuretics with special drainages or nasogastric suction The doctor usually orders I&0, but a nurse may initiate I&O as a nursing order if the need is indicated. Measuring Intake and Output: The unit used to measure intake and output is the milliliter (ml). To measure fluid intake, nurses must convert household measures such as a glass, cup, or soup bowl to metric units. In household measures, 30 ml is equivalent to 1 ounce, 500 ml. is about 1 pint, and 1000 ml is about 1 quart. Most agencies provide conversion tables for measurements in their agency. The equipment used to measure I & O are medicine cups, graduated cups and containers, and urine collection devices. The equipment needed for measuring intake and output include: I & O form – place to record amount and time as it actually happens I & O graphic record Graduated glass or cup Bedpan or urinal Urine collection devices (graduated) Nonsterile gloves Sign at bedside stating patient is on I&O. Fluid Intake items: 1. Oral fluids – water, milk, juice, soft drinks, coffee, tea, etc. Include water taken with medications. 2. Ice chips – recorded as ½ the original total amount (ie. 100cc ice = 50cc water. 3. Foods that become liquid at room temperature – ice cream, sherbert, Popsicle, gelatin. Pureed food is not considered fluid intake. 4. Tube feedings – the actual bag or bottle of tube feeding product and be sure to include water used to flush the tube. 5. Parenteral fluids – IV’s, piggybacks, and blood transfusions. Be sure to record “left to counts”, and the amounts from pumps. 6. GU irrigant – irrigation fluids amounts must be documented to ensure that the actual urinary output is determined. Fluid Output Items: 1. 2. 3. 4. 5. Urinary output – following each voiding, pour urine in measuring container, observe amount and time. For those with catheters, be sure to total contents at the end of the shift and empty the bag. A Urimeter measures hourly output and is used with foley catheter bags. If a patient is incontinent of urine, estimate and record these outputs as small, moderate, or large and the number of times pads changed. If a more accurate measurement is required, the pads, towels, etc. can be weighed. Each gram of weight is equal to 1 ml. of urine. Vomit and liquid feces – colostomy bag contents included. Diaphoresis – record number times gown, sheet changed and saturation. Tube drainage – gastric or intestinal. Wound drainage – recorded by type and number of dressing saturated with drainage or by measuring the exact amount from a drainage collected in a vacuum drainage or gravity drainage system. Documentation: Fluid intake and output measurements are totaled at the end of the shift and the totals transferred to a graphic record. In some circumstances in critically ill patients, the totals are recorded hourly. The shift totals are calculated at the end of a 24-hour period. To determine whether the output is proportional to the intake, the nurse compares the 24-hour fluid measurements and also compares them to previous measurements. Patient’s whose output exceeds intake are at risk for fluid volume deficit, and those who intake exceeds output are at risk for fluid volume excess. Causes for Error in measuring Intake and Output: 1. Poor communication among staff concerning which patients are on I&O. 2. Guessing at the measurements rather than actually measuring 3. Failure to estimate losses from perspiration, incontinence, and wound drainage. 4. Failure to measure fluids used in irrigation 5. Failure to explain to the patient and family importance of measuring and to save all output and allow the nurse to measure the amount. 6. Failure to record volumes at the time they are observed. 7. Failure to designate the specific volume of glasses, cups and bowls utilized. Guidelines for Measuring Height and Weight: 1. 2. 3. 4. The patient should be weighed the same time each day using the same equipment and with same clothing on. If daily weights are ordered, the patient is weighed in the early AM. Many times the doctor may order a daily weight to assess fluid loss or gain and not for nutritional purposes. The patient’s height is usually obtained only on admission to the hospital. Shoes should be removed. Procedure for Weighing a mobile patient: 1. Check the patient’s previous weight. 2. 3. 4. 5. 6. 7. Explain procedure to the patient Lock the scale Place the scale near the patient Balance scale at zero. Protect area of patient contact. May need to cover with paper towel. Ask patient to step up on scale and stand still with arms at side and not holding on to anything. 8. Read when balanced. Identify scale being used, electronic or balance and if in pounds or kilograms. 9. Ask the patient to step down 10. Zero the scale when finished. 11. Document correctly. Measuring weight of an immobile patient requires use of a sling scale or a bed scale. Many of the same principles are applied to these methods.