File
advertisement

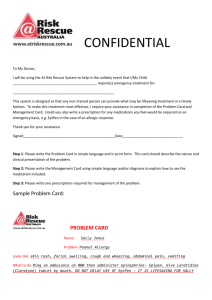
UNIT PROJECT It only takes one anaphylactic reaction to realize that you need to have emergency medications close at hand. IV contrast reactions can vary from mild to severe and life threatening. The incidence of contrast reactions in Radiology are as follows: 3% of patients receiving contrast will have a reaction and require no treatment. 0.4% of patients receiving contrast will have a moderate reaction and require treatment. 0.04% of patients receiving contrast will experience a severe (life-threatening) reaction. (Duncan, K. (December 6, 2012). Webinar, Anaphylaxis What’s Going On?). Although anaphylactic reactions are rare, it can be deadly when it does happen. We had a very serious contrast reaction in CT that resulted in anaphylaxis. Luckily the patient did go home. A patient that had a known contrast reaction had been premedicated with the standard thirteen hour prep, which includes Prednisone and Benadryl. Patients who are at higher risk include those with past reactions to contrast media (up to 44%); those with asthma; those who have a history of heart and kidney and thyroid (both hypo- and hyperthyroidism) diseases; those taking beta – blockers or metformin; and females and the elderly (appear to be at higher risk for severe reactions). (Center LM. Anaphylactoid reactions to radiocontrast media. Allergy Asthma Proc. 2005;209:189-192.) (Keller DM, Iodinated contrast media raises risk of thyroid dysfunction. Arch Intern Med. 2012;172:153-159) Immediately after the scan the patient was itching and had a rash. The patient was deteriorating quickly. The patient went into respiratory arrest and the nurse began respiratory support. The physician ordered Epinephrine (EPI) and the CT techs did not know exactly what the physician wanted. After this event is when Dr. Restauri and I realized that we needed an easier and faster way to get to EPI in an urgent situation. I mentioned to Dr. Restauri that at my previous hospital, we had an emergency box in every room on the wall. The one thing that Dr. Restauri insisted upon in this box was an EpiPen. Not only is it easily accessible but it is also premeasured. In an emergent situation, this saves critical time and prevents errors. However, getting approval for the EpiPen took some work. It is expensive and would not be used often. It is one of those times when if you have it you will not need it but if you do not have it you will need it. It took months of attending the Radiology Quality meetings, Resuscitative Committee and then P & T. The Resuscitative Committee wanted the box to mimic the box in Interventional Radiology with the exception of the EpiPen. We developed an algorithm for responding to contrast reactions (attachment #1) as well as a pocket card (attachment #2) that the physicians could carry around as a reference. We were also published in the Journal of American College of Radiology (JACR) (attachment #3). This was just the beginning of a process to get the anaphylactic boxes in use. I had to have the boxes made for us and order the meds through the Pharmacy. There was a lot of leg work, back and forth e-mails, training of the physicians and staff and the implementation of hanging and stocking the boxes. We had to get posters made and the pocket cards. I also had to create a guideline for checking and exchanging of the box and the contents along with a checklist to check the box daily to make sure that the lock had not been tampered with and the contents had not been compromised. Medications would have to been exchanged as they expired so a monthly examination of the box is required. I had created a guideline for the checking and exchanging of the emergency boxes, however, Andrew Davis of Pharmacy had incorporated it into the Policy and Procedure of all the tackle boxes in the hospital. Our box is officially called Turbo Tackle Box for Radiology. I had noticed that when we called a radiologist to a reaction it took them too long to respond and then asked us what needed to be done for the patient. Before we were able to hang the boxes we had to make sure the physicians had been trained in the availability and use of the boxes. The next step was to provide baseline training for the residents and fellows to determine their level of comfort and knowledge in responding to these emergencies. We used simulation to train the physicians on the emergency box and algorithm for responding to contrast reactions. We conducted a mock contrast reaction at the WELLS Center. My role along with Dr. Restauri was to instruct them on what the scenario was. I was responsible for recording the mock reaction scenario, being the person on the other line, when the nurse in the mock scenario called for respiratory, IV team and code team. I also timed the physicians and recorded how long it took them to request Epi once they responded. After the mock contrast reaction training took place, Dr. Restauri, Dr. Subelong and I would debrief the physicians on what they liked about the training. We offered feedback on what went right and what we needed improvement on. After the debriefing, I then was the one to train them on the use of the EpiPen and record how well they did at performing administering the EpiPen. I have noticed that they respond much quicker and that they are much more knowledgeable and comfortable as evidenced by the way they communicate with the nurses and the patients. Since the opening of a satellite clinic with radiology services, I have had to expand the guideline to this clinic. I have developed an algorithm that is more conducive to a free standing, radiology clinic without hospital resources (Attachment #4). They did not want the emergency boxes on the wall with all of the medications in it. They only wanted the EpiPen. Some of the physicians have been trained on the use of the EpiPen and how to respond to contrast reactions. I have created a power point presentation which includes written and video instruction on how to use the EpiPen. I am waiting on approval. Once this is approved it will be rolled out to the other physicians at the Lone Tree facility. This will be the standard for all free standing, satellite facilities. Of course since these boxes have been in place, we have not had a reaction that has required us to access them. Dr. Restauri and I will continue to provide training for the physicians and staff as needed. Our goal is to purchase our own mannequin so that we can do the training in the AOP. Even though we have not had to access the emergency boxes, it is very noticeable that the residents and fellows are quicker to respond and have more confidence. As you will notice in their evaluations of the training course, they feel more comfortable and have more confidence in responding to these types of emergencies. The monitoring of the effectiveness of these boxes will be an ongoing project to determine if they will help to save lives. We will continue to have contrast reactions and the majority are mild to moderate, however in the case of a patient deteriorating to the point that a code situation is imminent, I truly believe that these boxes will be effective in preventing the situation from progressing to that point. Please see next two downloads for attachments.