ภาวะฉุกเฉินทางอายุรกรรมแยกตามกลุ่มอาการ
advertisement
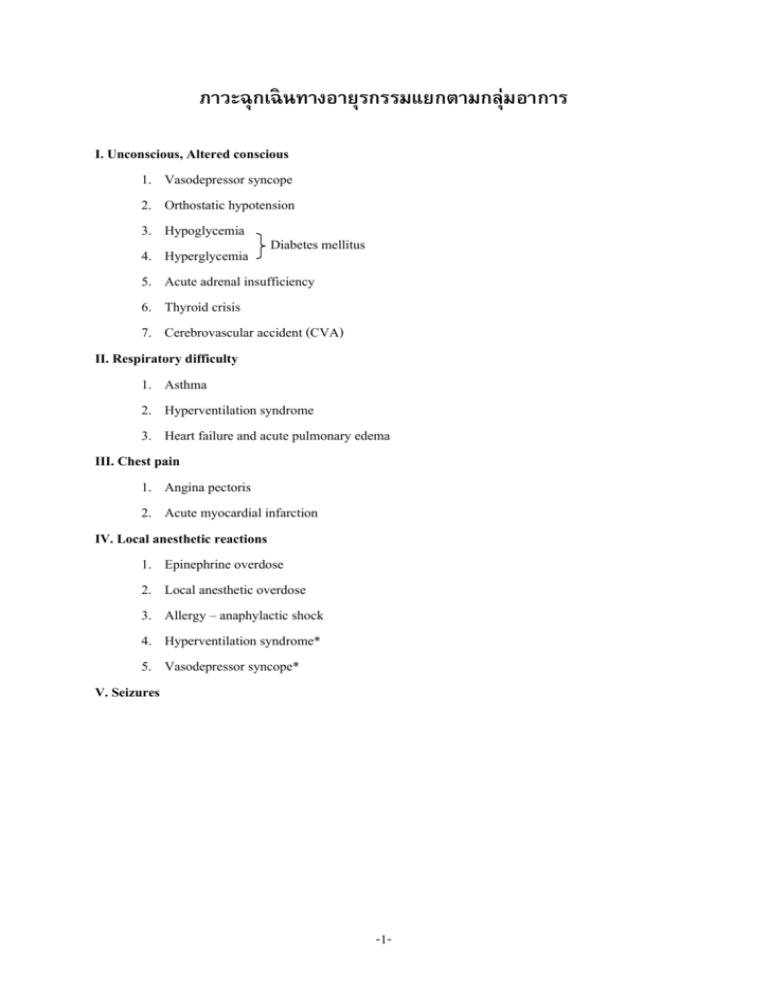
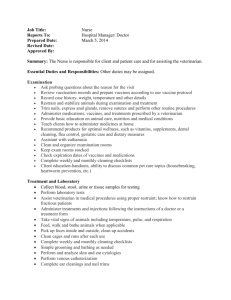
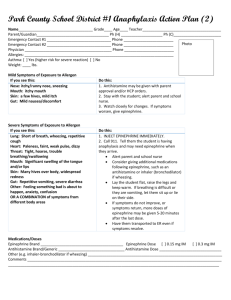
ภาวะฉุกเฉินทางอายุรกรรมแยกตามกลุ่มอาการ I. Unconscious, Altered conscious 1. Vasodepressor syncope 2. Orthostatic hypotension 3. Hypoglycemia Diabetes mellitus 4. Hyperglycemia 5. Acute adrenal insufficiency 6. Thyroid crisis 7. Cerebrovascular accident (CVA) II. Respiratory difficulty 1. Asthma 2. Hyperventilation syndrome 3. Heart failure and acute pulmonary edema III. Chest pain 1. Angina pectoris 2. Acute myocardial infarction IV. Local anesthetic reactions 1. Epinephrine overdose 2. Local anesthetic overdose 3. Allergy – anaphylactic shock 4. Hyperventilation syndrome* 5. Vasodepressor syncope* V. Seizures -1- ภาวะหมดสติ -2- ภาวะเปลี่ยนแปลงการมีสติรบั รู้ -3- ภาวะการหายใจลาบาก -4- ภาวะการเจ็บหน้ าอก -5- ปฏิกิริยาต่อการฉี ดยาชาเฉพาะที่ -6- ปฏิกิริยาต่อการฉี ดยาชาเฉพาะที่ -7- อาการชัก -8- Management of the unconscious patient Step 1 Recognition of unconsciousness “Shake and shout” Painful stimuli Step 2 Call for help Step 3 Position patient Supine position Step 4 Open airway Head tilt – chin lift Step 5 Assess airway patency and breathing Place ear 1 inch from patient’s nose/mouth Hear and feel air from lungs Look at patient’s chest/abdomen See movement of chest/abdomen Step 6 Jaw thrust maneuver (if needed) Dislocation of mandible Tilting head backward Opening mouth with fingers Step 7 Assess airway patency and breathing Place ear 1 inch from patient’s mouth/nose Hear and feel air from lungs Look at patient’s chest/abdomen See movement of chest/abdomen Step 8 Artificial ventilation Exhaled air ventilation (16%) Mouth – to – mouth ventilation Mouth – to – nose ventilation Atmospheric air (21%) Bag – valve – mask units Artificial airways Oropharyngeal Nasopharyngeal S tubes -9- Enriched oxygen (up to 100%) E cylinder with face mask Demand/positive pressure valve Inhalation sedation unit Step 9 Assess circulation Carotid artery (adult/child) Brachial artery (infant) Step 10 Definitive management of unconsciousness Management of vasodepressor syncope Step 1 Place patient in supine position with feet slightly elevated Step 2 Establish patent airway Head tilt – chin lift method Check breathing Jaw thrust maneuver if necessary Recheck breathing if necessary Artificial ventilation if necessary Check circulation Step 3 Monitor vital signs Blood pressure Heart rate Respiratory rate Support patient Ammonia vaporole crushed under nose of patient Cold towel to forehead Blankets if cold or shivering Step 4 Maintain your composure Step 5 Follow – up treatment Determine factors causing unconsciousness Prevent recurrence of vasodepressor syncope Arrange for patient to be taken home by friend or relative No further dental treatment for 24 hours -10- Management of orthotatic hypotension Step 1 Place patient in supine position with feet elevated slightly (at a 10-degree angle) (Note : in late stages of pregnency the lateral position is preferred) Step 2 Maintain airway Head tilt – chin lift Check breathing Jaw thrust maneuver, if necessary Oxygen, if necessary Monitor vital signs Step 3 Make position changes slowly Step 4 Discharge patient Management of acute adrenal insufficiency Conscious patient Step 1 Terminte dental therapy 2 Monitor vital signs 3 Position patient 4 Emergency kit (oxygen) 5 Administer glucocorticosteroid 6 Summon medical assistance Unconscious patient Step 1 Recognize unconsciousness 2 Position patient 3 Basic life support 4 Emergency kit (oxygen) 5 Summon medical assistance 6 Evaluate medical history 7 Administer glucocorticosteroid 7a Additional drugs (vasopressor) 8 Transfer to hospital Management of respiratory difficulty Step 1 Recognition of respiratory difficulty Sounds (wheezing, cough) Abnormal rate and/or depth of respiration Step 2 Terminationof dental procedure -11- Step 3 Position patient, implement basic life support Unconscious – supine position Conscious – upright position usually preferred by patient Step 4 Monitor vital signs Blood pressure, heart rate (pulse) respiratory rate Step 5 Symptomatic management of patient Step 6 Definitive management of respiratory difficulty Management of acute airway obstruction Step 1 Recognition unconsciousness Step 2 Call for help Step 3 Position victim (supine) Step 4 Head tilt Step 5 Assess airway and breathing Step 6 Attempt to ventilate Step 7 Reposition head (head tilt) and attempt to ventilate Step 8 Jaw thrust maneuver Step 9 Attempt to ventilate Step 10 Activate EMS system Step 11 Deliver 6 to 10 abdominal thrusts Step 12 Check mouth for foreign body Step 13 Attempt to ventilate Step 14 Repeat step 11 to 13 until successful Step 15 Cricothyrotomy Management of the hyperventilation syndrome Goals : Reduce anxiety and restore chemical balance of blood 1. Anxiety reduction Step 1 Terminate dental procedure Step 2 Position patient in any comfortable position Step 3 Remove foreign materials from mouth Step 4 Calm patient (latrosedation) -12- 2. Correct respiratory alkalosis Step 5 Breath CO2 –enriched air through brown paper bag, full face mask, or hands cupped over face Step 6 Drug management Diazepam or midazolam IV (titrate) IM (10 mg. Diazepam or 5 mg. Midazolam deeply injected; massage) Oral (10 to 15 mg.) diazepam Step 7 Follow – up Determine cause of anxiety; treat anxiety through psychosedation Note : Oxygen is not indicated for use in the hyperventilation syndrome Management of asthma Step 1 Terminate dental therapy Step 2 Position patient Comportable position Usually sitting with arms thrown forward Step 3 Administer bronchodilator by means of aerosol spray Epinephrine, isopreterenol, or metaproterenol (read instructions carefully before use) Step 4 Administer oxygen Step 5 Parenteral medication If episode continues, epinephrine 1 : 1,000 IM 0.3 ml. (adult); IM 0.125 ml. (infant); IM 0.25 ml. (child) Step 6 Intravenous medications (optional) If episode continues, aminophylline 250 mg. By means of a very slow IV; hydrocortisone sodium succinate, 100 to 200 mg. IV. Step 6a Summon medical assistance if step 6 is needed or if episode is refractory to management Step 7 Regarding further dental therapy: terminate therapy for day Permit patient to recover fully before discharge Management of heart failure and acute pulmonary edema Step 1 Place patient in upright position Step 2 Administer oxygen (nasal cannula preferred) -13- Step 3 Record vital signs Blood pressure Heart rate and thythm Respiratory rate Step 4 Alleviate symptoms of respiratory difficulty Place patient in upright position Bloodliss phlebotomy, rotating toruniquets Step 5 Alleviate apprehension Meperidine 50 mg. IM, or Morphine 10 mg. IM. (for adults) Step 6 Summon medical assistance Management of altered consciousness Step 1 Recognition of altered consciousness Skin Cold and wet Hot and dry Hot with excessive sweating Cold and dry Breath “Acetone” breath Headache, dizziness, confusion Step 2 Terminate dental procedure Step 3 Position patient Conscious – upright position usually preferred by patient Unconscious – supine position If CVA is considered and elevated blood pressure is present, head and thorax should be elevated slightly Step 4 Basic life support Step 5 Monitor vital signs Blood pressure, heart rate (pulse), respiratory rate, and temperature Step 6 Management of signs and symptoms Step 7 Definitive management -14- Hypoglycemia Conscious patient Step 1 Recognition of hypoglycemia Step 2 Assess airway, breathing and circulation and implement as necessary Step 3 Administer oral carbohydrates Step 4 Permit patient to recover Unresponsive conscious patient Step 1 Recognize hypoglycemia Step 2 Assess ABCs. Step 3 Administer oral carbohydrate Step 4 Administer parenteral carbohydrate Step 5 Summon medical assistance Unconscious patient Step 1 Basic life support Step 2 Summon medical assistance Step 3 Definitive management Management of thyroid gland dyfunction Hypofunction or hyperfunction under therapy (euthyroid) Step 1 Manage normally Clinical evidence of hypofunction or hyperfunction Step 1 Prior medical consultation Step 2 Judicious use of durgs CNS – depresants: sedative, narcotic, antianxiety drugs (hypofunction) Atropine and epinephrine (hyperfunction) Unconscious patient Step 1 Basic life support Step 2 Summon medical assistance if no response -15- Management of the patient with hyperglycemia or hypoglycemia Hyperglycemia /diabetic acidosis Hypoglycemia/insulin shock Predisposing factors Onset of symptoms Insulin level Food intake Gardual (days) Insufficient Normal to excessive Sudden (minutes to hours) Excessive May be inadequate Clinical signs and symptoms Skin appearance Mouth Thirst Hunger Vomiting Abdominal pain Respirations Breath odor Blood pressure Heart rate Tremor Convulsions Dry and flushed Dry Intense Absent Common Frequent Exaggerated (Kusmaul) Acetone Low Weak and rapid Absent None Mois and pale Drooling Absent Occasional Rare Absent Normal to shallow Normal Normal Full and bounding Frequent In late stages Gardual Overall – insulin Dental office – basic life support medical assistance Rapid Carbohydrate : oral, IV dextrose (50%), IM glucogon (1 mg.), IM epinephrine (0.5 mg.); (with unconscious patient, provide basic life support, medical assistance and carbohydrate) Management Response to treatment Management -16- Management of CVA Transient ischemic attack Step 1 Terminate dental therapy Step 2 Initiate basic life support Step 3 Manage signs and symptoms Step 4 Monitor vital signs Step 5 Follow – up management Consult with physsician regarding future management Discharge patient with adult companion CVA in the conscious patient Step 1 Terminate dental therapy Step 2 Initiate basic life support Step 3 Manage signs and symptoms Step 4 Monitor vital signs every 5 minutes Step 5 Summon medical assistance after 10 to 15 minutes CVA in the unconscious patient Step 1 Position patient (supine) Step 2 Basic life support Airway Breathing Step 3 Record vital signs CPR if indicated Reposition patient Supine with head elevated slightly in presence of elevated blood pressure or signs of hemorrhagic CVA; supine if CPR is indicated Step 4 Summon medical assistanc eimmediately Note : 1. Any drug with potential for CNS depression should be avoided in the acute CVA patient. 2. Oxygen should be employed in TIA and the conscious CVA patient only in the presence of respiratory difficulty. It may be freely used if unconscioussness is present. -17- Management of tonic-clonic seizures Convulsive (ictal) phase Step 1 Position patient (supine) Step 2 Prevent injury to patient Soft object under head Soft object between teeth, if possible Loosen tight clothing Step 3 Initiate basic life support Step 4 Monitor vital signs Postical phase Step 5 Initiate basic life support Step 6 Permit patient to recover, contact physician Step 7 Discharge patient in company of reponsible adult companion Grand mal status Step 1 Position patient (supine) Step 2 Prevent injury to patient Step 3 Initiate basic life support Step 4 Monitor vital signs Step 5 Administer anticonvulsant drug Diazepam 2 mg./min. slowly and intravenously (for adult) Pentobarbital 25 mg./min slowly and intravenously Step 6 Summon medical assistance Management of Local – anesthetic overdose Mild overdose reaction (rapid onset) No formal therapy Step 1 Reassure patient Step 2 Administer oxygen Step 3 Initiate basic life support Step 4 Monitor vital signs Step 5 Administer anticonvulant (optional) -18- Step 6 Recovery Mild overdose reaction (slow onset) Step 1 Reassure patient Step 2 Administer oxygen and instruct patient to hyperventilate Step 3 Initiate basic life support Step 4 Monitor vital signs Step 5 Venipuncture if available (diazepam 2 mg./min until reaction stops) Step 6 Summon medical assistance Step 7 Medical consultation Step 8 Recovery Severe overdose reaction (rapid onset) Step 1 Position patient (supine) Step 2 Manage seizures Prevent injury Loosen tight graments Step 3 Basic life support Ensure patent airway Administer oxygen Monitor vital signs Step 4 Anticonvulsant after 4 to 5 minutes (diazepam 2 mg./min IV if possible) Manage post seizure depression Airway maintenance Oxygen, artificial ventilation Step 5 Additional management Summon medical assistance Monitor vital signs CPR if indicated Methoxamine, 20 mg. IM for low blood pressure Step 6 Permit patient to recover before discharge to hospital Severe overdose reaction (slow onset) Step 1 Terminate dental therapy Step 2 Basic life support and oxygen -19- Step 3 Anticonvulsant, if symptom progress Step 4 Summon medical assistance Step 5 Manage post seizure depression Basic life support Vasopressor, if necessary Step 6 Permit patient to recover before discharge to hospital Management of epinephrine overdose Step 1 Step 2 Step 3 Step 4 Step 5 Step 6 Terminate dental procedure Position patient – not supine Reassure patient Initiate basic life support Monitor vital signs, administer oxygen Allow patient to recover Management of allergic reactions Skin reaction (delayed) Step 1 Initiate basci life support, as needed Step 2 Antihistamine IM (diphenhydramine 50 mg. Chlorpheniramine 10 mg. and Oral antihistamine) Step 3 Medical consultation Skin reactions (immediate) Step 1 Initiate basic life support, as needed Step 2 Epinephrine 0.125 – 0.3 ml. of 1 : 1,000 IM. SC Step 3 Antihistamine IM Step 4 Consult with physician Step 5 Observe patient Step 6 Oral antihistamine Respiratory reaction – bronchial constriction Step 1 Terminate dental therapy Step 2 Position patient (semierect) Step 3 Initiate basic life support as needed Step 4 Administer oxygen -20- Step 5 Epinephrine via aerosol inhaler or 0.125 –0.3 ml. of 1 : 1,000 IM. SC Step 6 Observe patient Step 7 Antihistamine IM or IV Step 8 Medical consultation Step 9 Oral antihistamine Respiratory reaction – laryngeal edema (partial obstruction) Step 1 Position patient (supine) Step 2 Epinephrine 0.125 – 0.3 ml. of 1 : 1,000 IM. SC. Step 3 Airway maintenance (head tilt) Step 4 Summon medical assistance Step 5 Additional drug therapy anthistamine and corticosteroid IM or IV Laryngeal edema (total obstruction) Step 1 Position patient (supine) Step 2 Epinephrine 0.125 – 0.3 ml. of 1 : 1,000 IM. SC Step 3 Oxygen Step 4 Summon medical assistance Step 5 Antihistamine and corticosteroid IM or IV Step 6 Cricothyrotomy (if needed) Step 7 Transfer to hospital Generalized anaphylaxis (if allergy symptoms appear) Step 1 Position patient (supine) Step 2 Initate basic life support Step 3 Epinephrine 0.125 – 0.3 ml. of 1 : 1,000 IM. SC Step 4 Summon medical assistance Step 5 Monitor vital signs every 5 minutes Step 6 Additional drug therapy antihistamine and corticosteroid IM or IV Step 7 Transfer to hospital Generalized anaphylaxis (no signs of allergy present) Step 1 Position patient (supine) Step 2 Initiate basic life support Step 3 Monitor vital signs every 5 minutes Step 4 Summon medical assistance -21- Dental therapy consideration in angina pectoris Frequency of angina 0-1 per month Patient’s abilities ASA physical status Considerations Patient can walk two level city blocks or climb one flight of stairs Patient can walk two level city blocks or clime one flight of stairs II Usual ASA II considerations and supplemental oxygen II Pain develops before patient walks two level city blocks or climbs one flight of stairs III Daily apisodes or recent (within Patient unable to walk two level past 2-3 weeks) changes in city blocks or climb one flight character of episode : of stairs Increased frequenecy, duration or severity Radiation to new site Precipitated by less acitivity Decreased pain relief with usual nitroglycerin dose IV Usual ASA II considerations to include possible premedication with nitroglycerin 5 minutes before therapy and supplemental oxygen Usual ASA III consideration to include possible premedication with nitroglycerin 5 minutes before therapy and supplemental oxygen Usual ASA IV considerations 2-4 per month 2-3 per week -22- Management of angina Step 1 Terminate dental therapy Step 2 Position patient (upright position most comfortable) Step 3 Administer vasodilator Nitroglycerin preferred Step 4 Amyl nitrite, if needed Nifedipine, if needed Step 5 Other medications Oxygen, if needed Narcotics contraindicated in angina Step 6 Modify further dental therapy to prevent recurrence Management of acute myocardial infarction Step 1 Diagnosis Administer nitroglycerin Step 2 Initiate basic life support and implement as needed Step 3 Summon medical assistance Step 4 Administer oxygen and monitor vital signs Step 5 Relieve pain SC or IV morphine or meperidine or a nitrous oxide – oxygen mixture by means of a nasal hood Step 6 Manage complications Dysrhythmias : Do not administer antidysrhythmic agents unless electrocardioscope is present Congestive heart failure see Cardiac arrest see Step 7 Transport patient to hospital, doctor should accompany patient to hospital -23- ขนาดและวิธีการบริหารยาที่ใช้ในภาวะฉุกเฉิน -24- ขนาดและวิธีการบริหารยาที่ใช้ในภาวะฉุกเฉิน (ต่อ) -25- ขนาดและวิธีการบริหารยาที่ใช้ในภาวะฉุกเฉิน (ต่อ) -26- -27-