Audit of Nutritional Interventions in Low Clearance Clinic
advertisement

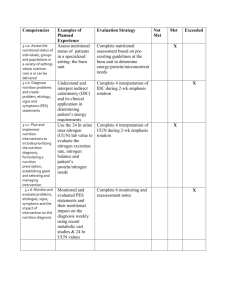
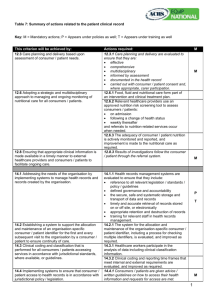
P38 IMPLEMENTATION OF STANDARDS OF DIETETIC CARE IS ASSOCIATED WITH IMPROVED MANAGEMENT OF HIGH NUTRITIONAL RISK PATIENTS IN A SINGLE CENTRE PRE-DIALYSIS CLINIC MacLaughlin, H Department of Nutrition and Dietetics, King’s College Hospital, London BACKGROUND: Recent evidence suggests nutritional status in patients with chronic kidney disease can be improved with the implementation of standards of care or practice guidelines (1). Following an audit revealing gaps in nutritional care and data capture, dietetic service provision increased to the multi-disciplinary pre-dialysis clinic (PDC), electronic documentation was introduced, and the following standards of care were established for renal dietitians in 2006: (a) all patients undergo baseline nutrition assessment and receive dietary education from the dietitian in PDC within 12 weeks (b) all patients undergo 6 monthly nutritional review, and (c) nutritional interventions are implemented as required to prevent or reduce weight loss and malnutrition. The dietetic service was audited to determine if service provision standards were met for all patients who attended the PDC prior to reaching end stage kidney failure requiring renal replacement therapy (RRT) in 2008. METHOD: A retrospective analysis of prospectively collected data for all patients commencing RRT in 2008 was conducted. Analysed data included age, body weight, body mass index (BMI), appetite, and incidence of nutrition assessment and review. Achievement of standards of care was assessed and patients were classified by baseline appetite status, indicating low or high nutritional risk with a good or poor appetite, respectively (2). RESULTS: Of 147 incident RRT patients in 2008, mean (SD) weight 84.7 (19.5) kg, BMI 29.6 (5.5) kg/m2, and age 59.9 (15.9) years, 115 (78%) attended PDC at least once. 104/115 (90%) underwent nutrition assessment, with no difference in weight, BMI or age for patients assessed, or not assessed by the Dietitian. The median (IQR) time to nutrition assessment in PDC was 7 (4-11) weeks and median time to nutritional review was 27 (20-35) weeks. 34/104 (33%) of patients were at high nutritional risk and had significantly more dietetic intervention than patients at low risk, with no significant difference in baseline BMI or % weight change between groups from nutrition assessment to commencement of RRT (Table 1). Table 1: Dietetic interventions, body mass index (BMI) and weight change between nutrition assessment in pre-dialysis clinic and commencement of renal replacement therapy Nutrition assessment to RRT All Good Appetite Poor Appetite P n=104 n=70 n=34 Dietetic interventions/6 months 1.17 1.0 1.4 0.005 (range) (0.3-4.0) (0.3-3.6) (0.5-4.0) BMI at nutrition assessment 29.7 30.0 28.8 0.35 (kg/m2) % weight change - 4.0 - 3.6 - 5.7 0.15 DISCUSSION: Renal dietitians met the standards of care for nutrition assessment, nutritional review and nutritional interventions for patients attending PDC who commenced RRT in 2008. BMI may be a poor indicator of nutritional risk, as BMI did not differ between patients with good and poor appetite. Patients with poor appetite demonstrated no greater weight loss in PDC than those with good appetite, indicating that nutrition assessment and intensive dietetic intervention may have curtailed weight loss and malnutrition in this high risk group. (1) Campbell KL et al. J Ren Nutr. 2009; 19:136-44. (2) Carrero JJ et al. Am J Clin Nutr 2007; 85: 695-701.