C H A P T E R
advertisement
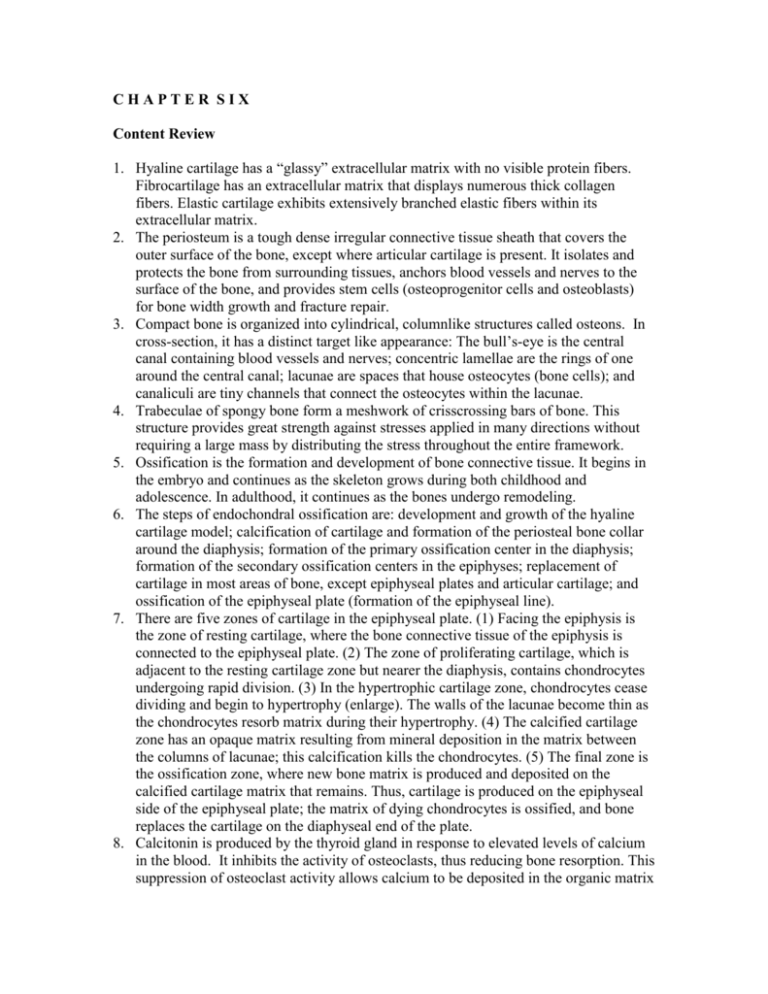
CHAPTER SIX Content Review 1. Hyaline cartilage has a “glassy” extracellular matrix with no visible protein fibers. Fibrocartilage has an extracellular matrix that displays numerous thick collagen fibers. Elastic cartilage exhibits extensively branched elastic fibers within its extracellular matrix. 2. The periosteum is a tough dense irregular connective tissue sheath that covers the outer surface of the bone, except where articular cartilage is present. It isolates and protects the bone from surrounding tissues, anchors blood vessels and nerves to the surface of the bone, and provides stem cells (osteoprogenitor cells and osteoblasts) for bone width growth and fracture repair. 3. Compact bone is organized into cylindrical, columnlike structures called osteons. In cross-section, it has a distinct target like appearance: The bull’s-eye is the central canal containing blood vessels and nerves; concentric lamellae are the rings of one around the central canal; lacunae are spaces that house osteocytes (bone cells); and canaliculi are tiny channels that connect the osteocytes within the lacunae. 4. Trabeculae of spongy bone form a meshwork of crisscrossing bars of bone. This structure provides great strength against stresses applied in many directions without requiring a large mass by distributing the stress throughout the entire framework. 5. Ossification is the formation and development of bone connective tissue. It begins in the embryo and continues as the skeleton grows during both childhood and adolescence. In adulthood, it continues as the bones undergo remodeling. 6. The steps of endochondral ossification are: development and growth of the hyaline cartilage model; calcification of cartilage and formation of the periosteal bone collar around the diaphysis; formation of the primary ossification center in the diaphysis; formation of the secondary ossification centers in the epiphyses; replacement of cartilage in most areas of bone, except epiphyseal plates and articular cartilage; and ossification of the epiphyseal plate (formation of the epiphyseal line). 7. There are five zones of cartilage in the epiphyseal plate. (1) Facing the epiphysis is the zone of resting cartilage, where the bone connective tissue of the epiphysis is connected to the epiphyseal plate. (2) The zone of proliferating cartilage, which is adjacent to the resting cartilage zone but nearer the diaphysis, contains chondrocytes undergoing rapid division. (3) In the hypertrophic cartilage zone, chondrocytes cease dividing and begin to hypertrophy (enlarge). The walls of the lacunae become thin as the chondrocytes resorb matrix during their hypertrophy. (4) The calcified cartilage zone has an opaque matrix resulting from mineral deposition in the matrix between the columns of lacunae; this calcification kills the chondrocytes. (5) The final zone is the ossification zone, where new bone matrix is produced and deposited on the calcified cartilage matrix that remains. Thus, cartilage is produced on the epiphyseal side of the epiphyseal plate; the matrix of dying chondrocytes is ossified, and bone replaces the cartilage on the diaphyseal end of the plate. 8. Calcitonin is produced by the thyroid gland in response to elevated levels of calcium in the blood. It inhibits the activity of osteoclasts, thus reducing bone resorption. This suppression of osteoclast activity allows calcium to be deposited in the organic matrix of bone produced by osteoblasts. Calcitonin also reduces blood calcium levels by increasing the rate of calcium loss in urine. Parathyroid hormone is secreted and released by the parathyroid glands in response to reduced calcium levels in the blood. Its ultimate effect is to increase the blood calcium level by stimulating osteoclasts to resorb bone. Parathyroid hormone also reduces the rate at which calcium is lost in the urine. Finally, parathyroid hormone increases calcium absorption across the lining of the small intestine, so calcium is actively absorbed from ingested food and drink. 9. In response to mechanical stress, bone has the limited ability to increase its strength. Usually, applications of stress strengthen bone tissue over a period of time by increasing the amounts of mineral salts deposited and collagen fibers synthesized. Stress in the form of exercise also increases the production of the hormone calcitonin to help inhibit bone resorption. 10. The steps involved are: (1) fracture hematoma formation; (2) fibrocartilaginous (soft) callus formation; (3) hard (bony) callus formation; and (4) bone remodeling.